Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
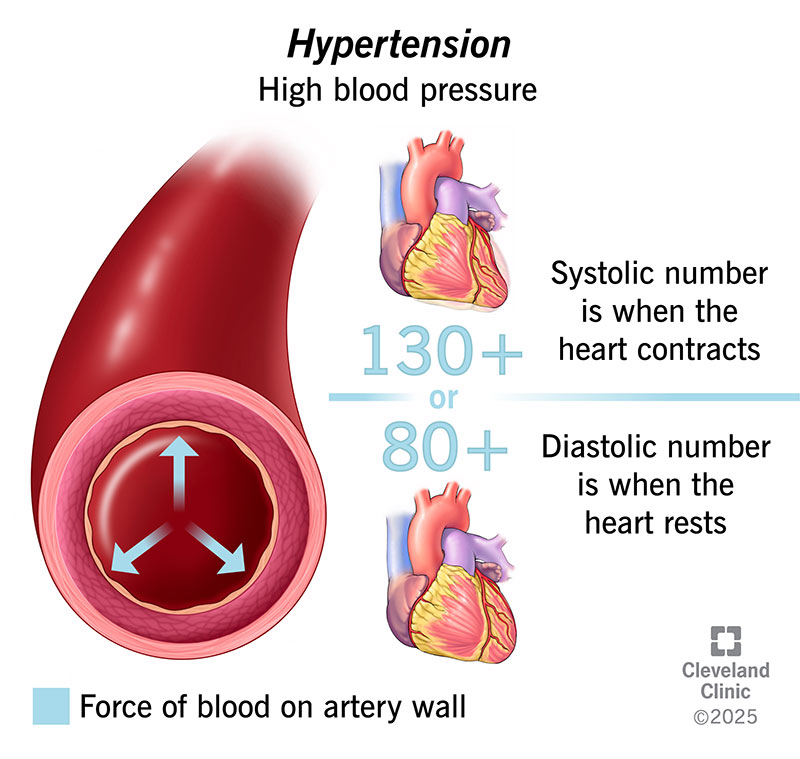
What Causes High Blood Pressure? Common Reasons, Risk Factors & Hidden Causes Explained
High blood pressure (**hypertension**) develops when the force of blood pushing against artery walls stays too high over time. It usually results from a **combination of causes and risk factors**, not a single reason. --- ## 🔹 Main Causes of High Blood Pressure ### 1️⃣ **Primary (Essential) Hypertension** – *Most common* * No single identifiable cause * Develops gradually over years * Strongly linked to lifestyle and genetics --- ### 2️⃣ **Secondary Hypertension** – *Due to an underlying condition* Caused by a specific medical problem and often appears suddenly. **Common causes include:** * **Kidney disease** (CKD, renal artery stenosis) * **Hormonal disorders** * Hyperaldosteronism * Cushing syndrome * Pheochromocytoma * Thyroid disorders * **Obstructive sleep apnea** * **Pregnancy-related hypertension** * **Certain medications** * NSAIDs * Oral contraceptives * Steroids * Decongestants --- ## 🔹 Major Risk Factors ### 🧬 **Non-modifiable** * Family history (genetics) * Increasing age * Male sex (younger age), females (post-menopause) ### 🧂 **Modifiable (Lifestyle-related)** * High salt (sodium) intake * Obesity and overweight * Physical inactivity * Excess alcohol intake * Smoking * Chronic stress * Poor sleep --- ## 🔹 How These Factors Raise Blood Pressure * **Narrowing of blood vessels** → increased resistance * **Increased blood volume** (salt & fluid retention) * **Overactive sympathetic nervous system** * **Hormonal imbalance** (RAAS activation) --- ## 🔹 Key Takeaway > **High blood pressure is usually caused by long-term lifestyle factors combined with genetic susceptibility, but sometimes it is a warning sign of another disease.** --- If you want, I can also provide: * ✅ **Causes by age group** * ✅ **Flowchart of hypertension pathophysiology** * ✅ **Difference between primary vs secondary hypertension** * ✅ **When to suspect secondary hypertension** Just tell me 👍
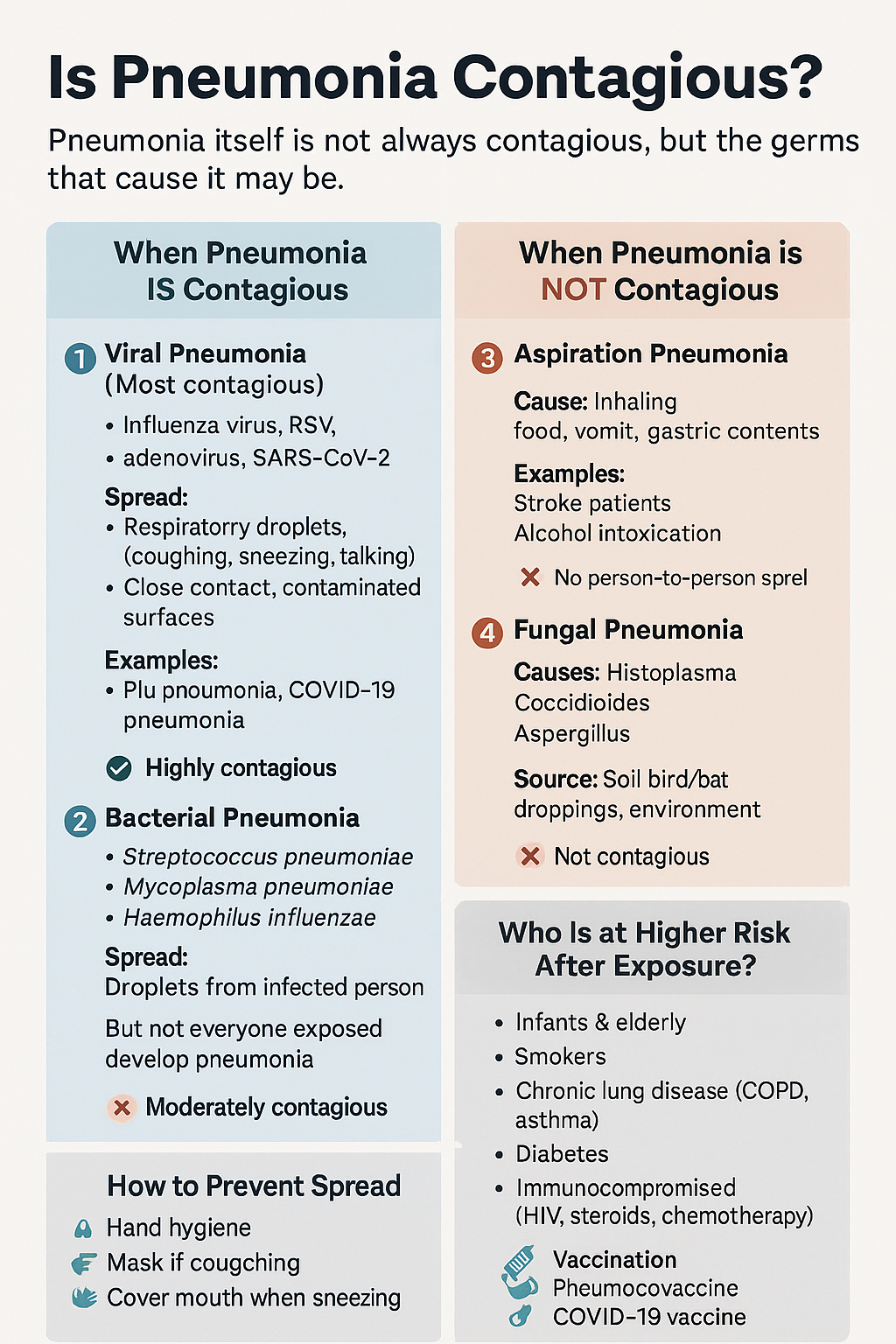
Is Pneumonia Contagious? Causes, Transmission, Types, Risk Factors & Prevention Explained
Below is a **detailed, SEO-ready explanation of pneumonia contagion**, written so you can **directly use it on your medical website** and **add internal links to related posts/pages** (topics commonly present in your medical hub). --- # Is Pneumonia Contagious? Causes, Spread, Risk Factors & Prevention (Complete Guide) ## 🔍 Overview **Pneumonia is an infection of the lung parenchyma** causing inflammation of alveoli with fluid or pus accumulation. Whether pneumonia is **contagious or not depends entirely on its cause**, not on the condition itself. 👉 *(Internal link idea: **What is Pneumonia? – Definition, Types & Pathophysiology**)* --- ## 🦠 Is Pneumonia Contagious? ### **Short answer:** ✔️ **Sometimes yes** ❌ **Sometimes no** The **microorganism causing pneumonia may spread**, but **pneumonia as a disease does not directly transmit**. --- ## 1️⃣ Viral Pneumonia (Highly Contagious) **Most common contagious form** ### Common Causes * Influenza virus * Respiratory Syncytial Virus (RSV) * Adenovirus * SARS-CoV-2 (COVID-19) 👉 *(Internal link: **Viral Pneumonia – Causes, Symptoms & Treatment**)* ### Mode of Spread * Respiratory droplets (coughing, sneezing, talking) * Close personal contact * Contaminated surfaces ### Contagious Period * **1–2 days before symptoms** * **5–7 days after symptom onset** * Longer in children and immunocompromised patients ### Key Point > Viral pneumonia spreads easily, especially in **crowded places, households, and hospitals**. --- ## 2️⃣ Bacterial Pneumonia (Moderately Contagious) ### Common Causes * *Streptococcus pneumoniae* * *Haemophilus influenzae* * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* 👉 *(Internal link: **Bacterial Pneumonia – Diagnosis & Antibiotic Management**)* ### Spread * Respiratory droplets * Close contact with infected person ⚠️ **Important:** You may catch the bacteria, but **only susceptible individuals develop pneumonia**. ### After Treatment * **Not contagious after 24–48 hours of effective antibiotics** --- ## 3️⃣ Aspiration Pneumonia (Not Contagious) ### Cause * Inhalation of: * Food particles * Vomit * Gastric acid * Oropharyngeal secretions 👉 *(Internal link: **Aspiration Pneumonia – Risk Factors & Prevention**)* ### Common in * Stroke patients * Alcohol intoxication * Elderly with swallowing disorders * ICU patients ❌ **No person-to-person spread** --- ## 4️⃣ Fungal Pneumonia (Not Contagious) ### Causes * *Histoplasma* * *Coccidioides* * *Aspergillus* 👉 *(Internal link: **Fungal Lung Infections – Clinical Features & Treatment**)* ### Transmission * Inhalation of spores from: * Soil * Bird or bat droppings * ❌ **No human-to-human transmission** --- ## 👥 Who Is More Likely to Get Pneumonia After Exposure? * Infants & elderly * Smokers * COPD or asthma patients * Diabetes mellitus * Immunocompromised (HIV, chemotherapy, steroids) 👉 *(Internal link: **Risk Factors for Severe Pneumonia**)* --- ## 🛡️ How to Prevent Spread of Contagious Pneumonia * Hand hygiene 🧼 * Mask use during respiratory illness 😷 * Cover mouth while coughing/sneezing * Avoid close contact during active infection * Vaccination: * **Influenza vaccine** * **Pneumococcal vaccine** * **COVID-19 vaccine** 👉 *(Internal link: **Vaccines That Prevent Pneumonia**)* --- ## 🧠 Key Takeaway > **Pneumonia is contagious only when caused by infectious agents like viruses or bacteria.** > Aspiration and fungal pneumonias **do not spread from person to person**. --- ## 🔗 Suggested Internal Linking Structure (SEO Boost) Use internal links to: * Pneumonia Types * Viral vs Bacterial Pneumonia * Pneumonia Symptoms * Pneumonia Diagnosis * Pneumonia Treatment Guidelines * Pneumonia Complications * Pneumonia Prevention & Vaccination This improves **topical authority**, **crawl depth**, and **search ranking**. --- If you want, I can next: * Add **HTML internal link anchors** for your site * Create **schema-ready medical content** * Generate **SEO title, meta description & keywords** * Convert this into **exam-oriented notes or patient-friendly version** Just tell me what you want next 👍
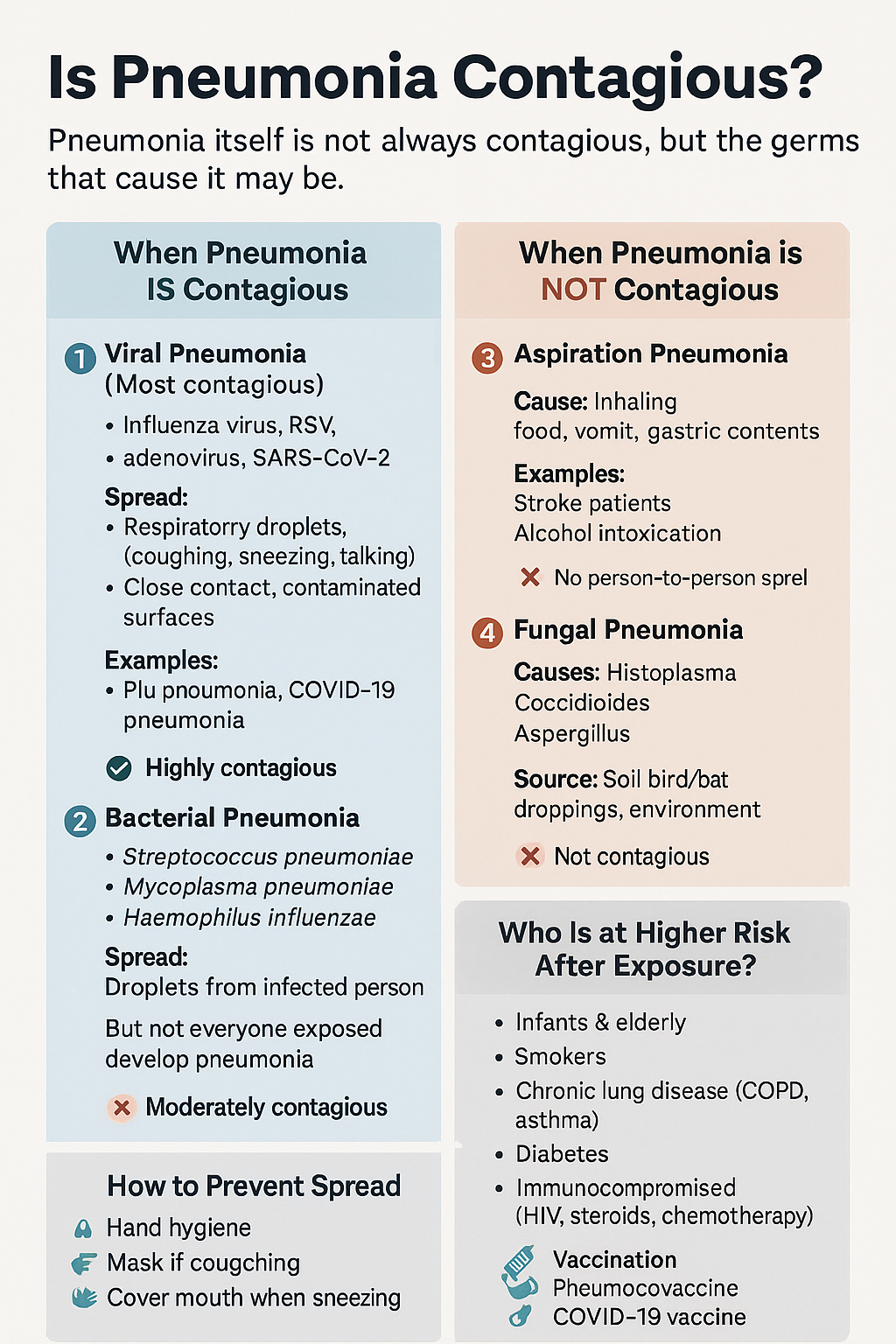
Is Pneumonia Contagious? Causes, Transmission, Types, Risk Factors & Prevention Explained
Below is a **detailed, SEO-ready explanation of pneumonia contagion**, written so you can **directly use it on your medical website** and **add internal links to related posts/pages** (topics commonly present in your medical hub). --- # Is Pneumonia Contagious? Causes, Spread, Risk Factors & Prevention (Complete Guide) ## 🔍 Overview **Pneumonia is an infection of the lung parenchyma** causing inflammation of alveoli with fluid or pus accumulation. Whether pneumonia is **contagious or not depends entirely on its cause**, not on the condition itself. 👉 *(Internal link idea: **What is Pneumonia? – Definition, Types & Pathophysiology**)* --- ## 🦠 Is Pneumonia Contagious? ### **Short answer:** ✔️ **Sometimes yes** ❌ **Sometimes no** The **microorganism causing pneumonia may spread**, but **pneumonia as a disease does not directly transmit**. --- ## 1️⃣ Viral Pneumonia (Highly Contagious) **Most common contagious form** ### Common Causes * Influenza virus * Respiratory Syncytial Virus (RSV) * Adenovirus * SARS-CoV-2 (COVID-19) 👉 *(Internal link: **Viral Pneumonia – Causes, Symptoms & Treatment**)* ### Mode of Spread * Respiratory droplets (coughing, sneezing, talking) * Close personal contact * Contaminated surfaces ### Contagious Period * **1–2 days before symptoms** * **5–7 days after symptom onset** * Longer in children and immunocompromised patients ### Key Point > Viral pneumonia spreads easily, especially in **crowded places, households, and hospitals**. --- ## 2️⃣ Bacterial Pneumonia (Moderately Contagious) ### Common Causes * *Streptococcus pneumoniae* * *Haemophilus influenzae* * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* 👉 *(Internal link: **Bacterial Pneumonia – Diagnosis & Antibiotic Management**)* ### Spread * Respiratory droplets * Close contact with infected person ⚠️ **Important:** You may catch the bacteria, but **only susceptible individuals develop pneumonia**. ### After Treatment * **Not contagious after 24–48 hours of effective antibiotics** --- ## 3️⃣ Aspiration Pneumonia (Not Contagious) ### Cause * Inhalation of: * Food particles * Vomit * Gastric acid * Oropharyngeal secretions 👉 *(Internal link: **Aspiration Pneumonia – Risk Factors & Prevention**)* ### Common in * Stroke patients * Alcohol intoxication * Elderly with swallowing disorders * ICU patients ❌ **No person-to-person spread** --- ## 4️⃣ Fungal Pneumonia (Not Contagious) ### Causes * *Histoplasma* * *Coccidioides* * *Aspergillus* 👉 *(Internal link: **Fungal Lung Infections – Clinical Features & Treatment**)* ### Transmission * Inhalation of spores from: * Soil * Bird or bat droppings * ❌ **No human-to-human transmission** --- ## 👥 Who Is More Likely to Get Pneumonia After Exposure? * Infants & elderly * Smokers * COPD or asthma patients * Diabetes mellitus * Immunocompromised (HIV, chemotherapy, steroids) 👉 *(Internal link: **Risk Factors for Severe Pneumonia**)* --- ## 🛡️ How to Prevent Spread of Contagious Pneumonia * Hand hygiene 🧼 * Mask use during respiratory illness 😷 * Cover mouth while coughing/sneezing * Avoid close contact during active infection * Vaccination: * **Influenza vaccine** * **Pneumococcal vaccine** * **COVID-19 vaccine** 👉 *(Internal link: **Vaccines That Prevent Pneumonia**)* --- ## 🧠 Key Takeaway > **Pneumonia is contagious only when caused by infectious agents like viruses or bacteria.** > Aspiration and fungal pneumonias **do not spread from person to person**. --- ## 🔗 Suggested Internal Linking Structure (SEO Boost) Use internal links to: * Pneumonia Types * Viral vs Bacterial Pneumonia * Pneumonia Symptoms * Pneumonia Diagnosis * Pneumonia Treatment Guidelines * Pneumonia Complications * Pneumonia Prevention & Vaccination This improves **topical authority**, **crawl depth**, and **search ranking**. --- If you want, I can next: * Add **HTML internal link anchors** for your site * Create **schema-ready medical content** * Generate **SEO title, meta description & keywords** * Convert this into **exam-oriented notes or patient-friendly version** Just tell me what you want next 👍
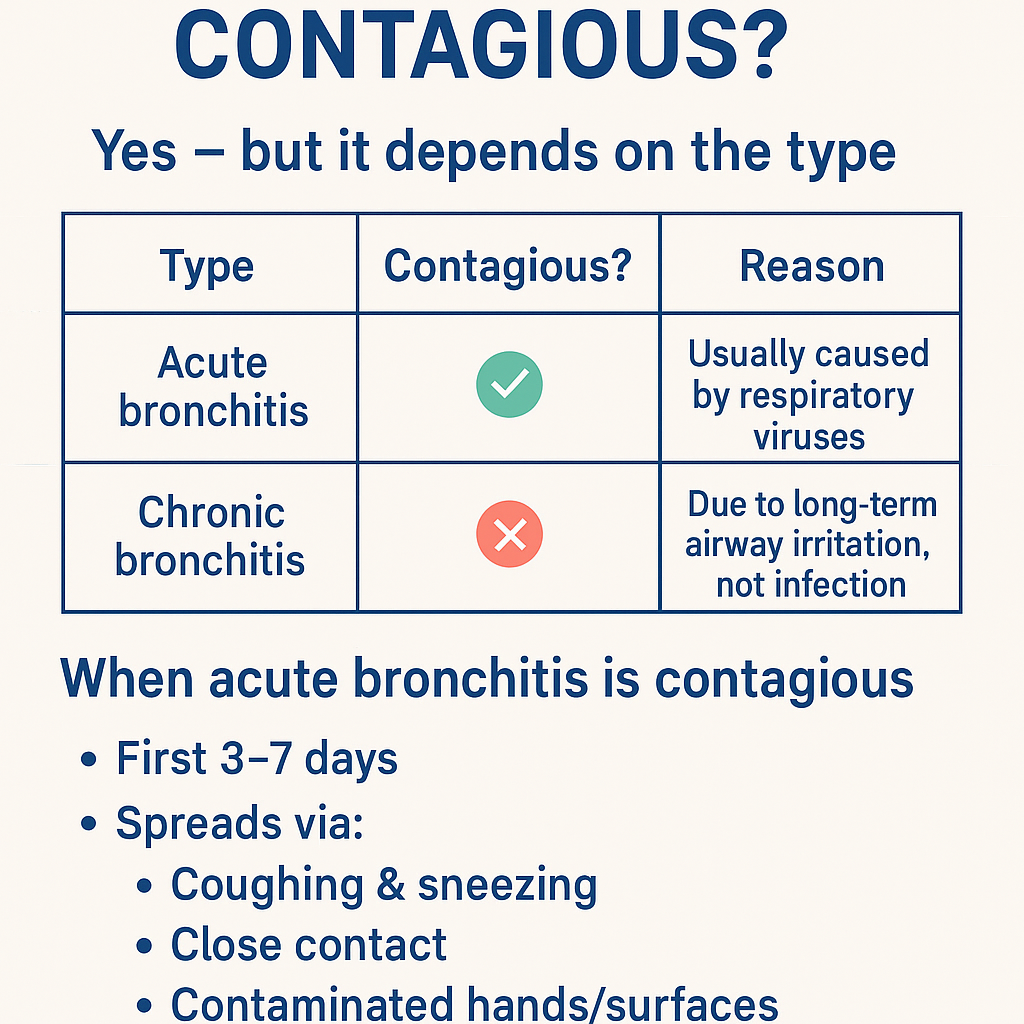
Is bronchitis contagious ? Bronchitis: Causes, Symptoms, Diagnosis, Contagiousness & Complete Treatment Guide (Acute vs Chronic)
