Complete guide on anaemia in pregnancy including causes, WHO definition, diagnosis, iron requirements, IFA tablets, NIAP, Anemia Mukt Bharat, treatment & management.
Explore Related Content
- Home Latest medical posts
- Sitelinks Index Complete site map
- Upload Medical Content Share clinical pearls
- More OBSTETRICS AND GYNAECOLOGY Posts Browse related content
- Reviews & Suggestions Community feedback
- Help & FAQ Upload & SEO tips
- More from this Author View all posts
- About Streamora Medical learning hub
Related Posts
Posts with similar category or tags for stronger sitelinks & internal backlinks.
Aneuploidy Screening in Pregnancy: First Trimester, Quadruple Test, NIPT & Soft Markers | Complete Guide 2025
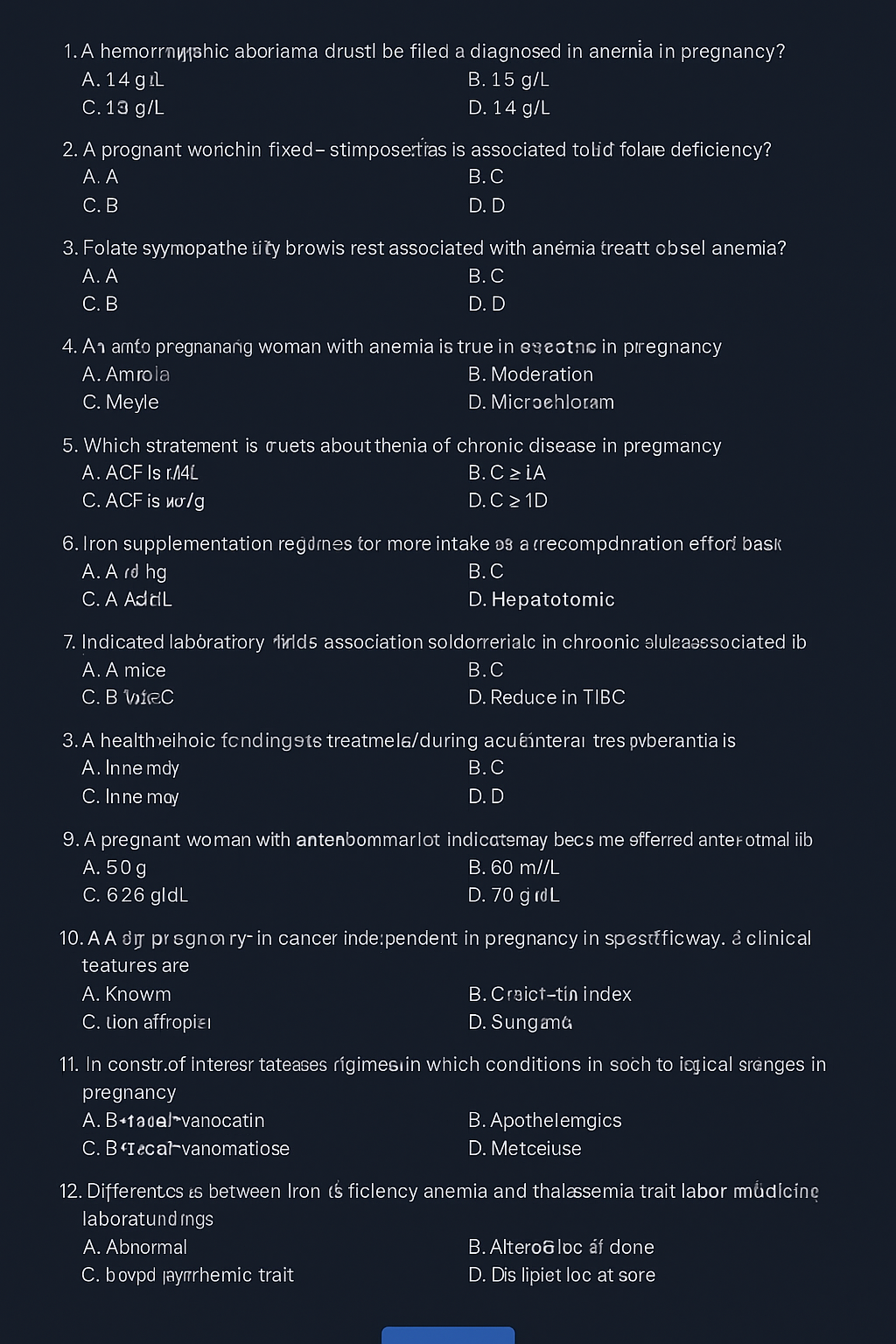
--- # ⭐ **Aneuploidy Screening in Pregnancy — Complete Obstetric Guide** Aneuploidy = **abnormal number of chromosomes** (most clinically relevant: **Trisomy 21, 18, 13**, Turner syndrome). Goal of screening = **identify pregnancies at increased risk** early enough to offer **diagnostic testing**. --- # **1. Why Aneuploidy Occurs (Basic Pathophysiology)** * **Meiotic nondisjunction** → failure of homologous chromosomes/sister chromatids to separate. * **Common in maternal meiosis I** (age-related). * **Trisomy 21 risk increases exponentially with maternal age**. * Mosaicism occurs if nondisjunction happens post-zygotically. --- # **2. High-Risk Factors** * Advanced maternal age (≥35 yrs). * Previous pregnancy with aneuploidy. * Parental balanced translocation (esp. Robertsonian). * Abnormal ultrasound markers (NT ↑, absent nasal bone, echogenic bowel, cardiac defects). * Abnormal biochemical screening results. --- # **3. Overview of Screening Timeline** | Gestation | Test | | ------------------- | ------------------------------------------------------------- | | **11–13+6 weeks** | First-trimester combined screening (NT + PAPP-A + free β-hCG) | | **10 weeks onward** | NIPT / cfDNA (highest accuracy) | | **15–22 weeks** | Second-trimester quadruple test | | **18–22 weeks** | Targeted anomaly scan (soft markers) | **Screening ≠ diagnosis.** Diagnostic tests = **CVS (10–13 wks)**, **Amniocentesis (≥15 wks)**, **FISH/karyotype/microarray**. --- # **4. First-Trimester Screening (11–13+6 Weeks)** ## **Components** 1. **Nuchal translucency (NT):** * Measured at CRL 45–84 mm * **NT >3.5 mm = major risk marker** * Increased NT → Trisomy 21/18/13, cardiac defects, Noonan syndrome, skeletal dysplasias 2. **Biochemical markers:** * **PAPP-A ↓**: Trisomy 21/18, placental insufficiency * **Free β-hCG ↑**: Trisomy 21 * **Free β-hCG ↓**: Trisomy 18/13 ## **Detection rate:** ~85–90% for T21 when combined. --- # **5. NIPT / cfDNA (Non-Invasive Prenatal Testing)** * Can be done **from 10 weeks onward**. * Analyzes **cell-free fetal DNA** in maternal blood. * **Most accurate screening test**. ## **Detects** * **Trisomy 21, 18, 13** * **Sex chromosome aneuploidies** (Turner, Klinefelter) * Microdeletions (low PPV, not recommended routinely) ## **Not diagnostic**, but: * **Sensitivity**: * T21 ≈ 99% * T18 ≈ 97–98% * T13 ≈ 92% ## **Causes of false results** * Confined placental mosaicism * Vanishing twin * Maternal malignancy * Low fetal fraction (<4%) --- # **6. Second-Trimester Quadruple Test (15–22 Weeks)** Markers: * **AFP** * **hCG** * **uE3 (unconjugated estriol)** * **Inhibin-A** ## **Patterns** ### **Trisomy 21** * **AFP ↓** * **uE3 ↓** * **hCG ↑** * **Inhibin-A ↑** ### **Trisomy 18** * **AFP ↓** * **uE3 ↓** * **hCG ↓** * **Inhibin-A normal** ### **Open neural tube defects** * **AFP ↑↑** Detection rate: * **~75% for T21** --- # **7. Ultrasound Soft Markers (18–22 Weeks)** ### **Major structural markers** * Cardiac defects (AV canal) → T21 * Holoprosencephaly → T13 * Omphalocele → T18 * Diaphragmatic hernia * Renal anomalies ### **Soft markers (non-structural)** | Marker | Association | | -------------------------------------- | --------------- | | **Absent nasal bone** | T21 | | **Echogenic intracardiac focus (EIF)** | Mild ↑ T21 risk | | **Echogenic bowel** | T21, CMV, CF | | **Short femur/humerus** | T21 | | **Choroid plexus cyst** | T18 | | **Single umbilical artery** | T18, T13 | | **Mild ventriculomegaly** | Aneuploidy risk | Soft markers **modify risk**, not diagnostic. --- # **8. Integrated & Sequential Screening** ### **Integrated test** * Combines first-trimester + second-trimester results * Highest combined detection before NIPT * Detection: **~94–95%**, but results available only in 2nd trimester ### **Sequential screening** * If first-trimester is high-risk → offer NIPT/CVS * If low-risk → continue with second trimester screening * More practical than integrated approach --- # **9. Diagnostic Tests (When Screening Is Positive)** ## **Chorionic Villus Sampling (CVS)** * **10–13+6 weeks** * Transcervical or transabdominal * Results: karyotype, microarray * Miscarriage risk: **~0.2–0.3%** ## **Amniocentesis** * **≥15 weeks** * Lower miscarriage risk: **0.1–0.2%** ## **Rapid tests** * **FISH** (24–48 hrs): detects T21, T18, T13 * **Microarray**: detects microdeletions/duplications --- # **10. Combined Detection Performance** | Test | Detection rate for T21 | | ------------------------ | ---------------------- | | First trimester combined | 85–90% | | Quadruple test | 75% | | Integrated screening | 94–95% | | **NIPT** | **>99%** | NIPT is **preferred**, especially for high-risk pregnancies. --- # **11. When to Offer NIPT (Indications)** * Maternal age ≥35 yrs * Previous trisomy pregnancy * Abnormal ultrasound markers * Positive biochemical screen * IVF pregnancies (optional but recommended) * Parental chromosomal rearrangement (screening may be inadequate → offer diagnostic test) --- # **12. Management Algorithm (Simplified)** ### **STEP 1: First antenatal visit** * Counsel regarding available screening methods * Offer **NIPT** to all (optimal) ### **STEP 2: If NT scan & biochemistry done** * **High-risk → NIPT or CVS** * **Intermediate risk → NIPT** * **Low risk → routine care** ### **STEP 3: Anomaly scan** * If any major structural abnormality → **Diagnostic test (CVS/Amniocentesis)** irrespective of NIPT result ### **STEP 4: If NIPT positive** * **Never terminate pregnancy based on NIPT alone** * Perform **confirmatory CVS/Amniocentesis** --- # **13. Counseling Points** * Screening ≠ diagnosis * Explain detection rates and false positives * Invasive diagnostic tests carry small miscarriage risks * A normal screen reduces but **does not eliminate** risk * Final decision is patient-centered --- # **14. Key Exam High-Yield Points** * **Most sensitive screening test:** NIPT * **Earliest diagnostic test:** CVS * **Best time for NT scan:** 11–13+6 weeks * **AFP ↑:** NTD, abdominal wall defects, incorrect dating * **AFP ↓ + hCG ↑ + uE3 ↓:** Trisomy 21 * **Choroid plexus cyst:** Trisomy 18 marker * **Absent nasal bone:** Down syndrome strongest soft marker * **Echogenic bowel:** Trisomy 21, CMV, CF ---
Antepartum Fetal Monitoring: Indications, NST, Biophysical Profile, Modified BPP & Vibroacoustic Test | Complete Obstetrics Guide 2025
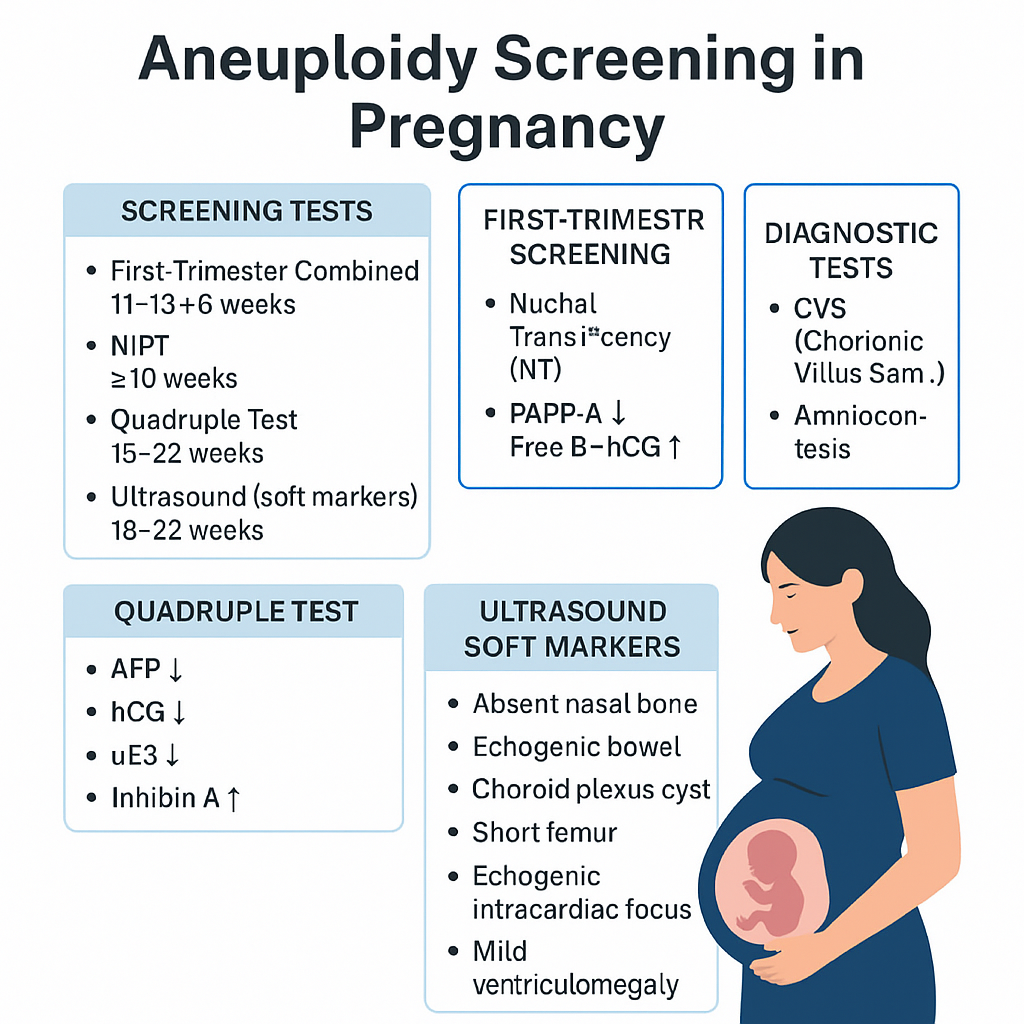
--- # ⭐ **ANTEPARTUM FETAL MONITORING — COMPLETE HIGH-YIELD REFERENCE (NEET PG / INI-CET)** Antepartum fetal surveillance aims to detect **early fetal hypoxia** to prevent stillbirth, reduce perinatal morbidity, and guide timing of delivery. It assesses **placental function**, **oxygenation**, **neurological integrity**, and **fetal compensatory mechanisms**. --- # **1️⃣ Indications for Antepartum Fetal Monitoring** ### **A. Maternal Indications** * **Hypertensive disorders:** Gestational HTN, preeclampsia, eclampsia * **Diabetes mellitus:** GDM requiring insulin/OADs, pre-gestational DM * **Chronic medical diseases:** * Chronic hypertension * Renal disease * Autoimmune disease (SLE, APLA syndrome) * Cardiac disease * Thyroid disease with complications * **Previous obstetric history:** * Previous stillbirth * Previous IUGR baby * Previous neonatal death * Isoimmunization/Rh alloimmunization * **Maternal infections:** TORCH with fetal involvement * **Advanced maternal age (>35)** * **Post-dated pregnancy (>40 weeks)** ### **B. Fetal Indications** * **Decreased fetal movements** * **IUGR (Symmetric/Asymmetric)** * **Oligohydramnios / Polyhydramnios** * **Multiple pregnancy with complications** * **Fetal anemia / hydrops** * **Congenital anomalies** ### **C. Placental Indications** * Placental insufficiency * Marginal/Abnormal cord insertion * Placenta previa with recurrent bleeding --- # **2️⃣ Fetal Movement Count (FMC / Kick Count)** Fetal movements reflect fetal well-being (neurological + metabolic status). ### **Methods** ### **A. Cardiff Count-to-10 Method** * Mother records movements daily. * **Normal:** 10 movements within 12 hours. ### **B. Sadovsky Method** * Count movements for 1 hour after meals. * **Normal:** ≥4 movements/hour. ### **When to worry?** * **<10 movements in 12 hours** * **<4 movements in 1 hour** * **No movement in 2 hours** → urgent evaluation (NST/BPP) ### **Management of Decreased Fetal Movements** 1. Immediate **NST** 2. If NST non-reactive → **BPP** 3. If BPP equivocal → **Doppler studies** 4. If evidence of fetal compromise → **Delivery based on GA** --- # **3️⃣ Non-Stress Test (NST)** NST measures **fetal heart rate accelerations** in response to fetal movements via cardiotocography. ### **Procedure** * Done after **28–32 weeks** (mature autonomic nervous system). * Duration: **20 minutes** (extend to 40 minutes if needed). --- ## **Interpretation (Reactive vs Non-Reactive)** ### ✔ **Reactive NST (Normal)** * **≥2 accelerations** in 20 minutes * Acceleration criteria: * **≥15 bpm for ≥15 sec** (≥32 weeks) * **≥10 bpm for ≥10 sec** (<32 weeks) ### ✔ **Non-Reactive NST** * <2 accelerations in 40 minutes * Suggests fetal sleep cycle, hypoxia, CNS depression. ### **Causes of Non-Reactive NST** * Fetal sleep * Maternal drug intake (MgSO₄, opioids, sedatives) * Hypoxia * Prematurity * Congenital anomalies ### **Next Steps in Non-Reactive NST** * Vibroacoustic stimulation test * BPP * Contraction stress test (rarely used today) * Doppler studies --- # **4️⃣ Vibroacoustic Stimulation Test (VAST)** Used to differentiate fetal sleep from hypoxia in non-reactive NST. ### **Method** * A vibrating device (artificial larynx) applied to maternal abdomen for **1–3 seconds**. ### **Normal Response** * FHR acceleration within **15 seconds** * Converts non-reactive NST → **reactive** ### **Significance** * High negative predictive value * Reduces need for BPP --- # **5️⃣ Biophysical Profile (BPP) / Manning Score** Combines **NST + ultrasound parameters** assessing fetal CNS integrity + oxygenation. ### **Components (Total 10 points)** Each gets **2 = normal**, **0 = abnormal** | Component | Normal Criteria (2 points) | | ------------------------------ | --------------------------------- | | **NST** | Reactive | | **Fetal breathing** | ≥30 sec in 30 min | | **Gross body movement** | ≥3 movements | | **Fetal tone** | ≥1 extension–flexion cycle | | **Amniotic Fluid Index (AFI)** | AFI ≥5 cm OR deepest pocket ≥2 cm | --- ## **Scoring & Interpretation** | Score | Interpretation | Management | | -------- | -------------- | ------------------------------------------- | | **8–10** | Normal | Routine monitoring | | **6** | Equivocal | Repeat BPP in 24 hrs; evaluate Doppler | | **4** | Abnormal | Risk of fetal hypoxia → Delivery if ≥34 wks | | **0–2** | Severe hypoxia | Immediate delivery | --- # **6️⃣ Modified Biophysical Profile (mBPP)** Simplified & widely used. ### **Components** 1. **NST** 