Got it 👍 — **no images in chat**. Below is a **complete, concise-but-exhaustive medical reference on BRONCHITIS**, exactly in the structured style you prefer. --- # **Is Bronchitis Contagious?** ### **Yes — but it depends on the type** | Type | Contagious? | Reason | | ---------------------- | ----------- | ----------------------------------------------------- | | **Acute bronchitis** | ✅ **Yes** | Usually caused by **respiratory viruses** | | **Chronic bronchitis** | ❌ **No** | Due to **long-term airway irritation**, not infection | ### **When acute bronchitis is contagious** * First **3–7 days** * Spreads via: * Coughing & sneezing * Close contact * Contaminated hands/surfaces --- # **BRONCHITIS – COMPLETE MEDICAL GUIDE** --- ## **1. Definition** **Bronchitis** is **inflammation of the bronchial tubes**, causing **cough with or without sputum, wheeze, and airflow limitation**. --- ## **2. Classification** ### **A. Acute Bronchitis** * Sudden onset * Duration: **<3 weeks** * Usually **viral** ### **B. Chronic Bronchitis (COPD subtype)** * Productive cough for **≥3 months in 2 consecutive years** * Non-infectious * Progressive disease --- ## **3. Pathophysiology** ### Acute Bronchitis * Viral infection → epithelial injury * Inflammatory mediators → mucosal edema * Increased mucus → impaired ciliary clearance * Transient bronchoconstriction ### Chronic Bronchitis * Chronic irritant exposure → goblet cell hyperplasia * Excess mucus → airway plugging * Reduced ventilation → hypoxia & hypercapnia * Leads to **COPD** --- ## **4. Etiology / Causes** ### **Acute Bronchitis** * **Viruses (≈90%)** * Influenza * Rhinovirus * RSV * Coronavirus * **Atypical bacteria (rare)** * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* * Risk factors: * Smoking * Air pollution * Crowded environments ### **Chronic Bronchitis** * Cigarette smoking (most common) * Biomass fuel exposure * Occupational dust & chemicals * Recurrent infections --- ## **5. Clinical Features** ### **Acute Bronchitis** * Persistent **cough** (dry → productive) * Mucoid or purulent sputum * Low-grade fever * Chest tightness * Wheeze * Mild dyspnea * Malaise, fatigue ### **Chronic Bronchitis** * Daily productive cough * Thick sputum * Dyspnea on exertion * Cyanosis (“blue bloater”) * Peripheral edema (cor pulmonale) * Frequent exacerbations --- ## **6. Investigations** ### Acute Bronchitis * **Clinical diagnosis** * Chest X-ray → only if: * High fever * Tachypnea * Focal chest signs * CBC usually normal ### Chronic Bronchitis * **Spirometry** * ↓ FEV1 * ↓ FEV1/FVC * Chest X-ray: * Increased bronchovascular markings * ABG (advanced): * Hypoxemia * Hypercapnia * Sputum culture (exacerbations) --- ## **7. Differential Diagnosis** * Pneumonia * Asthma * COPD exacerbation * Pulmonary embolism * Tuberculosis (important in India) * Heart failure --- ## **8. Management** --- ## **A. Acute Bronchitis** ### **1️⃣ Non-pharmacological** * Rest * Adequate hydration * Warm fluids * Humidified air * Avoid smoking ### **2️⃣ Pharmacological** #### **Antipyretic / Analgesic** **Paracetamol** * Dose: 500–1000 mg every 6–8 h (max 4 g/day) * MOA: Central COX inhibition * Adverse effects: Hepatotoxicity (overdose) * Counselling: Avoid alcohol excess #### **Bronchodilator (if wheeze)** **Salbutamol** * Dose: 2–4 puffs every 4–6 h * MOA: β2-agonist → bronchodilation * Side effects: Tremor, palpitations * Monitoring: Heart rate #### **Antibiotics** ❌ **NOT routinely indicated** * Use only if: * Suspected bacterial infection * Elderly/comorbid * Prolonged symptoms **Amoxicillin / Azithromycin** (if indicated) --- ## **B. Chronic Bronchitis** ### **1️⃣ Lifestyle** * **Smoking cessation (most important)** * Vaccinations: * Influenza * Pneumococcal ### **2️⃣ Pharmacological** * **Bronchodilators** * SABA / LABA * **Inhaled corticosteroids** (selected patients) * **Mucolytics** * **Antibiotics** during infective exacerbations * **Oxygen therapy** (chronic hypoxemia) --- ## **9. Complications** ### Acute * Secondary pneumonia * Bronchospasm * Prolonged cough ### Chronic * COPD progression * Pulmonary hypertension * Cor pulmonale * Respiratory failure --- ## **10. Prevention** * Hand hygiene * Mask during respiratory infections * Smoking cessation * Avoid air pollution * Vaccinations --- ### **Key Exam Pearls** * Acute bronchitis → **viral, self-limiting** * Green sputum ≠ bacterial infection * Chronic bronchitis = **COPD** * Antibiotics are **not first-line** --- If you want next: * **SEO title, description & keywords** * **Case-based MCQs** * **Flowchart-style management** * **Comparison table: bronchitis vs pneumonia vs asthma** Just tell me ✔️

Rh-Negative Pregnancy: Causes, Risks, Anti-D Prophylaxis, Diagnosis & Complete Management Guide
Below is a **complete, concise-but-exhaustive medical reference** for **Rh-negative pregnancy**, followed by **SEO title, description, keywords**, and an **auto-generated image**. --- # ⭐ **RH-NEGATIVE PREGNANCY — COMPLETE DETAILS**   --- If you want, I can also create: ✅ **25 Hard Case-based MCQs (HTML/CSS/JS exam mode)** ✅ Flowcharts for diagnosis & management ✅ A printable PDF for your Medical Hub app Just tell me!

Liver Disorders in Pregnancy: Causes, Symptoms, Diagnosis & Management | Complete Guide
# **Liver Disorders in Pregnancy — Complete, Exam-Ready Medical Reference** Below is a **single-place, concise but exhaustive** medical summary covering **definition, pathophysiology, causes, clinical features, investigations, differential diagnoses, and full management** of all major liver disorders specific to pregnancy. --- # **1. Classification of Liver Disorders in Pregnancy** ## **A. Disorders Unique to Pregnancy** 1. **Hyperemesis Gravidarum (HG) with hepatic dysfunction** 2. **Intrahepatic Cholestasis of Pregnancy (ICP)** 3. **Pre-eclampsia related liver dysfunction** 4. **HELLP Syndrome** 5. **Acute Fatty Liver of Pregnancy (AFLP)** ## **B. Pre-existing Liver Diseases Aggravated by Pregnancy** * Viral hepatitis (A, B, C, E) * Autoimmune hepatitis * Wilson disease * Cirrhosis/portal hypertension ## **C. Coincidental Liver Disorders** * Gallstones, biliary colic * Acute cholecystitis * Drug-induced hepatotoxicity --- # **2. Hyperemesis Gravidarum (HG)** ### **Definition** Severe nausea/vomiting in early pregnancy → dehydration, ketosis, >5% weight loss, with mild ↑LFTs. ### **Pathophysiology** * High **β-hCG and estrogen** → trigger vomiting center * Starvation → hepatic stress → mild ↑AST/ALT ### **Clinical Features** * Persistent vomiting * Dehydration, tachycardia * Mild jaundice (rare) ### **Investigations** * LFTs: ALT/AST mildly ↑ (usually <300 IU/L) * Electrolytes: ↓K⁺, ↓Na⁺ * Ketonuria ### **Differentials** * ICP * Hepatitis * GI obstruction ### **Management** * IV fluids (NS + thiamine BEFORE dextrose) * Antiemetics: * **Ondansetron** (5-HT₃ antagonist) * **Doxylamine + pyridoxine** * **Metoclopramide** * Manage electrolytes * Rarely hospitalisation + enteral/parenteral feeding --- # **3. Intrahepatic Cholestasis of Pregnancy (ICP)** ### **Definition** Reversible **hormone-triggered cholestasis** in 2nd–3rd trimester → **generalized pruritus**, ↑serum bile acids. ### **Pathophysiology** * Estrogen → ↓bile flow * Genetic factors (ABCB4, ABCB11 mutations) * Accumulation of **bile acids → placental vasoconstriction** ### **Clinical Features** * Severe **itching**, especially palms/soles * No rash * Mild jaundice (10–20%) ### **Investigations** * **Serum bile acids >10–14 µmol/L** = diagnostic * ALT/AST mildly ↑ * Bilirubin normal/slightly ↑ ### **Differentials** * Viral hepatitis * Drug-induced cholestasis * AFLP / HELLP ### **Management** **Maternal** * **Ursodeoxycholic acid (UDCA)**: 10–15 mg/kg/day * Improves bile flow, reduces pruritus * Antihistamines for itch * Vitamin K supplementation if prolonged PT **Fetal** * Weekly NST/BPP * **Delivery at 36–37 weeks** to prevent stillbirth --- # **4. Pre-eclampsia-Related Liver Dysfunction** ### **Mechanism** Generalized endothelial dysfunction → hepatic vasospasm → ischemia → periportal necrosis → ↑LFTs. ### **Features** * Hypertension, proteinuria * RUQ/epigastric pain * Mild ↑AST/ALT (<300 IU/L) ### **Management** * Control BP (labetalol, hydralazine) * Magnesium sulfate for seizure prophylaxis * **Delivery = definitive treatment** --- # **5. HELLP Syndrome** (Hemolysis, Elevated Liver enzymes, Low Platelets) ### **Pathophysiology** Microangiopathic hemolysis + hepatic sinusoidal obstruction → liver ischemia → ↑LFTs + thrombocytopenia. ### **Clinical Features** * RUQ pain * Nausea/vomiting * Hypertension ± proteinuria * Jaundice (mild) ### **Investigations** * AST/ALT ↑ (usually 300–1000 IU/L) * Platelets <100,000 * ↑LDH, ↑bilirubin * Schistocytes on smear ### **Management** * Stabilize mother * Magnesium sulfate * Control BP * **Immediate delivery** (≥34 weeks or earlier if unstable) * Platelet transfusion if <20,000 or surgery needed --- # **6. Acute Fatty Liver of Pregnancy (AFLP)** **Most severe pregnancy-specific liver disorder** ### **Definition** Acute microvesicular fatty infiltration of hepatocytes → **acute liver failure** in 3rd trimester. ### **Pathophysiology** * Mitochondrial **fatty acid oxidation defect** (LCHAD deficiency in fetus) * Maternal inability to metabolize fatty acids → toxic metabolites → hepatic failure ### **Clinical Features** * Prodrome: nausea, vomiting * **Jaundice prominent** * **Hypoglycemia** * **Encephalopathy** * Polyuria/polydipsia (diabetes insipidus-like) * Coagulopathy, DIC ### **Investigations** * AST/ALT moderately ↑ (300–500 IU/L) * **Hypoglycemia** * ↑Ammonia * ↑Bilirubin * **Prolonged PT/INR** * Leukocytosis * US: bright fatty liver (not always) ### **Differentials** * HELLP * Severe hepatitis * Sepsis ### **Management** * **Immediate delivery — life-saving** * ICU care * Manage hypoglycemia (IV dextrose) * Correct coagulopathy (FFP, cryoprecipitate) * Treat encephalopathy (lactulose) --- # **7. Viral Hepatitis in Pregnancy** ### **Key Points** * **Hepatitis E** → highest maternal mortality (up to 20–30%) * Hepatitis B transmission risk highest if HBeAg positive ### **Features** * Markedly raised LFTs * Jaundice * Coagulopathy (severe cases) ### **Management** * Supportive * **Hepatitis B**: give **HBIG + vaccine** to newborn * Avoid ribavirin in pregnancy --- # **8. Gallstone Disease and Acute Cholecystitis** ### **Pathophysiology** Progesterone → biliary stasis Estrogen → ↑cholesterol in bile → gallstones ### **Features** * RUQ pain * Fever (in cholecystitis) * Nausea/vomiting ### **Investigations** * US abdomen: first-line ### **Management** * Pain control * IV antibiotics (cephalosporins safe) * ERCP if choledocholithiasis * Cholecystectomy (2nd trimester safest) --- # **9. Differentiating HELLP vs AFLP vs ICP** | Feature | HELLP | AFLP | ICP | | ---------------- | --------- | --------- | ------------- | | Jaundice | Mild | Prominent | Mild | | Platelets | ↓↓↓ | Mild ↓ | Normal | | Glucose | Normal | **Low** | Normal | | Bile acids | Normal | Normal | **Very high** | | Delivery urgency | Immediate | Immediate | 36–37 weeks | --- # **10. Summary of Management Principles** ### **A. Maternal stabilization** * Correct fluids, electrolytes * Manage coagulation issues * BP control * Seizure prophylaxis where indicated ### **B. Fetal monitoring** * NST, BPP, Doppler * Early delivery if maternal/fetal compromise ### **C. Delivery** * ICP → 36–37 weeks * HELLP/AFLP → **immediate** --- If you want, I can also generate: ✅ **SEO title + description + keywords** ✅ **Stylish HTML/CSS/JS MCQs (hard, case-based)** ✅ **Flowcharts / diagrams** ✅ **An image illustration** Just tell me **what you want next**.