2. **AFI (Amniotic Fluid Index)** ### **Interpretation** * **Normal:** Reactive NST + AFI ≥5 cm * **Abnormal:** * Non-reactive NST * AFI <5 cm (Oligohydramnios) → placental insufficiency ### **Management** * If abnormal mBPP → full BPP or Doppler; consider delivery based on GA. --- # **7️⃣ Contraction Stress Test (OBSOLETE mostly)** Assesses fetal response to **uterine contractions** → risk of late decelerations. Rarely done due to risk + availability of Doppler and BPP. --- # **8️⃣ Putting It All Together — Management Algorithm** ### **Decreased fetal movements →** 1. **NST** 2. If reactive → reassure 3. If non-reactive → repeat + VAST 4. If still non-reactive → BPP 5. * **BPP ≤4** → Delivery * **BPP 6** → Repeat in 24 hrs * **BPP 8–10** → Continue routine follow-ups 6. Assess **AFI, Doppler, maternal condition** --- # **9️⃣ Important Clinical Correlations** ### **NST becomes abnormal earliest in fetal hypoxia** CNS activity reduces → loss of accelerations. ### **BPP components lost in sequence during hypoxia (Late → Early loss)** 1. **NST** 2. **Fetal breathing** 3. **Gross movement** 4. **Fetal tone** (last to disappear) 5. **AFI reduced** from chronic utero-placental insufficiency ### **AFI is chronic marker**; NST is acute marker. --- # ⭐ **HIGH-YIELD VALUES (MUST REVISE)** * Reactive NST: **≥2 accelerations** (15 × 15) * Tone: 1 flexion–extension * Breathing: ≥1 episode ≥30 sec * Movement: ≥3 body movements * AFI: Normal ≥5 cm * Modified BPP = NST + AFI * Sleep cycle: **20–40 min** → extend NST to 40 min --- --- # ⭐ **25 CASE SCENARIOS WITH DETAILED MANAGEMENT** *(Antepartum Fetal Surveillance: FMC, NST, BPP, VAST, mBPP)* --- # **1️⃣ Case Scenario – Decreased Fetal Movements at 34 Weeks** A 28-year-old G2P1 at 34 weeks reports **no fetal movements for 8 hours**. ### **Management** 1. Immediate **NST** 2. If **reactive** → reassure, daily kick count 3. If **non-reactive** → extend to 40 min 4. If still non-reactive → **VAST** 5. If remains non-reactive → **BPP** 6. * **BPP ≥8** → Follow-up * **BPP ≤4** → Deliver based on GA --- # **2️⃣ Case Scenario – Non-Reactive NST in a Diabetic Mother** GDM on insulin at 36 weeks undergoes NST → **non-reactive** after 40 minutes. ### **Management** 1. Perform **VAST** 2. If reactive → repeat NST in 1 week 3. If still non-reactive → **Full BPP** 4. If BPP score **≤4** → Plan delivery 5. Assess **AFI & Doppler** for placental insufficiency --- # **3️⃣ Case Scenario – Oligohydramnios with IUGR** 30-year-old at 32 weeks with **AFI = 4 cm**, EFW <10th percentile. ### **Management** 1. Start **modified BPP (NST + AFI)** 2. Daily NST 3. Doppler: **Umbilical artery S/D ratio** 4. If AEDF/REDF → **Immediate delivery** 5. If NST non-reactive → full BPP 6. Steroids if <34 weeks --- # **4️⃣ Case – Post-Dated Pregnancy (41 Weeks)** Patient at 41+2 weeks shows decreased fetal movement. ### **Management** 1. **NST + AFI** 2. If NST reactive & AFI normal → induce labour within 24–48 hrs 3. If NST non-reactive → BPP 4. BPP ≤6 → Deliver 5. Continuous intrapartum monitoring --- # **5️⃣ Case – Preeclampsia with Severe Features** 32 weeks, BP 160/110, proteinuria +++, fetus active. ### **Management** 1. Daily **NST** 2. Twice-weekly **BPP** 3. Doppler (UA + MCA) weekly 4. Magnesium sulfate for seizure prophylaxis 5. Deliver at 34 weeks or earlier if fetal compromise --- # **6️⃣ Case – Chronic Hypertension with Reduced Movements** 35-year-old with chronic HTN reports <4 kicks in 1 hr. ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. If AFI <5 → suspect placental insufficiency 4. Admit, daily surveillance 5. Deliver if BPP ≤4 or Doppler abnormal --- # **7️⃣ Case – IUGR with Normal NST** 29 weeks, IUGR but **reactive NST**. ### **Management** 1. Continue **twice-weekly NST** 2. Weekly Doppler (UA/ MCA/ CPR ratio) 3. Growth scan every 2 weeks 4. Deliver if Doppler deteriorates or NST becomes abnormal --- # **8️⃣ Case – Polyhydramnios with GDM** 30-year-old with polyhydramnios, NST reactive. ### **Management** 1. Twice-weekly NST 2. AFI monitoring 3. Doppler weekly 4. Induce at 38–39 weeks 5. Prepare for shoulder dystocia risk --- # **9️⃣ Case – Decreased Fetal Movement in Obese Mother** NST shows **baseline variability minimal**. ### **Management** 1. Rule out maternal meds, sleep cycle 2. Extend NST + VAST 3. If still abnormal → BPP 4. Deliver if BPP ≤4 --- # **🔟 Case – Rh-Isoimmunization** 28 weeks, MCA PSV >1.5 MOM (fetal anemia suspected). ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. Plan **intrauterine transfusion** 4. After IUT: Daily NST --- # **1️⃣1️⃣ Case – Twin Pregnancy with Growth Discordance** NST non-reactive for smaller twin. ### **Management** 1. VAST 2. If still non-reactive → BPP for each twin 3. Doppler UA/MCA/ Ductus venosus 4. Deliver if evidence of compromise --- # **1️⃣2️⃣ Case – Maternal Hypoglycemia Before NST** NST shows no accelerations. ### **Management** 1. Give oral glucose 2. Repeat NST 3. If becomes reactive → normal 4. If persistently non-reactive → VAST → BPP --- # **1️⃣3️⃣ Case – Placental Abruption Suspicion** Pain + bleeding + reduced movements. ### **Management** 1. **Immediate NST** 2. If late decelerations / bradycardia → **Immediate delivery** 3. Stabilize mother --- # **1️⃣4️⃣ Case – COVID Positive Mother with Decreased Movements** NST non-reactive. ### **Management** 1. Rule out maternal fever, hypoxia 2. Oxygen + hydration 3. VAST 4. If still non-reactive → BPP 5. Deliver if fetal compromise --- # **1️⃣5️⃣ Case – Smoking Mother with IUGR** NST shows decreased variability. ### **Management** 1. VAST 2. BPP 3. Doppler UA 4. Nicotine cessation + fetal surveillance every 2–3 days --- # **1️⃣6️⃣ Case – Absent Fetal Breathing on BPP** BPP = 6/10 (breathing absent). ### **Management** 1. Repeat BPP in 24 hrs 2. If repeat BPP ≤6 → Deliver 3. Continuous NST monitoring --- # **1️⃣7️⃣ Case – Low AFI but Reactive NST** AFI = 4 cm at 37 weeks. ### **Management** 1. Diagnose **oligohydramnios** 2. Admit, hydration 3. Modified BPP daily 4. Deliver at 37–38 weeks --- # **1️⃣8️⃣ Case – Maternal Seizure on MgSO₄** NST shows minimal variability (drug effect). ### **Management** 1. Continue monitoring 2. Do not interpret variability during MgSO₄ therapy 3. Use **BPP** instead of NST --- # **1️⃣9️⃣ Case – Poorly Controlled Diabetes** 36 weeks, polyhydramnios + macrosomia. ### **Management** 1. NST every 2–3 days 2. Weekly BPP 3. Deliver at 38 weeks 4. Prepare for shoulder dystocia --- # **2️⃣0️⃣ Case – Maternal Dehydration** NST non-reactive. ### **Management** 1. Give IV fluids 2. Repeat NST 3. If reactive → dehydration cause 4. If persists → BPP --- # **2️⃣1️⃣ Case – Postpartum Hemorrhage Risk Mother** Placenta previa major. ### **Management** 1. Weekly NST 2. BPP if NST abnormal 3. Plan elective C-section at 36–37 weeks --- # **2️⃣2️⃣ Case – Fetal Tachycardia** FHR 170 bpm in NST. ### **Management** 1. Exclude maternal fever, dehydration, drugs 2. Treat maternal cause 3. If persists → BPP + Doppler 4. Consider delivery if fetal compromise --- # **2️⃣3️⃣ Case – Mother on Sedatives** NST non-reactive. ### **Management** 1. Document medication effect 2. Perform BPP instead of repeating NST 3. Reassure if BPP normal --- # **2️⃣4️⃣ Case – Sudden IUD Suspicion** No FHR detected in NST. ### **Management** 1. Confirm with ultrasound 2. Evaluate cause (abruption, cord accident) 3. Manage according to GA and maternal stability --- # **2️⃣5️⃣ Case – Preterm (<32 Weeks) Non-Reactive NST** At 30 weeks, NST non-reactive. ### **Management** 1. Extend NST to 40 min 2. Apply VAST 3. If still non-reactive → BPP 4. If BPP ≤4 → Deliver after steroid cover 5. If BPP normal → prematurity likely cause ---
Intrapartum Fetal Monitoring: CTG Interpretation, Decelerations, Sinusoidal Pattern & Complete Management Guide 2025
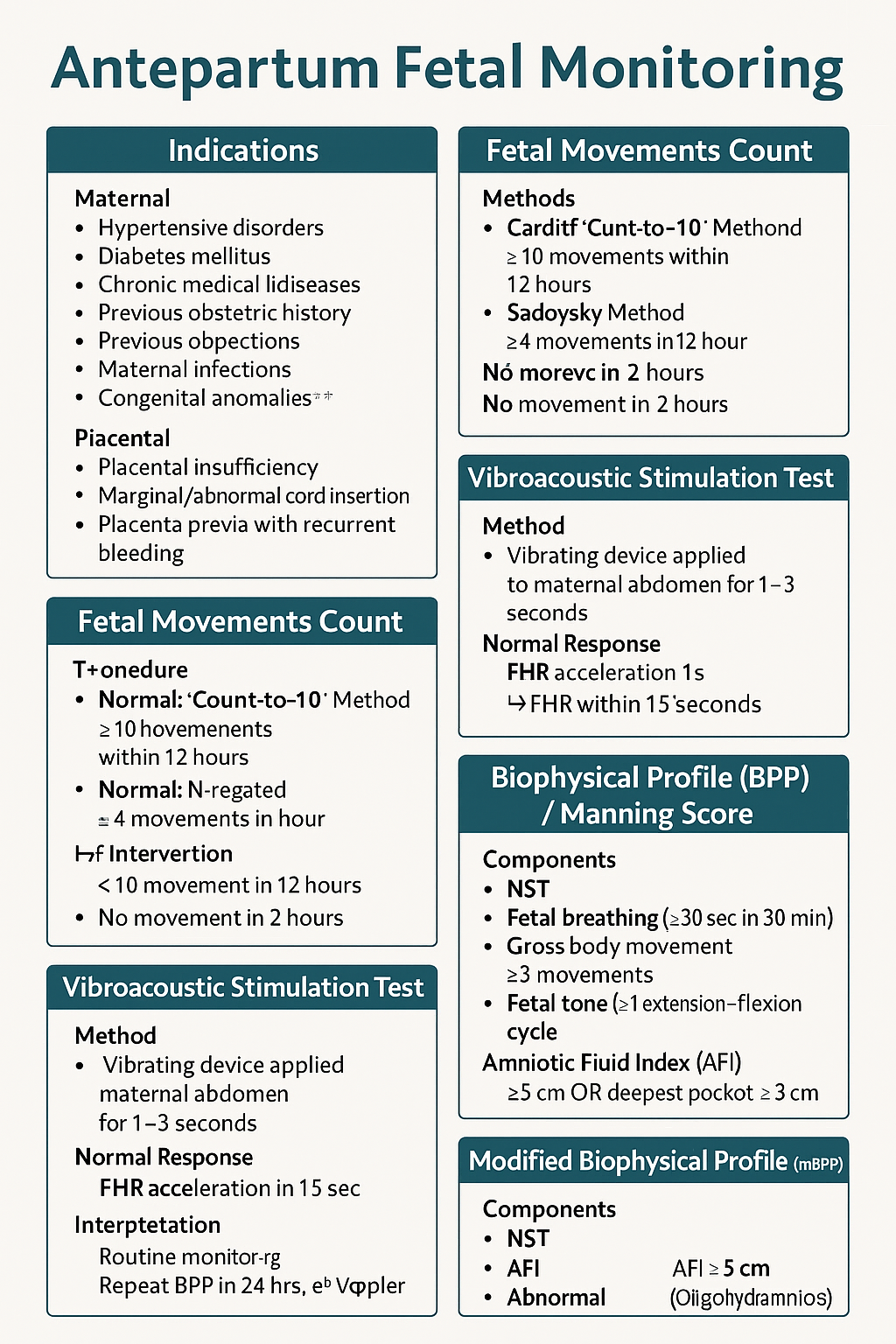
Below are **30 detailed intrapartum fetal monitoring case scenarios with complete management**, written in **NEET PG / INI-CET exam style**. Each scenario includes **clinical context → CTG finding → diagnosis → step-wise management**. --- # ✅ **30 CASE SCENARIOS WITH DETAILED MANAGEMENT (Intrapartum Fetal Monitoring)** --- ## **1️⃣ Case — Late Decelerations in a Preeclamptic Mother** A 25-year-old primigravida, 4 cm dilated, on oxytocin. CTG shows **recurrent late decelerations**, baseline 150, variability <5 bpm. ### **Diagnosis** Uteroplacental insufficiency from **preeclampsia + hyperstimulation**. ### **Management** 1. Stop oxytocin 2. Left lateral position 3. IV fluids 4. If contraction frequency >5/10 min → **tocolysis (terbutaline 0.25 mg SC)** 5. If no improvement → **FBS** 6. If pH <7.20 or tracing deteriorates → **Emergency LSCS** --- ## **2️⃣ Case — Variable Decelerations with Oligohydramnios** G2P1, term labor, CTG shows **variable decelerations with shoulders**, adequate variability. ### **Diagnosis** Cord compression due to oligohydramnios. ### **Management** 1. Maternal repositioning 2. Amnioinfusion 3. Continue labor if variability normal 4. If severe recurrent variables + loss of variability → expedite delivery --- ## **3️⃣ Case — Sinusoidal Pattern** Rh-negative woman, fetus 38 weeks. CTG: **true sinusoidal pattern**. ### **Diagnosis** Severe fetal anemia. ### **Management** 1. Immediate evaluation (Kleihauer test, ultrasound MCA Doppler if time permits) 2. **Emergency LSCS** 3. Prepare NICU for transfusion --- ## **4️⃣ Case — Prolonged Deceleration from Cord Prolapse** During vaginal exam, a loop of cord felt. CTG shows **bradycardia at 80 bpm** for 4 minutes. ### **Management** 1. Lift presenting part manually 2. Knee–chest position 3. Call for emergency LSCS 4. Warm sterile saline-soaked gauze to prevent vasospasm 5. Deliver within **<30 minutes** --- ## **5️⃣ Case — Tachysystole-Induced Late Decelerations** Oxytocin infusion running, contractions 6/10 min. CTG: recurrent late decels. ### **Management** 1. Stop oxytocin immediately 2. Terbutaline 0.25 mg SC 3. Lateral position 4. Reassess 5. If persists → expedite delivery --- ## **6️⃣ Case — Minimal Variability for 50 Minutes** Primigravida in active labor. CTG: baseline 140, variability <5 bpm for 50 min, no decels. ### **Diagnosis** Non-reassuring CTG, possibly fetal sleep or medication effect. ### **Management** 1. Scalp stimulation 2. If acceleration present → reassuring 3. If absent → FBS or continuous monitoring 4. Continue labor if other parameters normal --- ## **7️⃣ Case — Meconium-Stained Liquor with Abnormal CTG** Thick meconium + variable decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. Amnioinfusion (if available) 3. Prepare for operative delivery 4. NICU standby for Meconium Aspiration Syndrome --- ## **8️⃣ Case — Prolonged Deceleration After Epidural** Immediately after epidural, FHR drops to 90 bpm for 3 minutes. ### **Diagnosis** Maternal hypotension causing decreased uteroplacental flow. ### **Management** 1. Left lateral position 2. IV fluid bolus 3. Vasopressor (phenylephrine preferred) 4. If persists beyond 5 minutes → consider LSCS --- ## **9️⃣ Case — Fetal Tachycardia with Maternal Fever** CTG shows FHR 180 bpm, moderate variability; maternal temp 101°F. ### **Diagnosis** Chorioamnionitis. ### **Management** 1. Broad-spectrum antibiotics 2. Acetaminophen 3. Expedite delivery (not LSCS solely for fever) 4. Avoid prolonged labor --- ## **🔟 Case — Arrest of Descent + Late Decelerations** Second stage, fully dilated, prolonged pushing, late decels appear. ### **Management** 1. Check for instrumental eligibility 2. **Forceps or vacuum** if head low 3. If not eligible → emergency LSCS --- ## **1️⃣1️⃣ Case — Recurrent Severe Variable Decelerations** CTG: variable decels dropping to 70 bpm for 60–90 sec. ### **Management** 1. Lateral positioning 2. Amnioinfusion 3. Reduce contractions if tachysystole 4. If persistent → operative delivery --- ## **1️⃣2️⃣ Case — Fetal Scalp pH Borderline** FBS pH = 7.22. ### **Management** 1. Correct reversible causes 2. Repeat FBS in 30 min 3. If worsens → expedite delivery --- ## **1️⃣3️⃣ Case — Loss of Variability with Bradycardia** Baseline 90 bpm, absent variability. ### **Diagnosis** Advanced fetal hypoxia. ### **Management** 1. Immediate decision for LSCS 2. No role of waiting or FBS --- ## **1️⃣4️⃣ Case — CTG Unable to Trace Due to Obesity** During labor, external CTG poor quality. ### **Management** 1. Switch to **fetal scalp electrode (FSE)** 2. Use IUPC for contraction monitoring 3. Continue labor normally if FHR normal --- ## **1️⃣5️⃣ Case — Category III CTG in Trial of Labor After Cesarean (TOLAC)** Late decels + minimal variability + scar tenderness. ### **Diagnosis** Scar rupture suspected. ### **Management** 1. Immediate emergency LSCS 2. Do NOT attempt instrumental delivery --- ## **1️⃣6️⃣ Case — Hyperstimulation Causing Decelerations** Misoprostol induction; CTG shows tachysystole + decels. ### **Management** 1. Stop prostaglandin 2. Tocolysis 3. Continuous monitoring 4. If fetal distress → emergency delivery --- ## **1️⃣7️⃣ Case — True Sinusoidal Pattern from Fetomaternal Hemorrhage** CTG sinusoidal; Kleihauer test positive. ### **Management** 1. Emergency delivery 2. Neonatal transfusion preparation --- ## **1️⃣8️⃣ Case — Prolonged Decel During Second Stage** Mother pushing vigorously; CTG shows bradycardia. ### **Management** 1. Stop pushing 2. Reassess for instrument delivery 3. If head + station → vacuum/forceps 4. Otherwise → LSCS --- ## **1️⃣9️⃣ Case — Mild Variable Decelerations with Normal Variability** Intermittent variables, contraction-associated. ### **Management** 1. Reassurance 2. Continue monitoring No intervention required. --- ## **2️⃣0️⃣ Case — Shoulder Dystocia + Bradycardia** Delivery nearly complete, FHR falls to 70 bpm. ### **Management** 1. McRoberts + suprapubic pressure 2. Deliver shoulders quickly 3. Neonatal resuscitation readiness --- ## **2️⃣1️⃣ Case — Cord Around Neck Detected on Ultrasound Before Labor** During labor → variable decels appear. ### **Management** 1. Continue monitoring 2. If severe or persistent → expedite delivery 3. Do not intervene solely for nuchal cord --- ## **2️⃣2️⃣ Case — Prolapsed Cord in Breech** CTG severe bradycardia. ### **Management** 1. Knee–chest position 2. Manual elevation of presenting part 3. Emergency LSCS --- ## **2️⃣3️⃣ Case — Minimal Variability from Opioid Analgesia** Given pethidine 15 min ago; variability <5. ### **Management** 1. Observe for 30–60 min 2. If variability recovers → continue 3. If not → evaluate for fetal hypoxia --- ## **2️⃣4️⃣ Case — Reassuring CTG in Low-Risk Labor** Baseline 140, variability 10, accelerations present. ### **Management** Continue routine monitoring. --- ## **2️⃣5️⃣ Case — Excessive Maternal Dehydration** CTG shows fetal tachycardia 170 bpm. ### **Management** 1. IV fluid bolus 2. Assess maternal vitals 3. Continue monitoring --- ## **2️⃣6️⃣ Case — Placental Abruption Suspected** Pain + bleeding + fetal tachycardia → later bradycardia. ### **Management** 1. Stabilize mother 2. Immediate LSCS if fetus alive 3. Vaginal delivery only if imminent --- ## **2️⃣7️⃣ Case — IUGR Baby with Recurrent Late Decelerations** CTG: late decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. No role for prolonged labor 3. **Expedite delivery** --- ## **2️⃣8️⃣ Case — Maternal Seizure (Eclampsia)** CTG: prolonged decel. ### **Management** 1. Stabilize mother (MgSO₄, airway) 2. Left lateral position 3. If fetal recovery absent → LSCS --- ## **2️⃣9️⃣ Case — Vaginal Birth After Multiple Variables** CTG mostly reassuring except mild variables. ### **Management** 1. Continue monitoring 2. Check for cord issues 3. No intervention unless severe --- ## **3️⃣0️⃣ Case — Failure of Fetal Response to Scalp Stimulation** Minimal variability, no acceleration after stimulation. ### **Diagnosis** Hypoxia suspected. ### **Management** 1. FBS if available 2. If pH abnormal → immediate delivery 3. If not available → treat as pathological CTG → expedite delivery --- If you want, I can also produce: ✅ **HTML + CSS + JS EXAM MODE MCQs (25/30/50)** ✅ **SEO title/description/keywords** ✅ **A medical diagram image for intrapartum fetal monitoring** Just say **“generate MCQs”**, **“generate image”**, or **“give SEO”**. Below is your **complete, concise-but-exhaustive master reference** on **Intrapartum Fetal Monitoring** — fully aligned with NEET PG / INI-CET high-yield requirements. --- # ⭐ **INTRAPARTUM FETAL MONITORING — COMPLETE DETAILED NOTES (2025)** --- ## **1️⃣ Factors Affecting Fetal Oxygenation During Labor** Fetal oxygenation depends on uninterrupted flow across **four levels**: ### **A. Maternal Factors** * **Maternal oxygenation:** Hypoxia, severe anemia, pulmonary disease. * **Uterine perfusion:** Hypotension (epidural, hemorrhage), dehydration, aortocaval compression. * **Uterine hyperactivity:** Tachysystole (>5 contractions/10 min), hypertonus ↓ intervillous blood flow. * **Drugs:** β-agonists ↑ fetal tachycardia; opioids ↓ variability. ### **B. Uteroplacental Factors** * Placental insufficiency (hypertension, preeclampsia, post-maturity). * Placental abruption, infarction, previa, accreta spectrum. * Umbilical cord compression (oligohydramnios, cord prolapse, tight nuchal cord). ### **C. Fetal Factors** * Fetal anemia, infections, acidosis. * Congenital anomalies (especially CNS, cardiac). * Prematurity → reduced variability. ### **D. Intrinsic Physiological Factors** * Autonomic