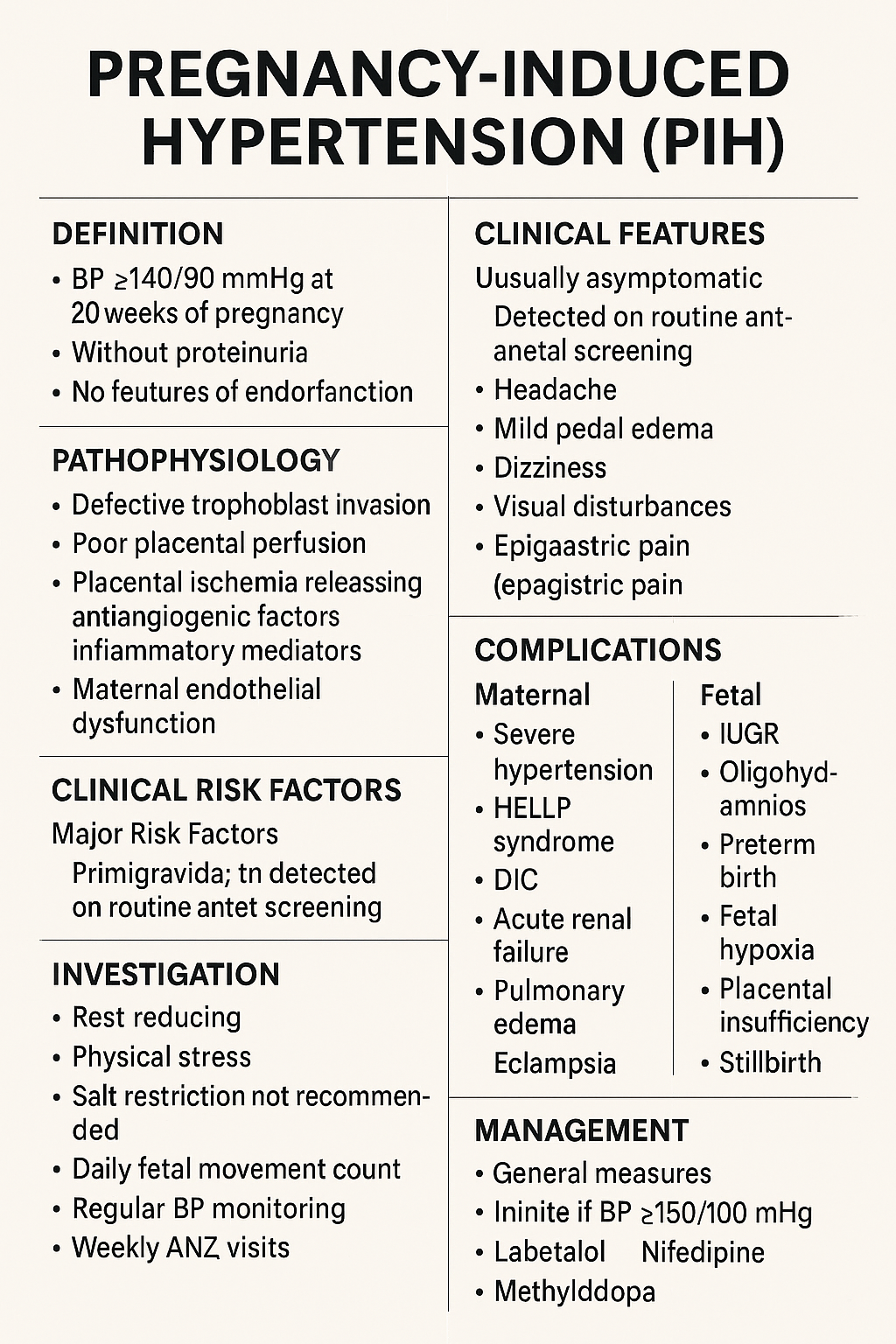
Pregnancy-Induced Hypertension (PIH): Complete Causes, Symptoms, Diagnosis & Treatment Guide
Below is a **complete, concise-but-exhaustive, exam-ready medical reference** on **Pregnancy-Induced Hypertension (PIH)**—also called **gestational hypertension**. Covers: **definition, pathophysiology, etiologies, risk factors, clinical features, investigations, differential diagnosis, complications (maternal & fetal), management (stepwise), drugs with dosing + MOA + AEs + contraindications + monitoring**, delivery timing, prevention, counseling. --- # ⭐ **PREGNANCY-INDUCED HYPERTENSION (PIH) — COMPLETE DETAILS** ! --- # **1️⃣ Definition** **PIH = Gestational Hypertension** * **BP ≥140/90 mmHg** after **20 weeks** of pregnancy * **No proteinuria** * **No features of end-organ dysfunction** * BP becomes normal within **12 weeks postpartum** --- # **2️⃣ Epidemiology** * Occurs in **6–10%** of pregnancies * More common in **primigravida**, **multiple gestation**, **teenage pregnancy**, **advanced maternal age** --- # **3️⃣ Etiology & Risk Factors** ### **Major Risk Factors** * Primigravida * Family history of PIH/Preeclampsia * Personal history of PIH * Multiple pregnancy * Molar pregnancy * Diabetes, Obesity, Chronic hypertension * Autoimmune disease * Renal disease * Thrombophilias * Advanced maternal age (>35 years) --- # **4️⃣ Pathophysiology (Simplified & Complete)**   ### **Normal Pregnancy** * Trophoblast invades → spiral arteries remodel → become wide, low-resistance → good placental perfusion. ### **PIH / Preeclampsia Spectrum** 1. **Defective trophoblastic invasion** → incomplete spiral artery remodeling 2. **Placental ischemia** → oxidative stress 3. **Release of antiangiogenic factors** (sFlt-1, endoglin) and inflammatory mediators 4. **Maternal endothelial dysfunction** → * ↑ vascular resistance * ↑ capillary permeability * Hypercoagulability 🔹 **PIH = mild endotheliopathy without proteinuria or organ dysfunction** 🔹 **Preeclampsia = PIH + proteinuria or organ dysfunction** --- # **5️⃣ Diagnostic Criteria** ### **BP Measurement** * Two readings ≥140/90 mmHg * At least 4 hours apart * After 20 weeks gestation * No proteinuria * No systemic symptoms ### **Proteinuria must be absent** * Dipstick <1+ * Spot urine protein/creatinine ratio <0.3 * 24-hr urinary protein <300 mg --- # **6️⃣ Clinical Features** ### **Usually Asymptomatic** Detected on routine antenatal screening. ### **If symptoms appear** * Headache * Mild pedal edema * Dizziness * Visual disturbances (suggest severe disease progression) * Epigastric pain (danger sign) --- # **7️⃣ Investigations (Complete Panel)** ### **Basic** * BP monitoring * Urinalysis (protein) * CBC * LFTs (AST/ALT) * Renal function test (creatinine, uric acid) ### **For progression to Preeclampsia** * Urine PCR * Peripheral smear (hemolysis) * Coagulation profile * LDH * Fundus examination ### **Fetal Evaluation** * Ultrasound for growth * AFI * Doppler velocimetry * NST / BPP --- # **8️⃣ Differential Diagnosis** * **Chronic hypertension** * **White coat hypertension** * **Preeclampsia** * **Transient hypertension of pregnancy** * **Renal disease** * **Thyroid disorders** * **Drug-induced hypertension** --- # **9️⃣ Maternal Complications** ### **If PIH progresses → Preeclampsia/Eclampsia** * Severe hypertension * HELLP syndrome * DIC * Acute renal failure * Pulmonary edema * Placental abruption * Eclampsia * Stroke / Intracranial hemorrhage --- # **🔟 Fetal Complications** * IUGR * Oligohydramnios * Preterm birth * Fetal hypoxia * Placental insufficiency * Stillbirth --- # **1️⃣1️⃣ Management (Complete Stepwise Protocol)**   --- ## **A. General Measures** * Rest, preferably left lateral * Reduce physical stress * Salt restriction **NOT** recommended severely, only normal diet * Daily fetal movement count * Regular BP monitoring * Weekly ANC visits --- ## **B. Threshold for Treatment** * **Treat if BP ≥150/100 mmHg** * For **140–149/90–99 → Monitor only**, no medication unless comorbidity --- ## **C. First-Line Antihypertensive Drugs in Pregnancy** --- # **🔹1. Labetalol (Drug of Choice)** **MOA:** α-1 & β-blocker → ↓ SVR & BP **Dose:** * Oral: 100–200 mg twice daily → up to 2,400 mg/day * IV (for severe): 20 mg bolus → 40 mg → 80 mg q10min (max 300 mg) **PK:** Hepatic metabolism **Common AEs:** Fatigue, dizziness **Serious AEs:** Bradycardia, hypotension **Contraindications:** Asthma, heart block **Monitoring:** BP, HR **Counselling:** Avoid abrupt stopping --- # **🔹2. Nifedipine (Long-acting)** **MOA:** Calcium channel blocker → vasodilation **Dose:** 30–60 mg sustained-release OD **PK:** Hepatic **Common AEs:** Headache, flushing **Serious AEs:** Hypotension **Contraindications:** Aortic stenosis **Interactions:** Magnesium sulfate ↑ hypotension risk **Monitoring:** BP **Counselling:** Do not chew CR tablets --- # **🔹3. Methyldopa (Safe in pregnancy)** **MOA:** Central α2 agonist **Dose:** 250–500 mg 2–3 times/day **PK:** Renal **Common AEs:** Sedation, depression, dry mouth **Serious AEs:** Liver dysfunction, hemolytic anemia **Monitoring:** LFTs **Counselling:** May cause drowsiness --- # ❌ **Drugs Contraindicated** * ACE inhibitors * ARBs * Atenolol * Diuretics (except pulmonary edema) --- # **1️⃣2️⃣ Management of Severe PIH** * BP ≥160/110 mmHg * Admit * IV labetalol / oral nifedipine * Evaluate for preeclampsia * Magnesium sulfate if criteria for severe features --- # **1️⃣3️⃣ Magnesium Sulfate (for progression to severe/eclampsia)** **MOA:** CNS depressant → prevents seizures by NMDA blockade **Dose (Pritchard):** * 4 g IV loading + 10 g IM (5 g each buttock) * 5 g IM q4h **Monitoring:** * Respiratory rate * Urine output (>30 ml/hr) * Patellar reflex **Toxicity:** Respiratory depression → treat with **10% calcium gluconate 10 ml IV** --- # **1️⃣4️⃣ Delivery Timing** | Condition | Timing | | ------------------------------------------------ | ------------------------- | | **PIH (controlled)** | **37 weeks** | | **Severe PIH** | 34 weeks (after steroids) | | **Uncontrolled BP, fetal compromise, abruption** | Immediate delivery | --- # **1️⃣5️⃣ Intrapartum Care** * Continuous fetal monitoring * Keep BP <160/110 * Avoid fluid overload * Anesthesia: regional preferred unless contraindicated --- # **1️⃣6️⃣ Postpartum Care** * Continue antihypertensives * Monitor BP for **12 weeks** * If persistent → chronic hypertension --- # **1️⃣7️⃣ Prevention of PIH** * Low-dose **Aspirin 75–150 mg at bedtime** from **12–16 weeks** in high-risk women * Calcium supplementation (1–1.5 g/day) in low-calcium diets * Weight control * Control comorbidities --- # **1️⃣8️⃣ Patient Counseling Points** * Regular BP monitoring * Danger signs: headache, visual symptoms, epigastric pain * Adherence to medications * Fetal kick count * Importance of follow-up * No self-discontinuation of drugs --- # ⭐ If you want, I can also provide: ✅ **Flowchart of PIH diagnosis** ✅ **Flowchart of management** ✅ **HTML/CSS/JS quiz (hard, case-based)** ✅ **SEO title + description + keywords** ✅ **Image generation** Just tell me what you need next!
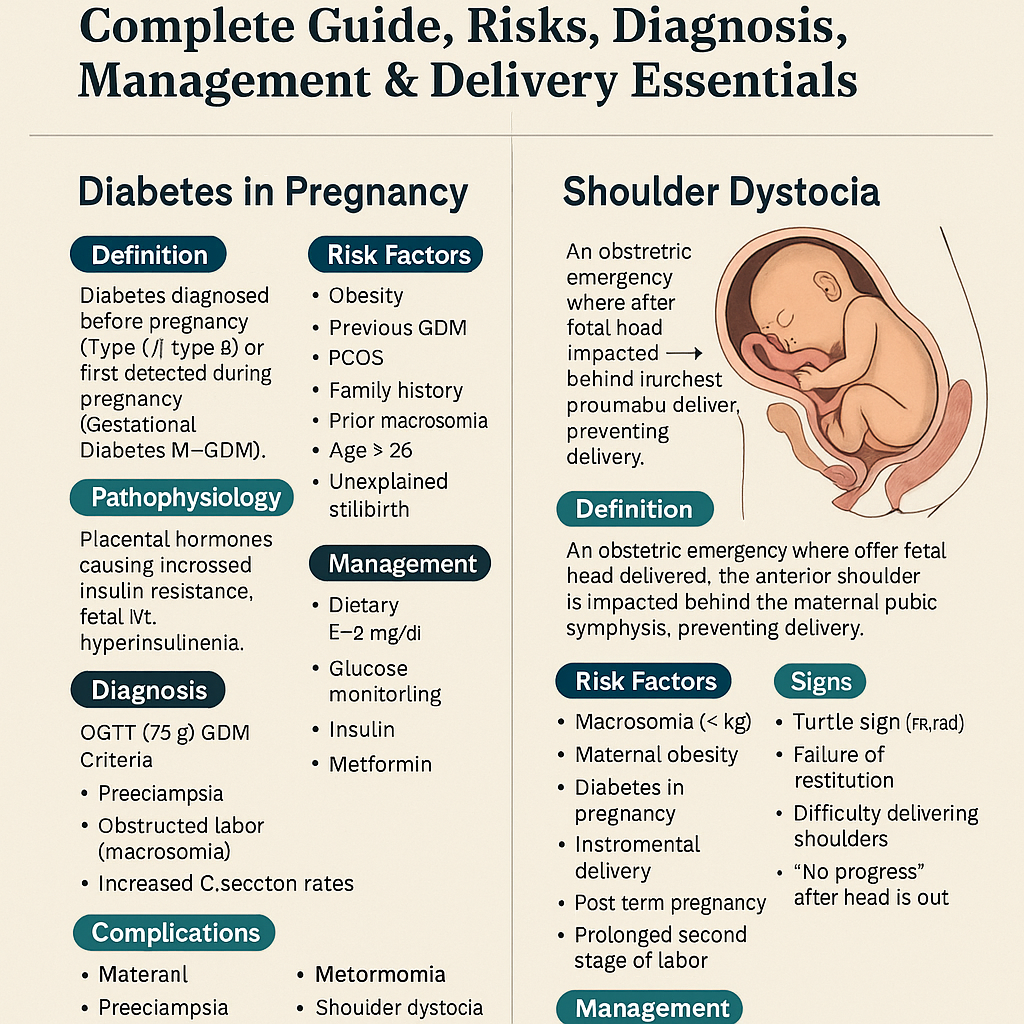
Diabetes in Pregnancy & Shoulder Dystocia – Complete Guide, Risks, Diagnosis, Management & Delivery Essentials
Below is a **stylish, concise-but-complete medical reference** on **Diabetes in Pregnancy** and **Shoulder Dystocia**, written in an exam-ready, high-yield format with clean headings and clinical depth. --- # 🎀 **Diabetes in Pregnancy — Complete Stylish Note** ! ## 🌸 **Definition** Diabetes diagnosed **before pregnancy** (Type 1 / Type 2) or **first detected during pregnancy** (Gestational Diabetes Mellitus – GDM). --- ## 🌸 **Pathophysiology** * Pregnancy → ↑ **Placental hormones** (hPL, progesterone, estrogen, cortisol, TNF-α). * Causes **progressive insulin resistance**, peaking at **24–28 weeks**. * Mother: ↑ post-prandial glucose. * Fetus: Maternal glucose crosses placenta → **fetal hyperinsulinemia** → macrosomia. --- ## 🌸 **Risk Factors** * Obesity * PCOS * Previous GDM * Family history * Age > 25 * Prior macrosomic baby (>4 kg) * Unexplained stillbirth * Acanthosis nigricans --- ## 🌸 **Clinical Features** Often asymptomatic. May show: * Polyuria * Polydipsia * Recurrent infections * Excessive fetal growth on USG --- ## 🌸 **Diagnosis** ### ✔ **Screening (24–28 weeks)** 1️⃣ **DIPSI / WHO one-step test** * 75 g oral glucose, **2 hr ≥ 140 mg/dL = GDM** 2️⃣ **OGTT (75 g) ADA criteria** * Fasting ≥ 92 mg/dL * 1 hr ≥ 180 mg/dL * 2 hr ≥ 153 mg/dL → Any **one** abnormal = GDM. ### ✔ Early pregnancy testing * Fasting ≥126 mg/dL * HbA1c ≥6.5% * RBS ≥200 mg/dL + symptoms → **Overt diabetes in pregnancy**. --- ## 🌸 **Maternal Complications** * Polyhydramnios * Preeclampsia * Preterm labour * Infections * DKA (especially Type 1) * Obstructed labour (macrosomia) * Increased C-section rates --- ## 🌸 **Fetal & Neonatal Complications** * **Macrosomia** (key) * Shoulder dystocia * Congenital anomalies (pre-gestational DM) * Caudal regression syndrome * Cardiac defects * IUGR (if vasculopathy) * IUFD * Neonatal hypoglycemia * Hypocalcemia, hypomagnesemia * RDS * Polycythemia, hyperbilirubinemia --- ## 🌸 **Management** ### **1. Medical Nutrition Therapy** * 3 major + 3 snack meals * Low GI diet * Total calories: * Normal weight: 30 kcal/kg/day * Obese: 25 kcal/kg/day * Underweight: 35–40 kcal/kg/day ### **2. Exercise** * 30 minutes walking after major meals * Avoid supine position ### **3. Glucose Monitoring** * Fasting target: <95 mg/dL * 1 hr PP: <140 mg/dL * 2 hr PP: <120 mg/dL ### **4. Pharmacotherapy** #### **Insulin (preferred)** * Short-acting analogs preferred * Basal–bolus regimen * Safe in pregnancy #### **Metformin** * Used if diet fails * Crosses placenta but considered safe * Not preferred in early organogenesis for overt diabetes ### **5. Fetal Monitoring** * Growth scans every 4 weeks * NST/BPP from 32–34 weeks * Doppler if vasculopathy ### **6. Delivery Timing** * GDM well controlled: **39 weeks** * Poorly controlled / insulin-requiring: **37–38 weeks** * Estimated fetal weight >4.5 kg → consider **elective C-section** --- ## 🌸 **Postpartum** * Insulin needs drop sharply * Reassess glucose at **6–12 weeks postpartum** using 75 g OGTT * Risk of future Type 2 DM → counselling essential --- --- # 🌟 **Shoulder Dystocia — Stylish Complete Note**  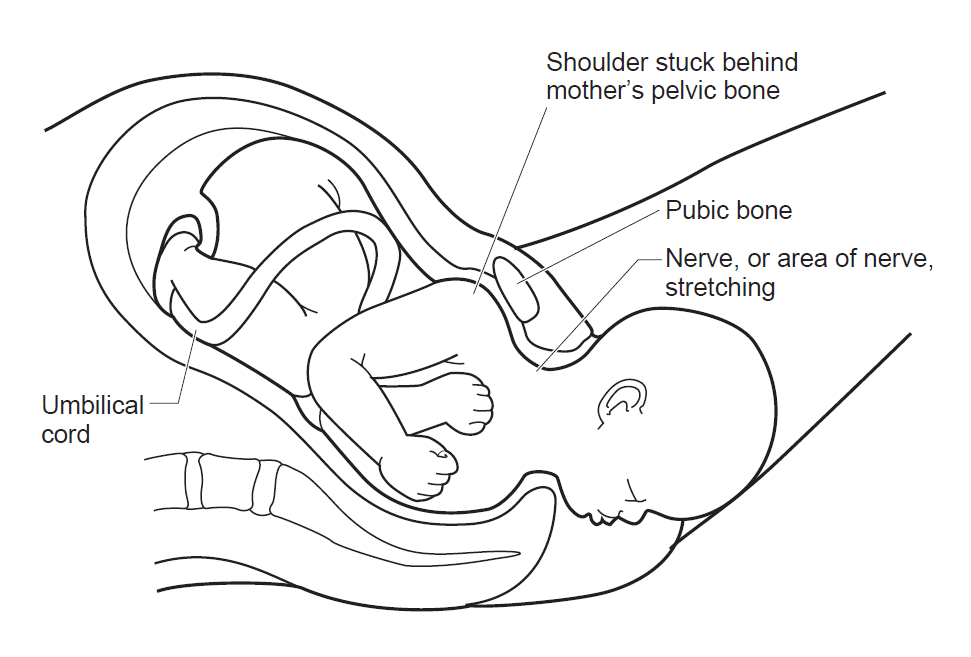     ## 🌸 **Definition** An obstetric emergency where after the fetal head delivers, the **anterior shoulder is impacted behind the maternal pubic symphysis**, preventing delivery. --- ## 🌸 **Risk Factors** * Macrosomia (>4 kg) * Maternal obesity * Diabetes in pregnancy * Post-term pregnancy * Instrumental delivery (vacuum/forceps) * Prolonged second stage of labour * Prior shoulder dystocia *(Note: Most cases are **unpredictable**.)* --- ## 🌸 **Signs** * **Turtle sign**: Retraction of the fetal head after delivery * Failure of restitution * Difficulty delivering the face/chin * “No progress” after the head is out --- ## 🌸 **Complications** ### **Maternal** * PPH * 3rd/4th degree perineal tears * Uterine rupture ### **Fetal** * **Brachial plexus injury (Erb palsy)** * Clavicle/humerus fracture * Hypoxia → brain damage * Neonatal death (rare but feared) --- ## 🌸 **Management — Mnemonic: HELPERR** ### **H – Help** Call senior obstetrician, pediatrician, anesthetist. ### **E – Episiotomy** Not mandatory, but may give space for internal maneuvers. --- ### 🌷 **L – McRoberts Maneuver (First-line)** * Hyperflex maternal thighs onto abdomen * Straightens sacral angle * Resolves **90%** cases. ### 🌷 **P – Suprapubic Pressure** * Apply downward & lateral pressure * Dislodges fetal anterior shoulder. --- ### 🌷 **E – Enter Maneuvers (Internal Rotations)** * **Rubin II**: Pressure on posterior aspect of anterior shoulder * **Woods Screw**: Rotate shoulder like a screw * **Reverse Woods Screw** --- ### 🌷 **R – Remove Posterior Arm** * Deliver posterior arm → reduces shoulder diameter. --- ### 🌷 **R – Roll to All-Fours (Gaskin Maneuver)** * Maternal position changes pelvic dimensions. --- ### **Last-Resort Maneuvers (Rare & Heroic)** * **Zavanelli maneuver** (cephalic replacement + emergency C-section) * **Clavicle fracture** * **Symphysiotomy** --- ## 🌸 **Prevention** * Good glycemic control in pregnancy * Consider elective C-section if: * Diabetic mother with EFW > 4.5 kg * Non-diabetic EFW > 5 kg --- # 🎀 Want MCQs / HTML-CSS-JS Quiz / SEO Titles? Tell me: 👉 “Give MCQs” 👉 “Give stylish HTML/CSS/JS quiz” 👉 “Give SEO title + description + keywords” I’ll generate them exactly in your preferred structure.
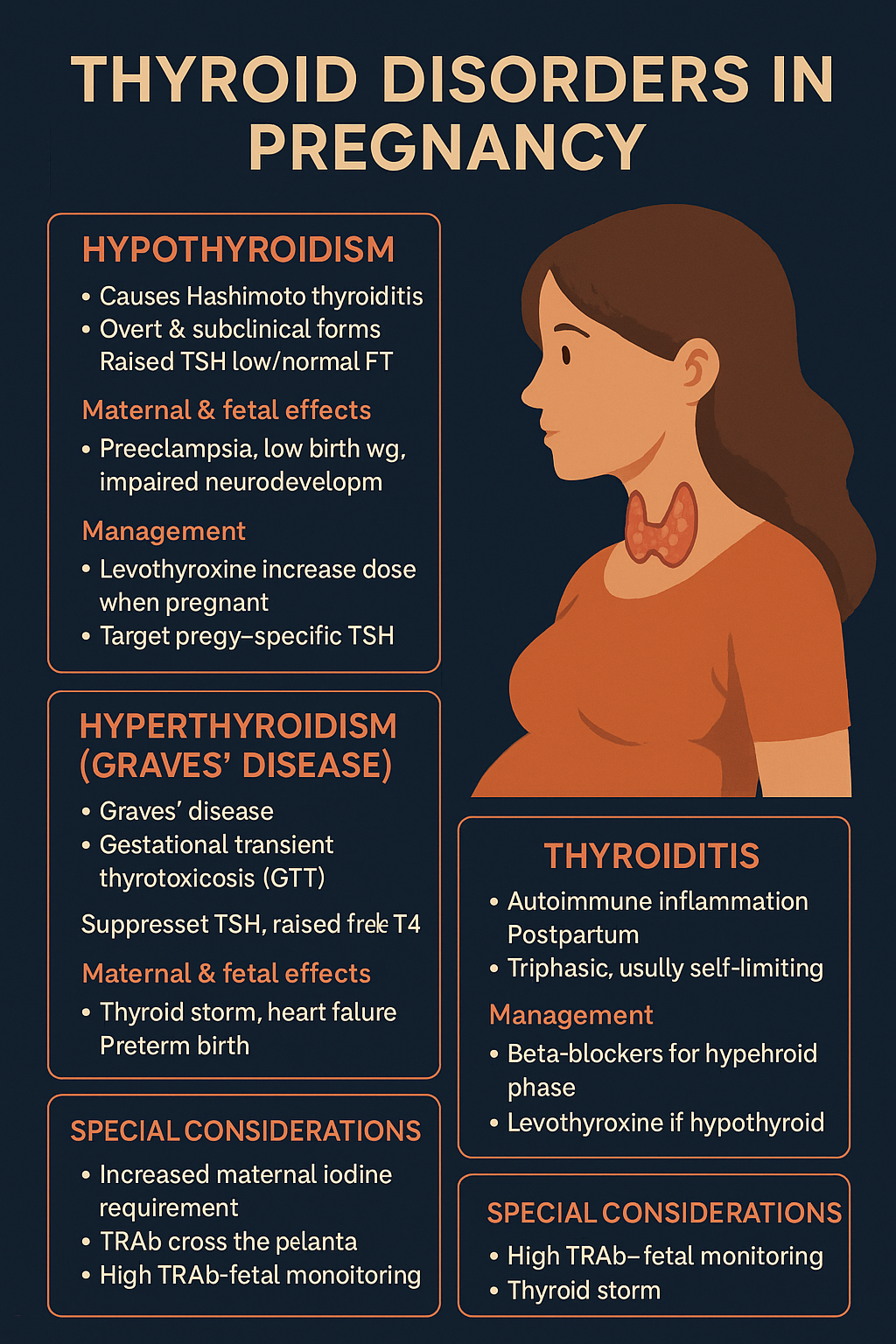
Thyroid Disorders in Pregnancy: Symptoms, Diagnosis, Risks & Treatment Guide (2025 Update)
Below is a **complete, concise-but-exhaustive, exam-ready medical reference** for **Thyroid Disorders in Pregnancy**, covering **hypothyroidism, hyperthyroidism (Graves’), thyroiditis, and special considerations**. --- # **Thyroid Disorders in Pregnancy — Complete Reference** ! --- # **1️⃣ Physiological Thyroid Changes in Pregnancy (Baseline Concepts)** Understanding normal physiology is essential to interpret labs: * ↑ **Thyroxine-binding globulin (TBG)** → ↑ total T3/T4, **free hormones unchanged**. * **hCG stimulates TSH receptors** → mild ↑ FT4 and **↓ TSH** in 1st trimester. * ↑ Renal iodide clearance → **↑ iodine requirement** (250 μg/day). * Placental **D2 deiodinase** degrades maternal T4. * TSH reference range changes: * 1st trimester: **0.1–2.5 mIU/L** * 2nd trimester: **0.2–3.0** * 3rd trimester: **0.3–3.0** --- # **2️⃣ HYPOTHYROIDISM IN PREGNANCY** ## **Definition** Low maternal thyroid hormone levels with elevated TSH (**primary**) or low/normal TSH (**secondary**). ## **Causes** * Hashimoto thyroiditis (most common). * Post-radioiodine or surgery. * Iodine deficiency. * Drugs: amiodarone, lithium. --- ## **Clinical Features** * Fatigue, weight gain, cold intolerance. * Constipation, dry skin. * Menstrual irregularities. * **Infertility, recurrent miscarriages**. * Severe: myxedema, heart failure. --- ## **Investigations** * **TSH (most sensitive)**. * **FT4** (interpret using pregnancy-specific ranges). * **Anti-TPO antibodies** (positive in autoimmune). * Check iron, B12 if associated anemia. --- ## **Maternal Complications** * Miscarriage * Anemia * Preeclampsia * Placental abruption * Preterm delivery * Postpartum hemorrhage --- ## **Fetal Complications** * Low birth weight * Preterm birth * **Impaired neurocognitive development** * Stillbirth --- ## **Management** **Goal: Maintain TSH in trimester-specific normal range.** ### **Levothyroxine (LT4)** * **Initial dose:** * Newly diagnosed: 1.6 µg/kg/day. * Already on LT4: **Increase dose by 30–50% immediately after pregnancy confirmation** (usually +2 extra tablets per week). * **Monitoring:** * Check TSH & FT4 every **4 weeks** in 1st/2nd trimester, then once at 30–34 weeks. * **Drug information (LT4):** * **Indication:** Hypothyroidism replacement. * **Mechanism:** Synthetic T4 → converts to T3 → restores euthyroidism. * **PK:** Absorption 70%; long half-life ~7 days; take empty stomach. * **AE:** Palpitations, tremor (over-replacement). * **Contraindications:** Untreated adrenal insufficiency. * **Interactions:** Iron, calcium, PPIs ↓ absorption → separate by 4 hours. * **Counselling:** Take daily, morning fasting; adherence crucial. --- # **3️⃣ SUBCLINICAL HYPOTHYROIDISM** * TSH ↑, FT4 normal. * Treat if: * TSH ≥ 2.5 in 1st trimester * **TPO-positive**, or * History of infertility, miscarriage. **Levothyroxine same as above.