nervous system balance (sympathetic/parasympathetic). * Fetal behavioral states (quiet sleep cycles ↓ variability). --- ## **2️⃣ Methods of Intrapartum Fetal Surveillance** ### **A. Intermittent Auscultation (IA)** * Using **Pinard stethoscope** or **Doppler**. * Low-risk pregnancies. * Frequency: * **1st stage:** every 30 min * **2nd stage:** every 5 min * Look for: baseline, accelerations, decelerations. ### **B. Continuous Electronic Fetal Monitoring (EFM / CTG)** * External US transducer + tocodynamometer. * Internal scaling: scalp electrode + IUPC (intrauterine pressure catheter) when needed. ### **C. Fetal Scalp Stimulation** * Acceleration after stimulation → reassuring (pH > 7.2). ### **D. Fetal Scalp Blood Sampling (FBS)** → Direct measure of fetal acid-base status. * **Normal pH ≥ 7.25** * **Borderline 7.21–7.24** * **Abnormal < 7.20** → urgent delivery. ### **E. ST-Analysis of Fetal ECG (STAN)** * Detects myocardial hypoxia (ST changes). * Used with CTG. ### **F. Fetal Pulse Oximetry (rare)** * Reassurance if SpO₂ > 30%. ### **G. Vibroacoustic Stimulation** * Sound stimulus → acceleration = good oxygenation. --- ## **3️⃣ Cardiotocography (CTG) – Complete Interpretation** CTG has **5 components**: **Baseline, Variability, Accelerations, Decelerations, Contractions.** --- ## **3.1 Baseline Fetal Heart Rate** Normal: **110–160 bpm** ### **Tachycardia (>160 bpm) causes:** * Maternal fever (chorioamnionitis) * Fetal hypoxia early * Fetal anemia * Drugs: β-agonists, atropine ### **Bradycardia (<110 bpm) causes:** * Vagal stimulation (head compression) * Cord compression * Prolonged deceleration → late sign of hypoxia --- ## **3.2 Baseline Variability (BV)** Reflects fetal autonomic integrity. | **Type** | **Range** | **Significance** | | --------------------- | ------------ | ------------------------------------------ | | Absent | 0 bpm | Severe hypoxia, acidosis, drugs | | Minimal | <5 bpm | Sleep cycle, opioids, prematurity, hypoxia | | **Moderate (Normal)** | **6–25 bpm** | Good oxygenation | | Marked | >25 bpm | Early hypoxia, cord compression | --- ## **3.3 Accelerations** * Abrupt ↑ in FHR by ≥15 bpm for ≥15 sec. * **Reassuring sign** → fetal well-being. --- ## **3.4 Decelerations — Types & Complete Interpretation** ### **A. Early Decelerations** * Mirror contractions. * Due to **head compression**. * **Benign, no treatment.** ### **B. Late Decelerations** * Begin after the contraction peak → return after contraction ends. * Due to **uteroplacental insufficiency**. * **Always concerning**, esp. with absent variability. ### **C. Variable Decelerations** * Abrupt fall in FHR, variable shape. * Due to **cord compression**. * May have "shoulders" (pre- & post-acceleration). * Severe if >60 bpm drop lasting >60 sec. ### **D. Prolonged Deceleration** * FHR drop ≥15 bpm lasting **2–10 min**. * > 10 min = change in baseline. ### **E. Sinusoidal Pattern (MOST IMPORTANT)** **True Sinusoidal Pattern** * Smooth, regular, sine-wave oscillation (3–5 cycles/min) * Amplitude 5–15 bpm * No variability, no accelerations * **Causes:** * Severe fetal anemia (Rh isoimmunization, fetomaternal hemorrhage) * Twin-to-twin transfusion * Hypoxia late stage * **Immediate delivery required** **Pseudo-sinusoidal:** * Seen with opioids — benign. --- ## **4️⃣ NICE 2024 Categories of CTG Interpretation** | Category | Findings | Action | | ------------------------------- | -------------------------------------------------------- | ------------------------------------------------ | | **Normal (Category I)** | Baseline 110–160, Variability 6–25, No repetitive decels | Continue | | **Suspicious (Category II)** | One non-reassuring feature | Correct reversible causes, close monitoring | | **Pathological (Category III)** | ≥1 abnormal feature OR ≥2 non-reassuring | Immediate evaluation, FBS, or expedited delivery | ### **Features** **Reassuring:** * Baseline 110–160 * Variability 6–25 * No decelerations / early decels * Accelerations present **Non-reassuring:** * Baseline 100–109 or 161–180 * Variability <5 for 40–90 min * Variable decels with features * Single prolonged decel <3 min **Abnormal:** * Baseline <100 or >180 * Variability <5 for >90 min * Late decels / prolonged decels >3 min * Sinusoidal pattern --- ## **5️⃣ Management of Abnormal CTG** ### **A. Correct Reversible Causes** * Left lateral position * IV fluids → treat maternal hypotension * Stop oxytocin (if tachysystole) * Tocolysis if uterine hyperstimulation (Terbutaline 0.25 mg SC) * Oxygen (only if maternal hypoxia) ### **B. Fetal Assessment** * Fetal scalp stimulation * FBS (pH or lactate) ### **C. Delivery** * If pH <7.20 OR pathological CTG persists * Emergency LSCS or instrumental delivery depending on stage --- ## **6️⃣ Other Methods of Intrapartum Monitoring** ### **A. Intrauterine Pressure Catheter (IUPC)** * Measures **Montevideo units** * Adequate labor: **>200 MVU** ### **B. Fetal Scalp Electrode (FSE)** * Accurate beat-to-beat FHR * Used when external CTG is poor. ### **C. Meconium-stained liquor evaluation** * Thick meconium + abnormal CTG → intrapartum hypoxia risk. ### **D. Lactate Monitoring** * Fetal scalp lactate <4.8 mmol/L reassuring. --- ## **7️⃣ Quick High-Yield Revision Table** | Topic | Key Points | | ------------------------------- | ------------------------------- | | Best indicator of fetal hypoxia | **Reduced variability** | | Worst CTG sign | **Sinusoidal pattern** | | Earliest sign of hypoxia | **Tachycardia** | | Most common deceleration | **Variable (cord compression)** | --- If you want, I can also generate: ✅ SEO title, description & keywords ✅ 25 hard case-based MCQs (HTML + CSS + JS EXAM MODE) ✅ 25 case scenarios with management ✅ Medical diagram image (via image generator) Just tell me **“continue”** with what you need.