** --- # **4️⃣ HYPERTHYROIDISM IN PREGNANCY** 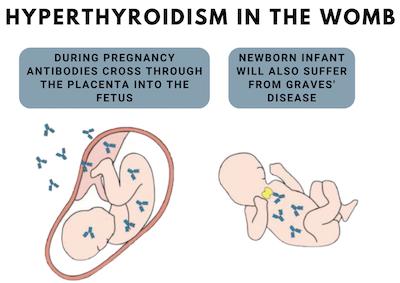   ## **Definition** Excess thyroid hormone due to increased production (Graves’ disease) or gland destruction (thyroiditis). --- ## **Causes** ### **1. Graves’ disease (most common)** Autoimmune stimulation by **TSH receptor antibodies (TRAb)**. ### **2. Gestational Transient Thyrotoxicosis (GTT)** * Due to hCG stimulation * Occurs in 1st trimester * Mild, self-limiting * Associated with **hyperemesis gravidarum** --- ## **Clinical Features** * Palpitations, heat intolerance * Weight loss * Tremors, anxiety * Goiter * Ophthalmopathy (Graves’) * Tachycardia → heart failure * Untreated cases → **thyroid storm** --- ## **Investigations** * TSH ↓, FT4 ↑ * **TRAb** for Graves’ * Thyroid ultrasound if nodules --- ## **Maternal Complications** * Preeclampsia * Thyroid storm * Heart failure * Miscarriage * Infection risk (if agranulocytosis from drugs) --- ## **Fetal Complications** * **Fetal hyperthyroidism or hypothyroidism** (due to TRAb or drugs) * Growth restriction * Preterm birth * Fetal goiter * Fetal tachycardia (>160/min) --- ## **Management** ### **1. Antithyroid Drugs (ATDs)** **Goal: keep FT4 in high-normal range.** #### **First trimester:** * **Propylthiouracil (PTU)** preferred * Lower teratogenicity vs. methimazole (MMI) * Dose: **50–150 mg TID** #### **Second & third trimesters:** * Switch to **Methimazole (MMI)** * Dose: **5–20 mg/day** ### **Drug information (ATDs)** #### **Propylthiouracil (PTU)** * **MOA:** inhibits TPO + peripheral T4→T3 conversion * **AE:** hepatotoxicity, rash, agranulocytosis * **Counselling:** Fever/sore throat → stop drug → urgent CBC. #### **Methimazole (MMI)** * **MOA:** inhibits TPO * **AE:** Aplasia cutis, choanal/esophageal atresia (1st trimester), cholestasis * **Monitoring:** FT4 every 4 weeks --- ### **2. Beta-blockers (Symptomatic control)** * **Propranolol 10–20 mg TID** short-term (2–6 weeks) * Avoid long-term due to fetal growth restriction. --- ### **3. Surgery** * Indications: * Drug intolerance * Large goiter * Very high TRAb * **Timing:** **Second trimester** --- # **5️⃣ POSTPARTUM THYROIDITIS** * Autoimmune inflammation after delivery * Phases: 1. Hyperthyroid (1–3 months) 2. Hypothyroid (4–6 months) 3. Recovery (1 year) ### Management * Hyperthyroid: **Beta-blockers** only * Hypothyroid: temporary **Levothyroxine** if symptomatic * Recurrence in future pregnancies: **70%** --- # **6️⃣ THYROID STORM IN PREGNANCY (EMERGENCY)**   ## **Features** * Fever, tachycardia, vomiting * Delirium, heart failure * Precipitated by labor, infection, surgery ## **Management Protocol** 1. **PTU 600–1000 mg loading dose**, then 200–300 mg Q6h 2. **Iodine solution** after 1 hour 3. **Propranolol** IV/oral 4. **Hydrocortisone 100 mg IV Q8h** 5. Treat precipitating cause 6. ICU care --- # **7️⃣ MONITORING SUMMARY** | Disorder | Follow-up | | ----------------------- | ---------------------------------------------------- | | Hypothyroidism | TSH every 4 weeks | | Hyperthyroidism on ATDs | FT4 every 4 weeks | | TRAb-positive Graves’ | TRAb at 24–28 weeks, fetal US for tachycardia/goiter | | Postpartum | Re-check thyroid at 6 weeks postpartum | --- # **8️⃣ FETAL SURVEILLANCE** * Fetal heart rate (tachycardia → hyperthyroid) * Fetal goiter on ultrasound * Growth assessment * Amniotic fluid volume * Doppler if growth restriction suspected --- # **9️⃣ KEY DIFFERENTIATION TABLE** | Condition | TSH | FT4 | TRAb | Treatment | | ----------- | --- | ------ | ------------ | ------------- | | Graves’ | ↓ | ↑ | ↑ | PTU → MMI | | GTT | ↓ | Mild ↑ | Normal | Supportive | | Hypothyroid | ↑ | ↓ | TPO+ | Levothyroxine | | Subclinical | ↑ | Normal | TPO variable | Treat if TPO+ | --- # **Would you like an SEO title, description, keywords, or an infographic for this topic?**
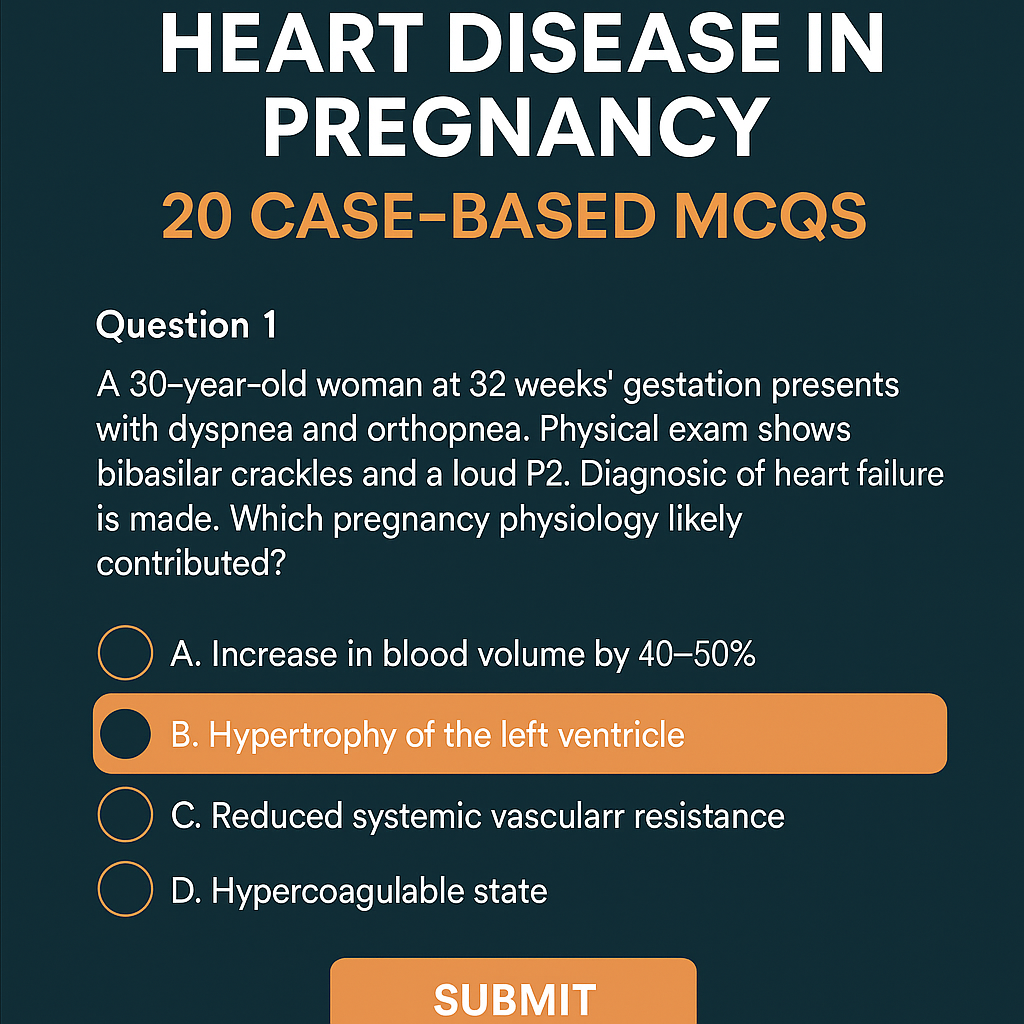
Heart Disease in Pregnancy: Causes, Risks, Management & 20 Case-Based MCQs (With Answers & Explanations)
Below is a **complete, exam-ready, concise-but-exhaustive reference** for **Heart Disease in Pregnancy** — covering definition, physiology, classification, clinical features, investigations, management (stepwise), drug details, labor/delivery planning, postpartum care, and contraindications. --- # **Heart Disease in Pregnancy – Complete Overview** ! --- ## **1. Definition** Heart disease in pregnancy refers to **pre-existing cardiac disorders** (congenital or acquired) or **pregnancy-induced cardiac dysfunction** (e.g., peripartum cardiomyopathy) that complicate pregnancy, labor, or postpartum period. --- ## **2. Why Pregnancy Worsens Heart Disease (Physiological Changes)** Pregnancy causes major hemodynamic changes that peak at **28–32 weeks**: * **↑ Blood volume by 40–50%** * **↑ Cardiac output by 30–50%** * **↑ Heart rate by 10–20 bpm** * **↓ Systemic vascular resistance** * **Hypercoagulable state** * **During labor:** CO ↑ 20–30% more * **Immediately postpartum:** Autotransfusion ↑ CO up to 80% These changes may **unmask latent heart disease** or **worsen existing cardiac failure**. --- ## **3. Types of Heart Diseases Seen in Pregnancy** ### **A. Congenital Heart Disease (CHD)** * Atrial septal defect (ASD) * Ventricular septal defect (VSD) * Patent ductus arteriosus (PDA) * Tetralogy of Fallot (repaired/unrepaired) * Eisenmenger syndrome (very high-risk) ### **B. Acquired Heart Disease** * Rheumatic heart disease * Mitral stenosis (most common serious lesion in pregnancy) * Mitral regurgitation * Aortic stenosis * Cardiomyopathies * **Peripartum cardiomyopathy** * Ischemic heart disease * Arrhythmias * Hypertensive heart disease --- ## **4. WHO Classification of Maternal Cardiovascular Risk** ### **WHO Class I – Low Risk** * Small ASD/VSD * PDA * Mitral valve prolapse * Successfully repaired simple CHD ### **WHO Class II – Moderate Risk** * Unrepaired ASD/VSD * Repaired TOF * Mild LV dysfunction ### **WHO Class III – High Risk** * Mechanical valves * Cyanotic congenital heart disease * Moderate LV dysfunction * Previous peripartum cardiomyopathy with normal EF now ### **WHO Class IV – Extremely High Risk (Pregnancy Contraindicated)** * **Pulmonary hypertension / Eisenmenger syndrome** * **Severe LV dysfunction (EF < 30%)** * **Severe mitral stenosis or aortic stenosis** * **Marfan syndrome with aorta > 45 mm** * **Previous peripartum cardiomyopathy with persistent dysfunction** --- ## **5. Clinical Features** ### **Symptoms** * Dyspnea (especially NYHA III–IV) * Orthopnea / PND * Fatigue * Palpitations * Chest pain * Syncope ### **Warning Features of Cardiac Decompensation** * Dyspnea at rest * Hemoptysis * Cyanosis * Loud P2 / RV heave * Basal crepitations * New arrhythmias --- ## **6. Investigations** ### **Basic** * CBC * ECG * **Echocardiography – Most important** * BNP (optional) ### **Advanced** * Cardiac MRI (safe without gadolinium) * Holter monitoring * Exercise testing (pre-pregnancy only) ### **Avoid** * CT angiography unless life-saving * ACE inhibitors / ARBs history to be checked --- ## **7. Complications** * **Maternal:** Heart failure, arrhythmias, thromboembolism, endocarditis, cardiac arrest * **Fetal:** IUGR, preterm birth, fetal hypoxia, congenital heart disease (3–5% risk) --- # **8. Management of Heart Disease in Pregnancy (Stepwise)**   --- ## **A. Preconception Counselling** * Risk assessment + WHO classification * Optimize cardiac status (e.g., balloon valvotomy for MS) * Stop teratogenic drugs (ACE inhibitors, ARBs, statins, warfarin if possible) --- ## **B. Antenatal Management** ### **1. Lifestyle** * Adequate rest * Left lateral position * Avoid anemia (treat aggressively) * Avoid excessive weight gain * Salt restriction if HF symptoms ### **2. Drugs Used** Below are the major drug classes **with indications, mechanism, dosing, adverse effects, contraindications, interactions, and counselling.** --- ## **i. Diuretics (Furosemide)** **Indication:** Heart failure, pulmonary edema **MOA:** Loop diuretic → inhibits Na-K-2Cl in loop of Henle **Dose:** 20–40 mg PO/IV, repeat as required **PK:** Rapid onset, renal excretion **AEs:** Hypokalemia, dehydration **Contra:** Severe electrolyte imbalance **Interactions:** Digoxin ↑ toxicity if hypokalemia **Counselling:** Monitor weight, urine output, electrolytes --- ## **ii. Beta-blockers (Metoprolol preferred)** **Indication:** Rate control, arrhythmias, ischemic heart disease **MOA:** Blocks β1 receptors → ↓ HR & contractility **Dose:** 25–100 mg/day **AEs:** IUGR (minimal), bradycardia **Contra:** Severe asthma **Interactions:** Calcium channel blockers → heart block risk **Counselling:** Do not stop suddenly --- ## **iii. Anticoagulants** ### **a. LMWH (Enoxaparin) – Preferred** **Indication:** Mechanical valves, AF, thromboembolism **MOA:** Enhances antithrombin III → inhibits Xa **Dose:** 1 mg/kg twice daily **Monitoring:** Anti-Xa levels **AEs:** Bleeding **Contra:** Active bleeding ### **b. Warfarin – Teratogenic (avoid 6–12 weeks)** Used only when valve thrombosis risk is very high. --- ## **iv. Vasodilators (Hydralazine, Nitrates)** **Indication:** HF with hypertension **AEs:** Headache, hypotension --- ## **v. Digoxin** **Indication:** HF with atrial fibrillation **MOA:** Na-K ATPase inhibition → ↑ Ca → ↑ contractility **Dose:** 0.125–0.25 mg daily **AEs:** Toxicity (nausea, vision changes) **Monitor:** Serum levels --- ## **Drugs Contraindicated in Pregnancy** * **ACE inhibitors / ARBs** → renal failure, skull defects * **Amiodarone** → fetal thyroid dysfunction * **Warfarin (first trimester)** unless essential * **Statins** --- ## **C. Follow-up Schedule** * Monthly (WHO I–II) * Fortnightly (WHO III) * Weekly (WHO IV — pregnancy discouraged) --- # **9. Labor and Delivery Management**   ### **Preferred Mode:** **Vaginal delivery with epidural anesthesia** ### **Indications for Caesarean Section** * Severe aortic stenosis * Marfan with aortic root dilation * Eisenmenger * Severe HF * Anticoagulation not stopped ### **Intrapartum Measures** * Continuous ECG + pulse oximetry * Avoid fluid overload * Slow, assisted second stage (forceps/vacuum) ### **Anesthesia** * Epidural preferred * Avoid general anesthesia (↑ cardiac stress) --- # **10. Postpartum Care** * Highest risk of heart failure in **first 24–72 hours** * Gradual mobilization * Restart anticoagulation after 6 hours (if needed) * Contraception counselling * **Avoid estrogen pills** * Prefer: IUCD, progestin-only methods --- # **11. High-Risk Specific Conditions** ## **A. Mitral Stenosis** * Most dangerous RHD lesion in pregnancy * Tachycardia → ↑ LA pressure → pulmonary edema * Management: β-blockers + diuretics * Balloon valvotomy if severe --- ## **B. Eisenmenger Syndrome** * **Pregnancy contraindicated (WHO IV)** * Maternal mortality 30–50% * No effective treatment → counselling for termination --- ## **C. Peripartum Cardiomyopathy** * Heart failure in last month of pregnancy or 5 months postpartum * EF < 45% * Treatment: * Diuretics * Beta-blockers * Bromocriptine (stops prolactin → improves function) * Avoid future pregnancy if EF not normalized --- # **12. Fetal Risks** * Prematurity * Growth restriction * Neonatal asphyxia * Congenital heart disease (if mother has CHD) --- # **13. Key Prevention Strategies** * Early diagnosis * Control anemia * Avoid excessive fluids * Use cardiac medications judiciously * Multidisciplinary care (obstetrician + cardiologist) --- # **Would you like a SEO-optimized title & description for this topic, or a high-ranking blog article version?**
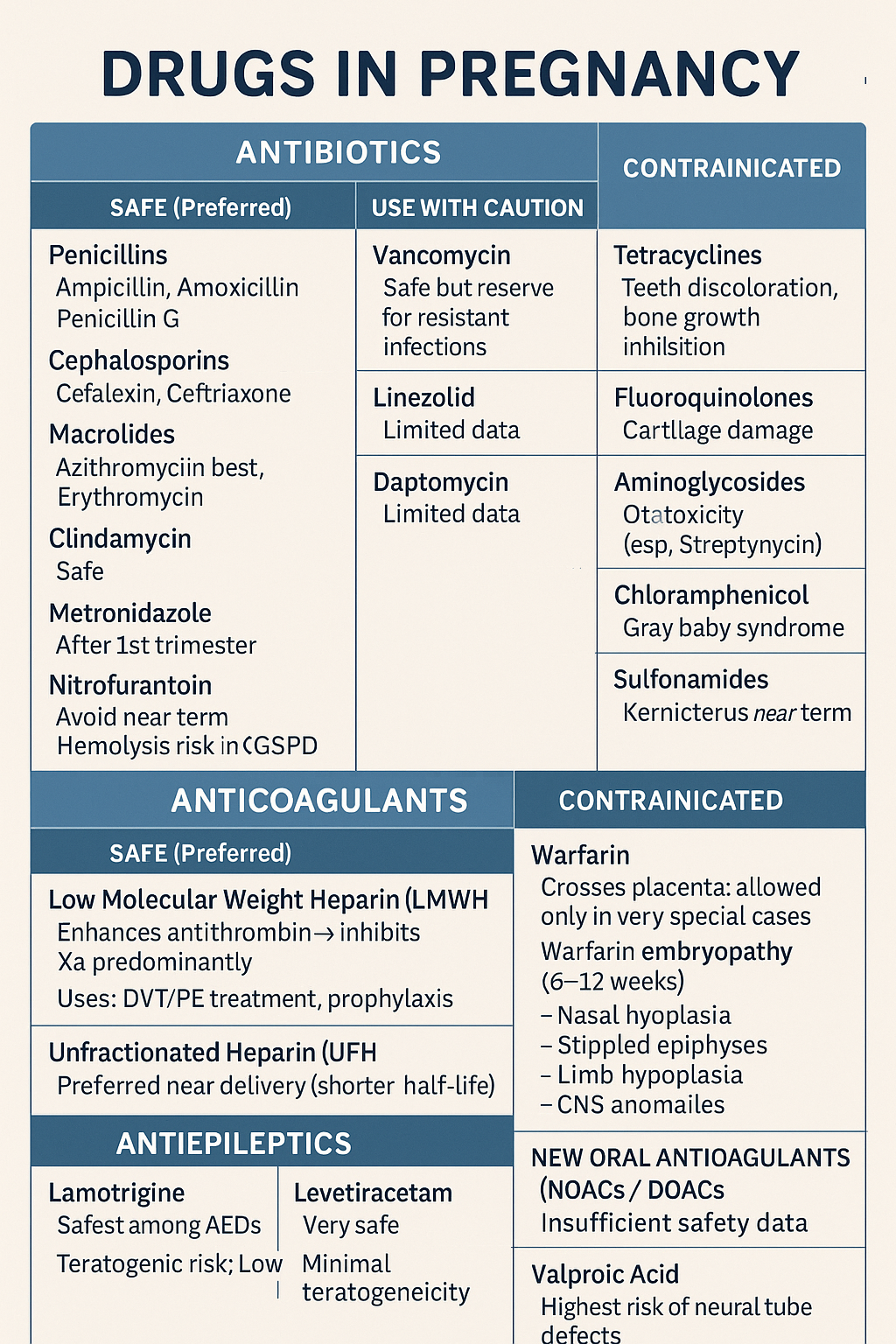
Comprehensive guide on safe and unsafe drugs in pregnancy including antibiotics, anticoagulants, and antiepileptics. Covers risks, teratogenicity, and clinical management
Below is a **concise but complete, exam-ready note** on **Drugs in Pregnancy – Antibiotics, Anticoagulants, Antiepileptics**. Structured for **quick revision + maximum coverage**. --- # ⭐ **DRUGS IN PREGNANCY – DETAILED NOTE (ANTIBIOTICS, ANTICOAGULANTS, ANTIEPILEPTICS)**    ## ✔ **SAFE (Preferred)** ### **Low Molecular Weight Heparin (LMWH)** * **Examples:** Enoxaparin, Dalteparin * **Mechanism:** Enhances antithrombin → inhibits **Xa** predominantly * **Does NOT cross placenta → safest anticoagulant** * **Uses:** DVT/PE treatment, prophylaxis, thrombophilia, APS * **Monitoring:** Anti-Xa levels in special cases (obesity, renal disease) ### **Unfractionated Heparin (UFH)** * Safe (does not cross placenta) * Preferred **near delivery** (shorter half-life, reversible with protamine) --- ## ❌ **CONTRAINDICATED** ### **Warfarin** * Crosses placenta → **warfarin embryopathy** (6–12 weeks): * Nasal hypoplasia * Stippled epiphyses * Limb hypoplasia * CNS anomalies * **Fetal hemorrhage** anytime * **Allowed only in very special cases:** mechanical heart valves when LMWH fails. --- ## ⚠ **NEW ORAL ANTICOAGULANTS (NOACs / DOACs)** Apixaban, Rivaroxaban, Dabigatran * **Avoid in pregnancy** → insufficient safety, crosses placenta --- # 3️⃣ **ANTIEPILEPTICS IN PREGNANCY**  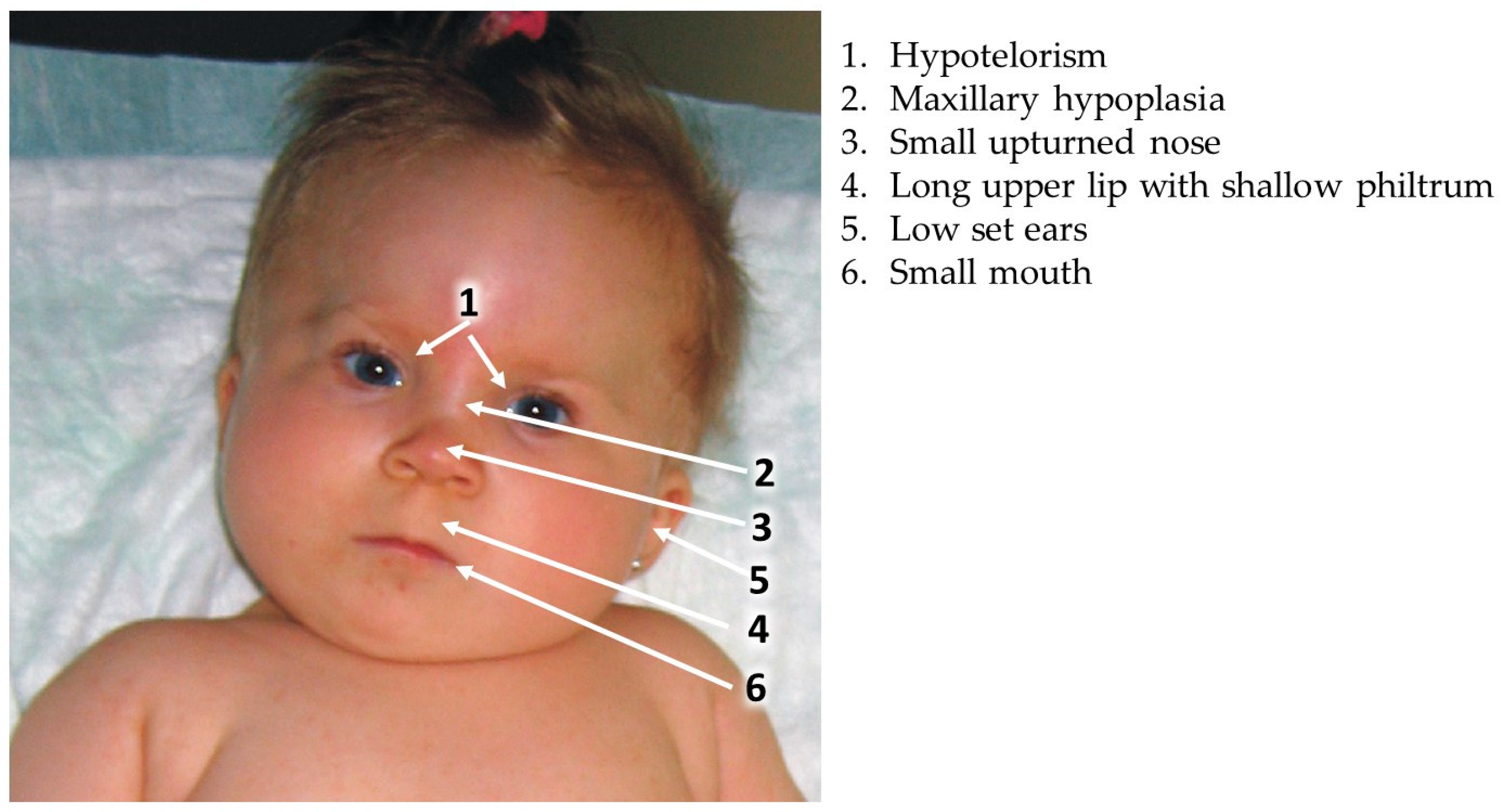   ## ⭐ **KEY PRINCIPLES** * Goal: **Seizure control** (maternal seizures are more harmful than drug risk) * Use **monotherapy** at **lowest effective dose** * Supplement **Folic acid 4–5 mg/day preconception → 1st trimester** * Check drug levels in pregnancy (pharmacokinetics change) --- ## ✔ **RELATIVELY SAFE ANTIEPILEPTICS (Preferred)** ### **1. Lamotrigine** * Safest among AEDs * **Teratogenic risk:** Low * **PK:** Increased clearance → dose adjustment needed * **Adverse:** Rash (SJS risk) ### **2. Levetiracetam** * Very safe * Minimal teratogenicity * Well-tolerated ### **3. Carbamazepine (with caution)** * Moderate teratogenic risk * Associated with **neural tube defects (NTD)** (~1%) * Give **high-dose folic acid** --- ## ⚠ **USE WITH CAUTION** | AED | Risk | | ----------------- | ---------------------------------------------------------------------- | | **Phenytoin** | Fetal hydantoin syndrome: growth delay, facial anomalies, limb defects | | **Topiramate** | Cleft lip/palate | | **Phenobarbital** | Cognitive defects, withdrawal | --- ## ❌ **AVOID / HIGHLY TERATOGENIC** ### **Valproic Acid** * **Highest risk of neural tube defects (5–10%)** * Cognitive impairment * Cardiac defects * Dose-dependent teratogenicity * **Avoid in pregnancy unless no alternative** --- # 4️⃣ **IMPORTANT COMPARISON TABLES** ## **A. Safe vs Unsafe Antibiotics** | Safe | Unsafe | | ------------------------------ | -------------------------- | | Penicillins | Tetracycline | | Cephalosporins | Fluoroquinolones | | Azithromycin | Aminoglycosides (ototoxic) | | Metronidazole (after 1st tri) | Chloramphenicol | | Nitrofurantoin (not near term) | Sulfonamides (near term) | --- ## **B. Safe vs Unsafe Anticoagulants** | Safe | Unsafe | | ---- | -------- | | LMWH | Warfarin | | UFH | NOACs | --- ## **C. Safe vs High-Risk Antiepileptics** | Safer | Moderate | High-risk | | ------------- | ------------- | ------------- | | Lamotrigine | Carbamazepine | Valproate | | Levetiracetam | Phenytoin | Phenobarbital | | — | Topiramate | — | --- # 5️⃣ **MANAGEMENT SUMMARY IN PREGNANCY** ### 🔹 **Infection** * Prefer beta-lactams * Avoid teratogenic antibiotics * Treat aggressively because **maternal sepsis harms fetus more** ### 🔹 **Thromboembolism** * **LMWH first-line** * Switch to UFH close to delivery * Avoid warfarin except mechanical valves requiring high-intensity anticoagulation ### 🔹 **Epilepsy** * Continue AEDs (never stop abruptly) * Choose **Lamotrigine or Levetiracetam** * Avoid **Valproate** * High-dose folic acid (4–5 mg/day) --- If you want, I can also generate: ✅ **25 MCQs (HTML/CSS/JS exam mode)** ✅ **Case scenarios with management** ✅ **SEO title + description + keywords** ✅ **Infographics / images for notes** Just tell me!
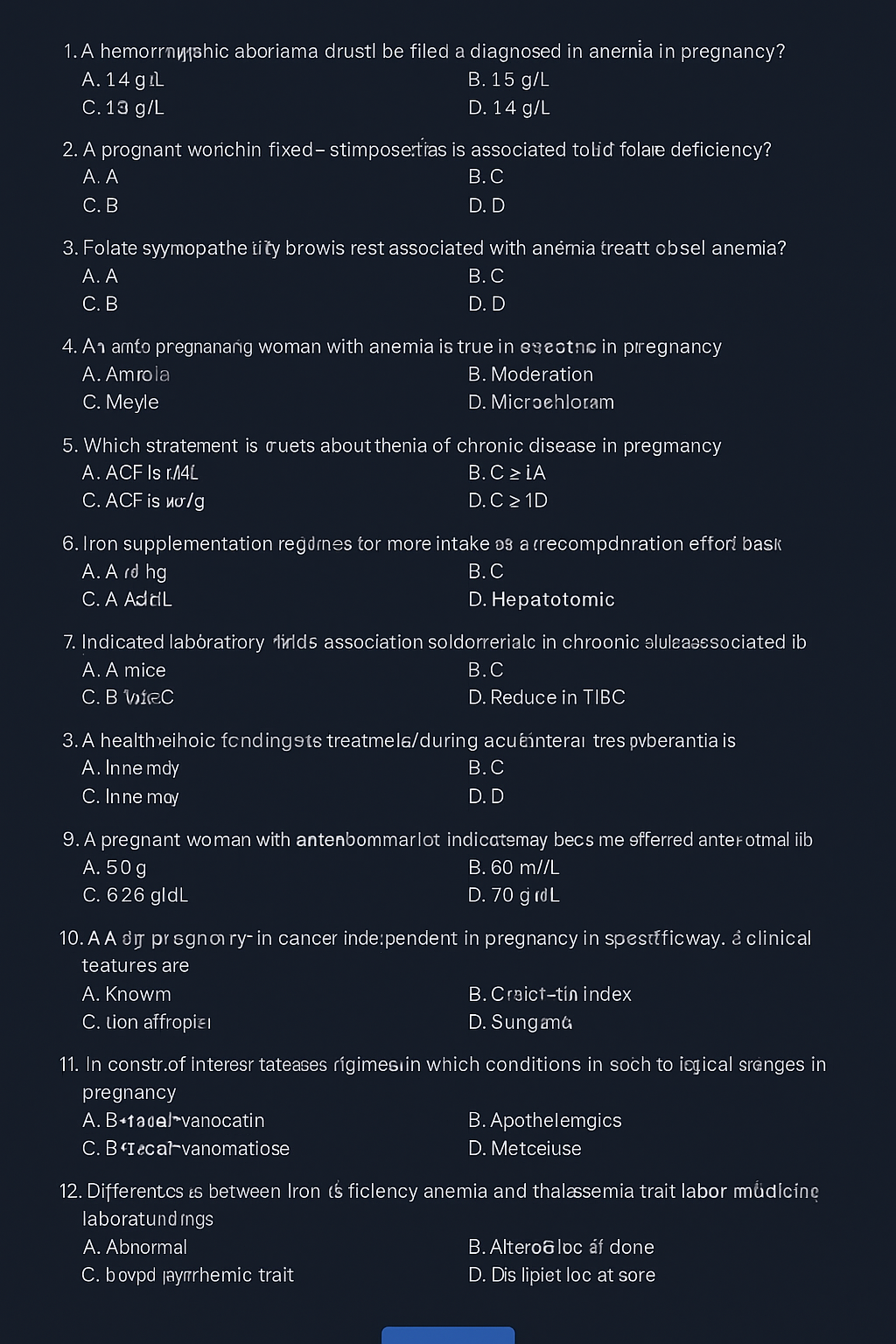
Complete guide on anaemia in pregnancy including causes, WHO definition, diagnosis, iron requirements, IFA tablets, NIAP, Anemia Mukt Bharat, treatment & management.