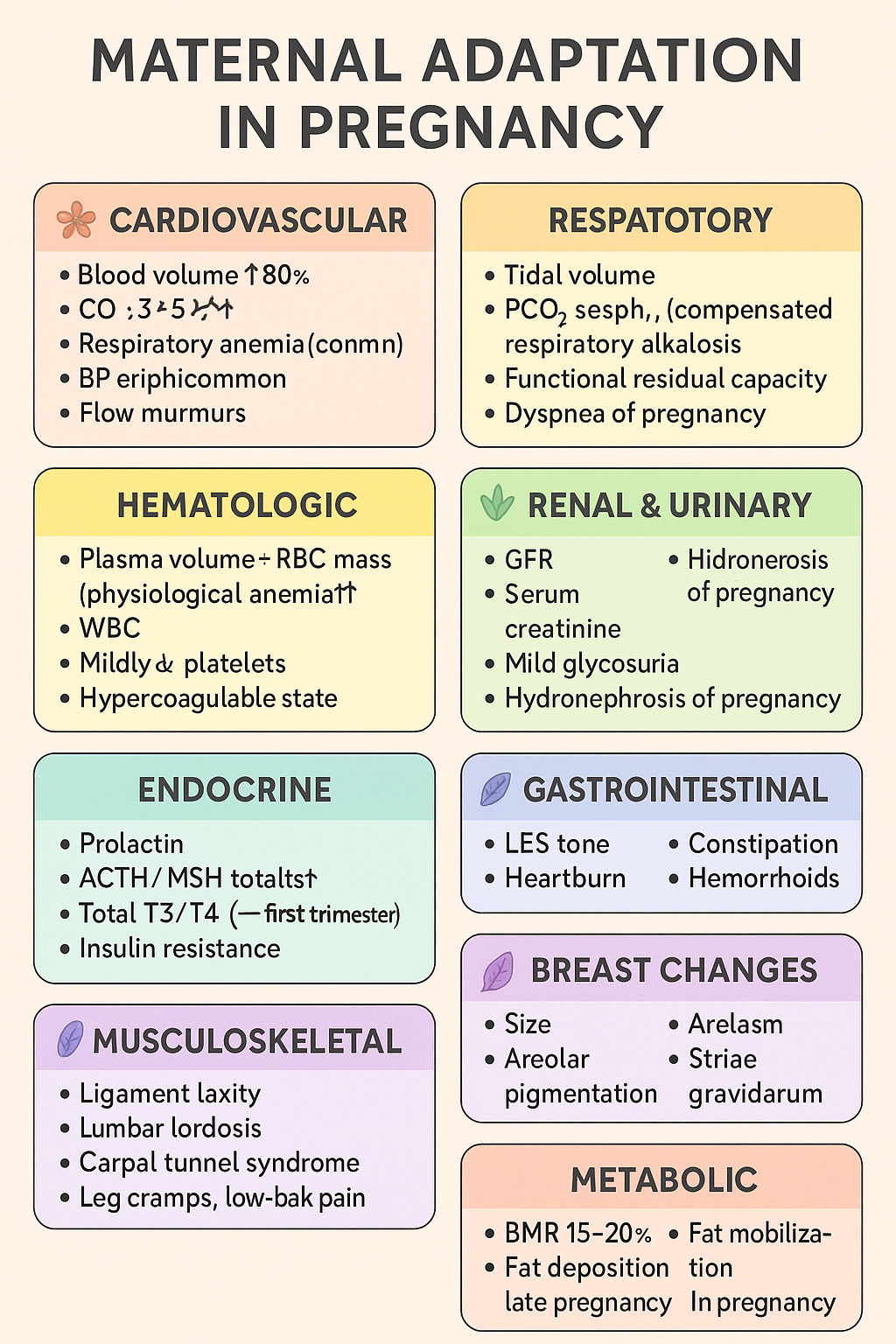
Maternal Adaptations in Pregnancy: Cardiovascular, Respiratory, Renal, Endocrine & Hematologic Changes | Complete Obstetrics Guide 2025
Below is your **complete, crisp but exhaustive stylish note** on **MATERNAL ADAPTATION IN PREGNANCY** — perfect for **NEET PG / INI-CET** and LWT article publishing. Presented in **high-yield, section-boxed format**. --- # ⭐ **MATERNAL ADAPTATIONS IN PREGNANCY — COMPLETE STYLISH NOTE (2025)** Pregnancy induces **multi-system physiologic adaptations** to support fetal growth, prepare for labor, and protect the mother from hemodynamic stresses. --- ## 🌸 **1. Cardiovascular Adaptations** ### 🔹 *Changes* * **Blood volume ↑ 40–50%** (plasma ↑ > RBC mass ↑ → *physiological anemia*). * **CO ↑ 30–50%** → peaks at 20–24 weeks. * **HR ↑ 10–20 bpm**. * **Systemic vascular resistance ↓** (progesterone-mediated vasodilation). * **BP ↓ in 2nd trimester**, returns to baseline in 3rd. * **Peripheral edema common** due to venous compression by gravid uterus. * **Flow murmurs, S3 may appear**. ### 🔹 *Clinical significance* * ↑ preload → protects from blood loss during delivery. * Supine position → **supine hypotension syndrome** (IVC compression). * Murmurs usually benign; still evaluate if symptomatic. --- ## 🌸 **2. Respiratory Adaptations** ### 🔹 *Changes* * **Tidal volume ↑ 30–40%**, minute ventilation ↑. * **PCO₂ ↓ → respiratory alkalosis (compensated)**. * **Functional residual capacity ↓** (diaphragm elevation by 4 cm). * **Dyspnea of pregnancy common** (physiological). ### 🔹 *Clinical significance* * Low PCO₂ → facilitates **placental CO₂ transfer**. * Increased ventilation → improved oxygenation for fetus. --- ## 🌸 **3. Hematologic Adaptations** ### 🔹 *Changes* * **Plasma volume ↑ 50%**, **RBC mass ↑ 20–30%** → dilution → **Hb ↓ (physiologic anemia)**. * **WBC ↑** (can reach 12–16k). * **Platelets mildly ↓** (gestational thrombocytopenia). * **Hypercoagulable state** → fibrinogen ↑, clotting factors ↑. ### 🔹 *Clinical significance* * Protects from postpartum hemorrhage. * ↑ VTE risk — especially postpartum. --- ## 🌸 **4. Renal & Urinary Adaptations** ### 🔹 *Changes* * **GFR ↑ 40–50%** (starts early). * **Serum creatinine ↓ 0.4–0.6 mg/dL**. * **Mild glycosuria** common. * **Hydronephrosis of pregnancy** (right > left) due to progesterone + uterine compression. ### 🔹 *Clinical significance* * Minor proteinuria acceptable (<300 mg/day). * Avoid misinterpreting physiologic glycosuria as diabetes. --- ## 🌸 **5. Endocrine Adaptations** ### 🔹 *Pituitary* * **Prolactin ↑** 10-fold → lactation prep. * **ACTH & MSH ↑** → pigmentation changes. ### 🔹 *Thyroid* * **Estrogen ↑ TBG**, total T3/T4 ↑; **free T4 normal**. * **hCG weak TSH activity → TSH ↓** (first trimester). ### 🔹 *Pancreas* * Early pregnancy: **insulin sensitivity ↑**. * Late pregnancy: **insulin resistance ↑** (placental hormones: hPL, cortisol) → predisposes to **GDM**. --- ## 🌸 **6. Gastrointestinal Adaptations** ### 🔹 *Changes* * **Progesterone ↓ LES tone** → heartburn. * **Gastric emptying ↓** → nausea/vomiting. * **Constipation** from prolonged transit time. * **Hemorrhoids** due to venous congestion. ### 🔹 *Clinical significance* * Morning sickness peaks at 9–10 weeks. * Hyperemesis gravidarum requires electrolyte correction. --- ## 🌸 **7. Musculoskeletal Adaptations** ### 🔹 *Changes* * **Relaxin + progesterone → ligament laxity**. * **Lumbar lordosis ↑** due to uterine weight. * **Carpal tunnel syndrome** possible. * **Leg cramps**, **low-back pain** common. ### 🔹 *Clinical significance* * Risk of falls increases. * Proper posture + exercises advised. --- ## 🌸 **8. Breast Changes** * **Size ↑**, ducts proliferate. * **Areolar pigmentation**, Montgomery tubercles prominent. * **Colostrum secretion** by late pregnancy. --- ## 🌸 **9. Dermatologic Adaptations** * **Linea nigra**, **melasma**, **striae gravidarum**. * **Spider angiomas**, palmar erythema (estrogen related). --- ## 🌸 **10. Metabolic Adaptations** * **Basal metabolic rate ↑ 15–20%**. * **Fat deposition ↑** early pregnancy. * Late pregnancy: catabolic → **fat mobilization** for maternal energy, glucose spared for fetus. --- # ⭐ **ULTRA-SHORT MEMORY HACK TABLE** | System | Key Adaptation | Why it Happens | | --------------- | ---------------------- | ---------------------------------------------------- | | CVS | CO ↑ 50%, plasma ↑ 50% | To meet fetal perfusion & buffer delivery blood loss | | Respiratory | TV ↑, PCO₂ ↓ | Better fetal CO₂ removal | | Renal | GFR ↑ 50% | Remove maternal/fetal waste | | Hematologic | Hypercoagulable | Prevent PPH | | Endocrine | Insulin resistance | Ensure fetal glucose | | GI | ↓ Motility | Progesterone effect | | Musculoskeletal | Ligament laxity | Prepare pelvis for birth | --- If you want, I can generate: ✅ **HTML-CSS-JS formatted article** (like your LWT posts) ✅ **MCQs (20/25/30 hard case-based)** ✅ **SEO title + description + keywords** ✅ **Custom medical diagram for maternal adaptations** Just tell me **which output you want next**.