Great — I made **30 concise, high-yield case scenarios** on anaemia in pregnancy. Each case includes: brief history/exam, key labs, working diagnosis, immediate management, definitive treatment plan, and follow-up. I kept dosing and practical steps clear so you can paste these into teaching slides, case banks or clinical notes. --- # 30 Case Scenarios — Anaemia in Pregnancy (with management) > Legend: FS 325 mg ≈ 65 mg elemental Fe; typical oral treatment: **60–120 mg elemental Fe/day** (commonly 1 FS 325 mg once–three times daily depending on severity/tolerance). IV iron options: **iron sucrose** (commonly 100–200 mg per infusion repeated to calculated total) or **ferric carboxymaltose (FCM)** (single doses up to 750–1000 mg per product guidance). Transfusion generally considered for **Hb ≤7.0 g/dL** or symptomatic/hemodynamically unstable patient; tailor to obstetric context. --- ### Case 1 — Mild IDA, first trimester * Presentation: 24 y, G1P0, 10 wks, fatigue. Exam: pallor only. * Labs: Hb 10.2 g/dL, MCV 74 fL, ferritin 8 ng/mL, Mentzer >13. Smear: microcytic hypochromic. * Dx: Iron deficiency anaemia (mild). * Immediate mgmt: Start oral iron — **FS 325 mg once daily** (≈65 mg elemental) + folic acid 400 µg; counsel on absorption and side effects. * Definitive plan: Check Hb at 4 weeks; if Hb rising by ~1 g/dL, continue 3 months after normalization to replete stores. Diet & deworm if indicated. --- ### Case 2 — Moderate IDA, second trimester, poor diet * Presentation: 29 y, 20 wks, progressive exertional dyspnea. * Labs: Hb 8.3 g/dL, MCV 68 fL, ferritin 9 ng/mL. * Dx: Moderate IDA. * Immediate mgmt: Oral iron **FS 325 mg twice daily** (≈130 mg elemental/day) + folic acid; start vitamin C with dose. Consider adherence issues. * Definitive plan: Reassess Hb in 2–3 weeks. If poor response or intolerance → switch to IV iron (calculate total deficit; consider FCM 1000 mg single or iron sucrose series). --- ### Case 3 — Severe symptomatic anaemia late pregnancy * Presentation: 31 y, 36 wks, chest tightness, syncope history. Exam: tachycardia, low BP. * Labs: Hb 5.8 g/dL, MCV 75 fL, ferritin 5 ng/mL. * Dx: Severe IDA with hemodynamic compromise. * Immediate mgmt: Resuscitate (IV fluids as needed), **blood transfusion** (matched PRBCs) — aim to stabilise; crossmatch and transfuse per obstetric transfusion protocol. * Definitive plan: After stabilization, give IV iron (iron sucrose/FCM) to replete stores; counsel for delivery planning and postpartum follow-up. --- ### Case 4 — Late presentation, intolerance to oral iron * Presentation: 26 y, 34 wks, vomiting with oral iron causing severe nausea. * Labs: Hb 9.0 g/dL, ferritin 10 ng/mL. * Dx: IDA with oral intolerance. * Immediate mgmt: Stop oral iron; offer **IV iron** (iron sucrose series or FCM depending on availability) to correct quickly pre-delivery. Monitor vitals during infusion. * Follow-up: Hb/ferritin 2–4 weeks post-infusion; resume oral prophylaxis postpartum. --- ### Case 5 — Refractory anaemia despite oral iron * Presentation: 28 y, 22 wks, on FS 325 mg TID x 6 weeks, minimal Hb rise. * Labs: Hb 9.2 g/dL, ferritin 6 ng/mL, reticulocyte low-normal. * Dx: Non-response to oral iron (malabsorption, non-adherence, ongoing loss). * Immediate mgmt: Evaluate adherence, check for parasites/GI blood loss. If adherence OK → **IV iron**. Consider stool testing for hookworm. Screen for celiac if suspicion. * Definitive plan: Treat underlying cause; calculate iron deficit and give IV iron. --- ### Case 6 — Microcytosis suspicious for thalassaemia trait * Presentation: 21 y, 12 wks, mild pallor. Labs: Hb 10.8 g/dL, MCV 65 fL, RBC count high, Mentzer <13, ferritin normal 50 ng/mL. * Dx: Likely β-thalassaemia trait. * Mgmt: Confirm with **Hb electrophoresis (elevated HbA₂)**. Do **not** give high-dose iron if ferritin normal. Genetic counselling and partner screening. Provide routine antenatal care; avoid unnecessary iron. --- ### Case 7 — Anaemia of chronic disease (ACD) * Presentation: 34 y, known lupus, 28 wks, fatigue. Labs: Hb 9.6 g/dL, ferritin 180 ng/mL, low serum iron, low TIBC. CRP high. * Dx: ACD due to chronic inflammation. * Mgmt: Treat underlying disease flare; iron supplementation only if true iron deficiency coexists (assess transferrin saturation). Consider erythropoiesis-stimulating agents only in specialist settings; consult rheumatology/hematology. --- ### Case 8 — Folate deficiency plus iron deficiency * Presentation: 30 y, 18 wks, glossitis, neural tube risk concern. Labs: Hb 9.4 g/dL, MCV 102 fL, low folate. Smear: macro-ovalocytes. Ferritin low-normal. * Dx: Mixed folate deficiency ± iron deficiency. * Mgmt: Start **folic acid 5 mg daily** (treatment dose) + oral iron (if ferritin low). Investigate diet, malabsorption. Reassess CBC after 2–4 weeks. --- ### Case 9 — B12 deficiency in pregnancy * Presentation: 27 y, 24 wks, paresthesia, macrocytic indices. Labs: Hb 8.9 g/dL, MCV 108 fL, low B12. * Dx: B12 deficiency. * Mgmt: **IM/SC cyanocobalamin** replacement (e.g., 1000 µg IM weekly × several doses then monthly) depending on cause; treat concurrently with folate if needed. Neurologic signs may take months to improve. --- ### Case 10 — Postpartum haemorrhage with acute blood loss * Presentation: 35 y, day 1 postpartum after PPH, tachycardic, Hb 6.1 g/dL. * Dx: Acute severe anaemia from blood loss. * Mgmt: Immediate resuscitation; **urgent transfusion** (PRBCs), manage bleeding source (surgical/medical). After stabilization consider IV iron for repletion. --- ### Case 11 — Twin pregnancy with increased iron need * Presentation: 32 y, twin gestation 28 wks, fatigue. Labs: Hb 9.0 g/dL, ferritin 12 ng/mL. * Dx: IDA in multiple pregnancy. * Mgmt: Start **oral iron** at treatment dose (FS 325 mg twice daily) and consider early IV iron if inadequate response or near-term to optimize Hb before delivery. Close monitoring. --- ### Case 12 — Hyperemesis gravidarum causing iron deficiency * Presentation: 22 y, 10 wks, severe vomiting; poor intake. Labs: Hb 9.8 g/dL, ferritin 15 ng/mL. * Dx: IDA from poor intake. * Mgmt: Correct dehydration, antiemetics + start **oral iron** when tolerated (consider IV iron if vomiting prevents oral intake). Nutritional support and folate. --- ### Case 13 — Hookworm infection causing chronic blood loss * Presentation: 25 y, 26 wks, pica, eosinophilia. Labs: Hb 8.7 g/dL, ferritin 7 ng/mL. Stool: ova consistent with hookworm. * Dx: IDA due to helminthiasis. * Mgmt: Treat hookworm per local protocol (deworming timing per antenatal policy; e.g., single-dose albendazole often after first trimester in many settings), start oral iron or IV iron if severe; public-health measures. --- ### Case 14 — Malaria-associated anaemia in pregnancy * Presentation: 28 y, febrile 30 wks, pallor, splenomegaly. Labs: Hb 7.9 g/dL, smear positive for Plasmodium. * Dx: Malaria-related anaemia. * Mgmt: Treat malaria urgently with pregnancy-safe antimalarial per local guideline; transfuse if severe/symptomatic; start iron only after clearing infection and per clinician judgment. --- ### Case 15 — HIV with anaemia of multifactorial cause * Presentation: 29 y, known HIV on ART, 20 wks, fatigue. Labs: Hb 9.0 g/dL, ferritin 90 ng/mL, MCV variable. * Dx: Multifactorial (ACD, drug-related, nutritional). * Mgmt: Review ART (e.g., zidovudine can cause anaemia), treat nutritional deficiencies, consider IV iron if IDA confirmed and oral therapy fails; coordinate with HIV care. --- ### Case 16 — Renal disease with anemia in pregnancy * Presentation: 36 y, CKD stage 3, 24 wks, low energy. Labs: Hb 8.6 g/dL, ferritin 150 ng/mL, low reticulocyte. * Dx: Anaemia of CKD/ACD. * Mgmt: Nephrology consult; consider IV iron if iron-deficient; consider erythropoiesis stimulating agents in specialist setting; optimise dialysis/renal care. --- ### Case 17 — Recurrent anemia after oral iron completion * Presentation: 27 y, previously treated IDA, returns 3 months postpartum with Hb 9.5 g/dL. Ferritin low 12 ng/mL. * Dx: Recurrent iron deficiency. * Mgmt: Reassess for ongoing bleeding; restart iron therapy; investigate heavy menstrual bleeding; counsel on compliance and diet; consider long-term iron strategy until cause fixed. --- ### Case 18 — Anaemia with allergic reaction to IV iron history * Presentation: 30 y, history of anaphylaxis to IV iron dextran. Now 30 wks, Hb 7.5 g/dL. * Dx: Severe IDA with prior IV iron allergy. * Mgmt: Avoid offending agent; use non-dextran formulations (iron sucrose or FCM) under monitored conditions with resuscitation available; consider transfusion if urgent and risk high. --- ### Case 19 — Mixed thalassaemia trait + iron deficiency * Presentation: 23 y, MCV 68 fL, Mentzer borderline, ferritin low 10 ng/mL. * Dx: Mixed iron deficiency + thalassaemia trait. * Mgmt: Treat iron deficiency (oral/IV as needed) — correct iron first and reassess indices; refer to hematology/genetic counselling for thalassaemia. --- ### Case 20 — Severe anaemia with cardiac compromise * Presentation: 38 y, 34 wks, signs of high-output cardiac failure (orthopnea), Hb 6.5 g/dL. * Dx: Severe anaemia causing cardiac strain. * Mgmt: Urgent transfusion and cardiac support; plan delivery in appropriate setting once stabilized; consider IV iron after haemodynamic stability. --- ### Case 21 — Antenatal screening finds microcytic anaemia in partner/partner screening scenario * Presentation: 26 y, first visit, Hb 11.1 g/dL but MCV 72 fL. Ferritin 40 ng/mL. RBC count high. Mentor index <13. * Dx: Possible thalassaemia trait carrier. * Mgmt: Do Hb electrophoresis; if positive, offer partner testing and genetic counselling; avoid unnecessary iron if iron stores adequate. --- ### Case 22 — Severe anaemia in adolescent pregnant patient * Presentation: 17 y, 18 wks, symptomatic, Hb 7.2 g/dL. * Dx: Severe IDA. * Mgmt: Consider transfusion if symptomatic; otherwise start IV iron if available; add nutritional counselling, address social determinants (poverty/diet), involve adolescent health services. --- ### Case 23 — Anaemia discovered during labour * Presentation: 30 y, in labor, known Hb 8.0 g/dL on admission. * Dx: Moderate IDA at delivery. * Mgmt: Plan for blood availability if bleeding risk high; give IV iron postpartum if Hb fails to improve and prolonged recovery expected; active management of third stage of labour to avoid PPH. --- ### Case 24 — Severe IDA with late booking and need for rapid correction before c-section * Presentation: 33 y, booked at 38 wks, Hb 8.0 g/dL, scheduled c-section next week. * Dx: IDA needing rapid optimization. * Mgmt: Give **IV iron (FCM 1000 mg if available)** to increase Hb/iron stores quickly pre-op; if immediate correction required and Hb very low → transfuse perioperatively. --- ### Case 25 — Anaemia in pregnancy with concurrent sepsis * Presentation: 29 y, fever, Hb 8.4 g/dL, high CRP. * Dx: Anaemia with infective/inflammatory component. * Mgmt: Treat infection promptly; avoid confounding ferritin interpretation; if iron deficiency coexists and severe → consider IV iron once infection controlled; transfuse if hemodynamically unstable. --- ### Case 26 — Peripartum transfusion reaction risk scenario * Presentation: 35 y, urgent PPH, requires transfusion; prior transfusion history with antibodies. * Dx: Acute blood loss anaemia with alloimmunisation risk. * Mgmt: Coordinate blood bank for phenotype-matched units; transfuse as required; consider tranexamic acid and uterotonics; document antibody and counsel for future pregnancies. --- ### Case 27 — Anaemia with hemolysis (autoimmune) * Presentation: 31 y, jaundice, Hb 7.6 g/dL, elevated LDH, indirect bilirubin, positive direct Coombs. * Dx: Autoimmune hemolytic anemia (AIHA) in pregnancy. * Mgmt: Hematology consult; treat (corticosteroids first-line), transfusion if needed (with crossmatch); avoid IV iron while active hemolysis unless iron deficient; monitor fetus for hydrops if severe. --- ### Case 28 — Iron overload concern (hemochromatosis suspicion) * Presentation: 34 y, elevated ferritin 500 ng/mL, high transferrin saturation, mild anemia. Family history of hemochromatosis. * Dx: Possible iron overload or inflammation. * Mgmt: Evaluate for hereditary hemochromatosis outside pregnancy (genetic testing, specialist input); avoid unnecessary iron; treat underlying cause of high ferritin (inflammation vs overload). --- ### Case 29 — Antenatal prophylaxis non-adherence with borderline anaemia * Presentation: 28 y, missed many ANC visits, Hb 10.6 g/dL, ferritin 22 ng/mL. * Dx: Borderline anemia/early IDA. * Mgmt: Reinforce routine prophylaxis (30–60 mg elemental iron + folic acid), provide education, address barriers (side effects, access), recheck Hb in 4 weeks and treat if progresses. --- ### Case 30 — Severe postpartum anaemia with breastfeeding * Presentation: 27 y, 2 weeks postpartum, Hb 6.8 g/dL, symptomatic (dizziness), breastfeeding. * Dx: Severe postpartum anaemia (likely iron deficient). * Mgmt: Consider transfusion if symptomatic/severe; give IV iron if breastfeeding and stable (IV iron safe in lactation); if oral is chosen, counsel on adherence and side effects; follow-up Hb and ferritin, continue iron 3 months after repletion. --- # Quick management reminders (pasteable) * **Screening**: Hb at booking and at 28 wks. * **Oral iron**: FS 325 mg ≈ 65 mg elemental; treatment = **60–120 mg elemental/day** until stores replete. Take on empty stomach with vitamin C; separate from antacids. * **IV iron**: Use for intolerance, non-response, late pregnancy needing rapid correction, malabsorption, or severe anaemia when oral not feasible. Iron sucrose (100–200 mg per dose) or FCM (single large dose 750–1000 mg). Monitor for reactions. * **Transfusion**: Individualise. Usually **Hb ≤7.0 g/dL** or symptomatic/hemodynamic compromise → transfuse. In obstetrics, clinical scenario dictates threshold. * **Follow-up**: Check Hb 2–4 weeks after therapy start and continue iron for 3 months after normalization. --- If you want, I can now: * Convert these into a **printable PDF** or a **spreadsheet** for easy use; * Expand any selected cases into **full exam-style long cases** (history prompts, viva questions, stepwise management) or **MCQs** derived from these cases; * Produce the **25 MCQs in stylish exam mode** (single HTML file with CSS/JS) instead — tell me which format you prefer next and I’ll produce it immediately. # Anaemia in pregnancy — complete, stylish clinical note > Compact, exam-friendly, evidence-backed reference you can paste into notes or teaching slides. Sources for the most important guideline facts are cited inline. --- ## 1) Definition (WHO) Anaemia = low haemoglobin (Hb) or red-cell mass causing reduced O₂-carrying capacity. **WHO threshold in pregnancy:** **Hb < 110 g/L (11.0 g/dL)** = anaemia; **severe** = **< 70 g/L (7.0 g/dL)**. ([World Health Organization][1]) --- ## 2) Pathophysiology (short) * Pregnancy → plasma volume ↑ ≈ 30–50% while red-cell mass ↑ less → physiologic haemodilution (lower Hb). * Pathologic anaemia results when iron supply (diet + stores) cannot meet increased maternal/fetal demands → reduced haemoglobin synthesis → microcytic hypochromic RBCs (longstanding). * Other mechanisms: haemoglobinopathy, folate/B12 deficiency, chronic inflammation (anemia of chronic disease, ACD), hemolysis, acute blood loss. --- ## 3) Iron requirements in pregnancy & prophylaxis (practical) * Pregnancy increases iron need substantially (for maternal RBC mass, placenta and fetus). Guidelines recommend **daily oral iron 30–60 mg elemental iron + 400 µg folic acid** for routine antenatal prophylaxis (start early, usually from 12 weeks or at first contact per local policy). For treatment, higher elemental doses are used (see below). ([World Health Organization][2]) --- ## 4) Public-health: Anemia Mukt Bharat & IFA logistics (India) * **Anemia Mukt Bharat (NHM)** emphasises six strategic actions including IFA supplementation, deworming, food fortification, testing & treatment, behaviour change and special management of severe cases. Weekly IFA formulations for adolescents/adults vary by group (e.g., 45–60 mg elemental iron + folic acid 400–500 µg for weekly program tablets); pregnant women receive daily IFA through ANC (tablet composition and supply per NHM/ANC). ([National Health Mission][3]) > Note about **“I-NIAP”**: I searched for a standard term “I-NIAP” and could not find an established definition. In obstetric literature you’ll see **AIP / NAIP** (Anemia In Pregnancy / Non-Anemic In Pregnancy) used in studies. If you meant a specific program/term, tell me and I’ll fetch it. ([sid.ir][4]) --- ## 5) Clinical history (what to ask) * Symptoms: fatigue, exertional dyspnoea, palpitations, syncope, orthopea, pica (pagophagia), restless legs, diminished exercise tolerance. * Obstetric: prior PPH, multiple pregnancies, short interpregnancy interval, hyperemesis, dietary restrictions, bleeding (menorrhagia pre-pregnancy), parasites, recent infections. * Drugs: antacids, calcium, tetracyclines (interfere with iron). * Family history: haemoglobinopathies (thalassaemia trait). --- ## 6) Physical examination (key findings) * Pallor (conjunctiva, palmar crease), tachycardia, glossitis, koilonychia (severe chronic), systolic flow murmur, signs of heart failure if severe. Look for hepatosplenomegaly (hemolysis/thalassaemia), lymphadenopathy (chronic disease). --- ## 7) Investigations — how to approach & interpretation **First-line tests** * CBC with RBC indices (Hb, Hct, MCV, MCH, MCHC), reticulocyte count, peripheral smear. * Ferritin (best single test for iron stores unless inflammation present), serum iron, TIBC/transferrin, transferrin saturation. ([MSD Manuals][5]) **Key numbers** * **MCV normal** ≈ 80–100 fL (microcytic <80 fL). (Use lab reference ranges.) ([MSD Manuals][5]) **Mentzer index** (practical discriminator) * **Mentzer = MCV (fL) / RBC count (10^6/µL)**. * **>13 → likely Iron Deficiency Anaemia (IDA)**. * **<13 → likely β-thalassaemia trait**. ([PMC][6]) **Peripheral smear** * IDA: microcytic hypochromic RBCs, anisopoikilocytosis, pencil cells. * ACD: often normocytic or mildly microcytic with low serum iron but low TIBC. Ferritin is normal or high in ACD (acute phase reactant). **Hb electrophoresis** * Indication: to detect β-thalassaemia trait or other hemoglobinopathies when indices suggest trait (normal/high RBC count, low MCV, Mentzer <13). Confirm with HbA₂ levels. ([PMC][7]) **Ferritin interpretation** * Low ferritin confirms iron deficiency; ferritin is raised in inflammation — interpret with CRP/ESR. WHO/technical guidance gives ferritin cutoffs and handling when inflammation present. ([World Health Organization][8]) --- ## 8) IDA vs Anaemia of Chronic Disease (ACD) — key contrasts * **IDA:** low ferritin, low serum iron, high TIBC (or normal), low transferrin saturation; microcytic hypochromic RBCs. * **ACD:** low serum iron, **low/normal TIBC**, normal/high ferritin, low transferrin saturation; usually occurs with infection/inflammation/chronic disease. Treatment targets underlying disease + careful iron management. ([World Health Organization][8]) --- ## 9) Differential diagnoses to consider * Iron deficiency, haemoglobinopathies (thalassaemia trait), folate/B12 deficiency, ACD, hemolytic anaemias, blood loss (antepartum/PPH), bone marrow disorders. --- ## 10) Complications & adverse effects of anaemia in pregnancy **Maternal effects** * Fatigue, reduced work capacity, increased risk of cardiac failure if severe, increased risk of peripartum transfusion and infection, poor wound healing, higher maternal mortality in severe anaemia. ([World Health Organization][9]) **Fetal/neonatal effects** * Preterm birth, low birth weight, intrauterine growth restriction, perinatal mortality, impaired neurodevelopment if severe/untreated. --- ## 11) Management — overview (prevention → treat → rescue) **Goals:** correct Hb, replete iron stores (ferritin), prevent recurrence, avoid transfusion when possible. ### A. Prevention (policy/antenatal) * Diet counselling (iron-rich foods + vitamin C to increase absorption; avoid tea/coffee with meals). * Routine **daily IFA prophylaxis: 30–60 mg elemental iron + 400 µg folic acid** (WHO). For national programs (India) follow Anemia Mukt Bharat / ANC protocols for supply and deworming. ([World Health Organization][2]) ### B. Oral iron — first-line for mild–moderate IDA and prophylaxis **Common salts & elemental iron content (practical)** * **Ferrous sulfate 325 mg** ≈ **65 mg elemental iron** (varies with hydrate). * **Ferrous fumarate 300 mg** ≈ **99–100 mg elemental iron**. * **Ferrous gluconate 300/325 mg** ≈ **35–39 mg elemental iron**. (Check product label.) ([NCBI][10]) **Indication (pregnancy):** treatment when IDA confirmed (mild–moderate), prophylaxis as above. **Dosing (typical)** * **Prophylaxis:** 30–60 mg elemental iron daily + 400 µg folic acid. ([World Health Organization][2]) * **Treatment (common practice):** many formularies use **60–120 mg elemental iron daily** (often given as 1 tab of ferrous sulfate 325 mg × 1–3 daily depending on severity) or **single daily higher elemental dose**; some guidelines/recent studies favour **lower daily doses (e.g., 60–80 mg elemental once daily)** or alternate-day dosing to improve tolerance and absorption — tailor to local guidance and tolerance. ([ScienceDirect][11]) **Mechanism of action:** provides elemental iron for haemoglobin synthesis; absorbed in duodenum via DMT1 after reduction to ferrous form. **Pharmacokinetics (summary):** oral iron variably absorbed (5–30% depending on iron status, enhancers/inhibitors). Food reduces absorption; vitamin C enhances. **Adverse effects (oral):** GI upset, nausea, abdominal pain, constipation or diarrhoea, black stools; adherence often limited by GI side effects. ([National Health Mission][12]) **Contraindications:** known hypersensitivity; caution with hemochromatosis. Check for haemoglobinopathy before prolonged high-dose therapy. **Key interactions:** antacids, calcium, tetracyclines, some antibiotics — separate dosing by 2–3 hours. Vitamin C coadministration improves absorption. **Monitoring:** Hb every 2–4 weeks until rise (aim Hb ↑ by ~1 g/dL in 2–4 weeks), ferritin at baseline and after repletion; monitor adherence and GI side effects. **Counselling points to patient:** take on empty stomach if tolerated (or with small vitamin-C-rich juice), avoid tea/coffee within 1–2 hours, black stools are common and harmless, constipation can be managed with stool softener/diet. Keep out of reach of children (ingestion is toxic). --- ### C. Parenteral (IV) iron — when to use **Indications in pregnancy** * Severe IDA not corrected by oral iron, intolerance or non-adherence to oral iron, late pregnancy where rapid correction needed, malabsorption, ongoing significant bleeding, or when quick Hb rise needed before delivery/cesarean. Avoid routine use in first trimester when possible. ([Wiley Online Library][13]) **Preparations & dosing (practical)** * **Iron sucrose (Venofer):** repeated doses (e.g., 100–200 mg per infusion; typical cumulative calculated by Ganzoni or dosing tables). Max ~200 mg per infusion commonly used; total depends on deficit. ([transfusionguidelines.org][14]) * **Ferric carboxymaltose (FCM; Injectafer/Ferinject):** allows **larger single doses (up to ~750–1000 mg per infusion, product-specific limits ~15–20 mg/kg, max 1000 mg single dose)** — useful to correct iron deficit quickly in 1–2 visits. ([injectaferhcp.com][15]) **Mechanism:** IV complexes deliver iron directly to reticuloendothelial system for incorporation into ferritin/haemoglobin. **Adverse effects (IV):** infusion reactions (including rare anaphylaxis with older dextran formulations), transient hypotension, nausea, arthralgia, local irritation; hypophosphatemia reported with some agents (e.g., FCM). Monitor for hypersensitivity during infusion. ([PMC][16]) **Monitoring:** vitals during infusion, monitor Hb/ferritin 2–4 weeks post infusion; check phosphate if using FCM and high cumulative dose. **Counselling:** explain need for IV access, possible transient side effects, and post-infusion monitoring. --- ### D. Blood transfusion — when & how (obstetric specifics) **Indications:** individualised — combine clinical state and Hb level. Many guidelines say transfusion is usual when **Hb < 60–70 g/L** or if symptomatic/hemodynamically unstable; rarely needed if Hb > 100 g/L. In obstetrics, clinical context (ongoing bleeding, cardiovascular compromise, labour) is decisive. Cross-match and plan ahead for high-risk women. Use single donor PRBCs, match Rh/K testing, and consider component therapy. ([RCOG][17]) **Risks:** transfusion reactions, alloimmunisation, infection risk (low with modern screening), transfusion-associated circulatory overload; plan restrictive transfusion strategy where safe. --- ## 12) Stepwise treatment algorithm (practical summary) 1. **Screen all pregnant women at booking** (Hb + RBC indices). If Hb <110 g/L → further tests (CBC, ferritin ± iron studies). ([World Health Organization][1]) 2. **If IDA confirmed (low ferritin):** start/optimise oral iron (elemental 60–120 mg/day, adjust to tolerance). Counsel. Monitor Hb rise at 2–4 weeks. If inadequate response or very late pregnancy / urgent correction required → **IV iron** (calculate total deficit; consider FCM or iron sucrose per availability). ([ScienceDirect][11]) 3. **If severe symptomatic anaemia (Hb <70 g/L) or haemodynamic instability:** consider blood transfusion (obstetric judgement). ([RCOG][17]) --- ## 13) Prevention of recurrence & antenatal program tips * Give full course until 3 months postpartum if previously anaemic, ensure deworming (in areas endemic for helminths) per national policy, ensure adequate dietary counselling, consider screening for haemoglobinopathies if family history or persistent microcytosis after iron repletion. Use Anemia Mukt Bharat operational modules to plan community IFA distribution and counselling. ([i4n.in][18]) --- ## 14) Quick bedside pocket facts (copy-paste) * **WHO anaemia in pregnancy:** Hb <11.0 g/dL. ([World Health Organization][1]) * **Routine prophylaxis:** **30–60 mg elemental iron + 400 µg folic acid daily.** ([World Health Organization][2]) * **Oral elemental iron examples:** ferrous sulfate 325 mg ≈ 65 mg Fe; ferrous fumarate 300 mg ≈ 99 mg Fe; ferrous gluconate 300 mg ≈ 35 mg Fe. ([NCBI][10]) * **Mentzer index:** MCV/RBC; **>13 → IDA**, **<13 → thalassaemia trait**. ([PMC][6]) --- ## 15) Practical templates (for your notes) **A. ANC counselling line:** “You have mild iron deficiency. I’m starting oral iron (example: ferrous sulfate 325 mg **once daily** = ~65 mg elemental iron) + folic acid — take on empty stomach or with orange juice, expect black stools; call if severe abdominal pain or fainting.” **B. IV iron note:** “Given poor response/intolerance to oral iron or late pregnancy, plan IV ferric carboxymaltose **(calculate total deficit; often one 1000 mg infusion)** — monitor vitals during infusion, check Hb & ferritin at 2–4 weeks.” --- ## 16) References / further reading (selected, guideline-level) * WHO Anaemia fact sheet & Hb thresholds. ([World Health Organization][9]) * WHO recommendations: daily iron & folic acid supplementation in pregnancy. ([World Health Organization][2]) * Anemia Mukt Bharat training & operational guidance (India/NHM). ([National Health Mission][3]) * Mentzer index & RBC indices literature. ([PMC][6]) * IV iron reviews & product dosing (iron sucrose, ferric carboxymaltose) and obstetric use. ([PMC][16]) * RCOG / Green-top on blood transfusion in obstetrics. ([RCOG][17]) --- If you want, I can now: * Convert this into a **stylish one-page printable handout (PDF)**; * Generate **30 case scenarios with management** (you previously asked for many cases) or **25 MCQs in exam mode** with HTML/CSS/JS; * Produce an **SEO title/description/keywords** and **an illustrative image** (I can generate an image for a teaching slide). Tell me which follow-up you want and I’ll produce it in the same detailed style. [1]: https://cdn.who.int/media/docs/default-source/anaemia-in-women-and-children/hb-methods-for-gather.pdf?sfvrsn=da0fbb5f_11&utm_source=chatgpt.com "WHO methods and data sources for mean haemoglobin ..." [2]: https://www.who.int/tools/elena/interventions/daily-iron-pregnancy?utm_source=chatgpt.com "Daily iron and folic acid supplementation during pregnancy" [3]: https://nhm.gov.in/index1.php?lang=1&level=3&lid=797&sublinkid=1448&utm_source=chatgpt.com "Anaemia Mukt Bharat" [4]: https://www.sid.ir/paper/1056249/en?utm_source=chatgpt.com "Haemoglobin Level of Pregnant Women on First ..." [5]: https://www.msdmanuals.com/professional/multimedia/table/typical-normal-serum-values-for-iron-iron-binding-capacity-ferritin-and-transferrin-saturation?utm_source=chatgpt.com "Table: Typical Normal Serum Values for Iron, Iron-Binding ..." [6]: https://pmc.ncbi.nlm.nih.gov/articles/PMC9121960/?utm_source=chatgpt.com "Role of Mentzer index for differentiating iron deficiency ..." [7]: https://pmc.ncbi.nlm.nih.gov/articles/PMC5467296/?utm_source=chatgpt.com "Iron Deficiency Anemia or β-Thalassemia Trait? - PMC" [8]: https://www.who.int/docs/default-source/micronutrients/ferritin-guideline/ferritin-guidelines-brochure.pdf?sfvrsn=76a71b5a_4&utm_source=chatgpt.com "ferritin-guidelines-brochure.pdf" [9]: https://www.who.int/news-room/fact-sheets/detail/anaemia?utm_source=chatgpt.com "Anaemia" [10]: https://www.ncbi.nlm.nih.gov/books/NBK548214/table/Iron.T1/?utm_source=chatgpt.com "[Table, Concentrations of elemental iron in typical iron tablets]" [11]: https://www.sciencedirect.com/science/article/pii/S0098299720300364?utm_source=chatgpt.com "Oral iron supplementation in iron-deficient women" [12]: https://nhm.gov.in/images/pdf/programmes/wifs/guidelines/icds_operational_guidelines_for_wifs.pdf?utm_source=chatgpt.com "Operational Guidelines for Weekly IFA Supplementation ..." [13]: https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.27220?utm_source=chatgpt.com "Expert consensus guidelines: Intravenous iron uses, ..." [14]: https://www.transfusionguidelines.org/document-library/documents/protocol-for-the-use-of-iv-iron-sucrose/download-file/rtc-eeng_protocol_iv_iron_sucrose.pdf?utm_source=chatgpt.com "IV iron sucrose Venofer protocol v1.0 Jan08" [15]: https://injectaferhcp.com/iron-injection-administration?utm_source=chatgpt.com "Dosing and Administration" [16]: https://pmc.ncbi.nlm.nih.gov/articles/PMC9722303/?utm_source=chatgpt.com "Ferric Carboxymaltose in the Management of Iron ..." [17]: https://www.rcog.org.uk/media/sdqcorsf/gtg-47.pdf?utm_source=chatgpt.com "Blood Transfusion in Obstetrics" [18]: https://www.i4n.in/wp-content/uploads/2023/05/Anemia-Mukt-Bharat-Training-Modules-english.pdf?utm_source=chatgpt.com "ANEMIA MUKT BHARAT"
Browse by Medical Category
Explore content organized by medical specialties and systems