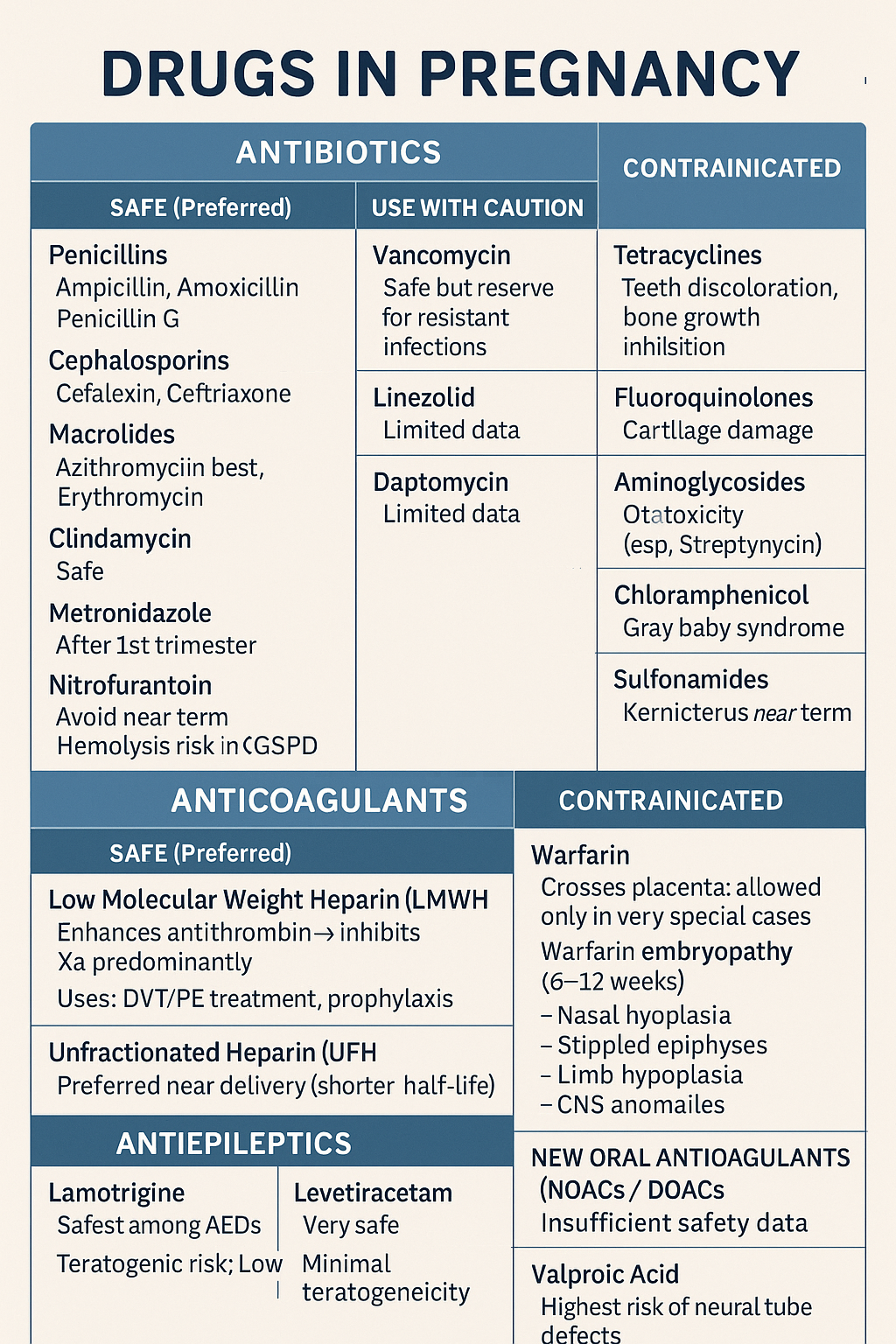
Comprehensive guide on safe and unsafe drugs in pregnancy including antibiotics, anticoagulants, and antiepileptics. Covers risks, teratogenicity, and clinical management
Below is a **concise but complete, exam-ready note** on **Drugs in Pregnancy – Antibiotics, Anticoagulants, Antiepileptics**. Structured for **quick revision + maximum coverage**. --- # ⭐ **DRUGS IN PREGNANCY – DETAILED NOTE (ANTIBIOTICS, ANTICOAGULANTS, ANTIEPILEPTICS)**    ## ✔ **SAFE (Preferred)** ### **Low Molecular Weight Heparin (LMWH)** * **Examples:** Enoxaparin, Dalteparin * **Mechanism:** Enhances antithrombin → inhibits **Xa** predominantly * **Does NOT cross placenta → safest anticoagulant** * **Uses:** DVT/PE treatment, prophylaxis, thrombophilia, APS * **Monitoring:** Anti-Xa levels in special cases (obesity, renal disease) ### **Unfractionated Heparin (UFH)** * Safe (does not cross placenta) * Preferred **near delivery** (shorter half-life, reversible with protamine) --- ## ❌ **CONTRAINDICATED** ### **Warfarin** * Crosses placenta → **warfarin embryopathy** (6–12 weeks): * Nasal hypoplasia * Stippled epiphyses * Limb hypoplasia * CNS anomalies * **Fetal hemorrhage** anytime * **Allowed only in very special cases:** mechanical heart valves when LMWH fails. --- ## ⚠ **NEW ORAL ANTICOAGULANTS (NOACs / DOACs)** Apixaban, Rivaroxaban, Dabigatran * **Avoid in pregnancy** → insufficient safety, crosses placenta --- # 3️⃣ **ANTIEPILEPTICS IN PREGNANCY**  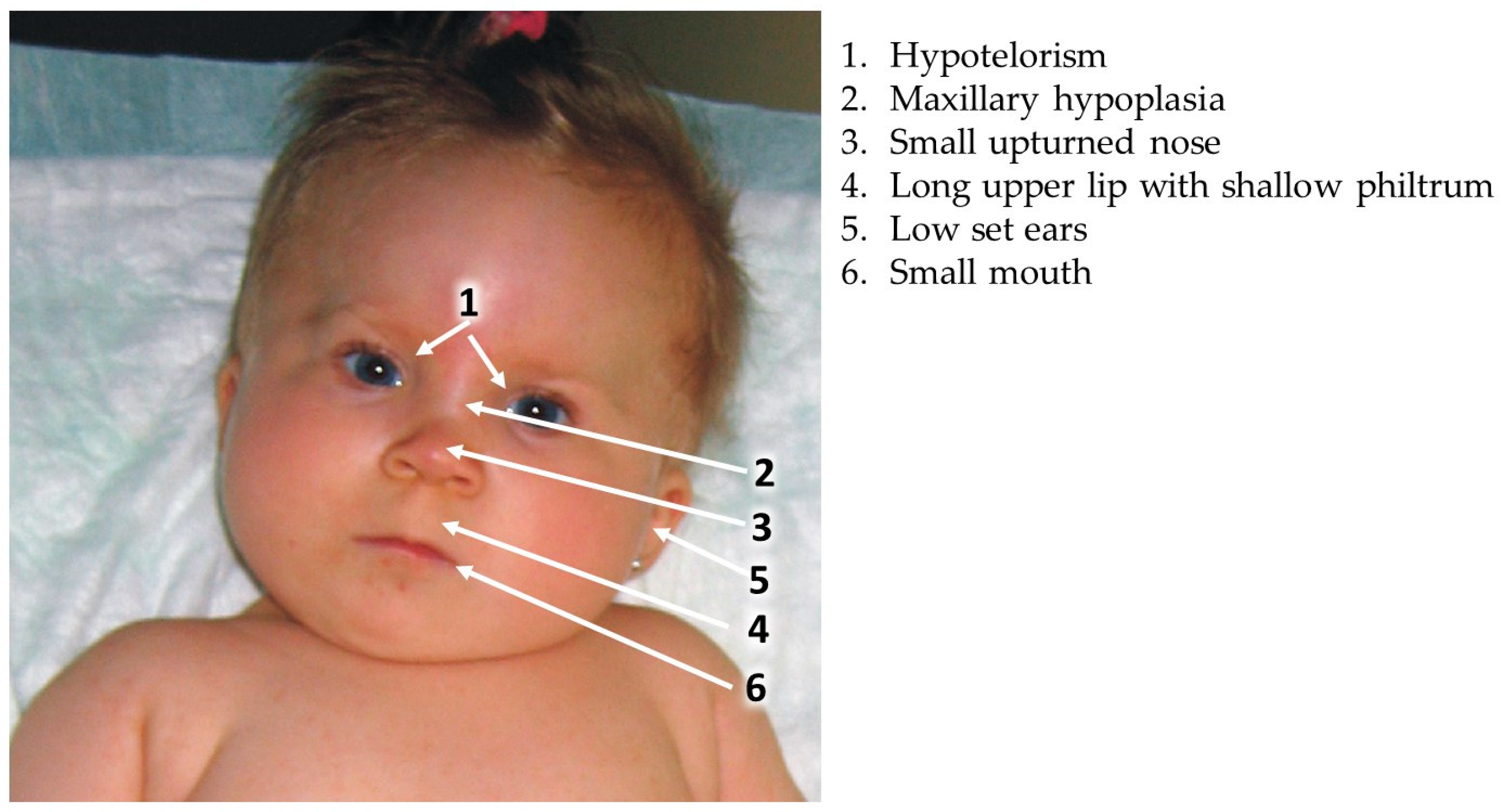   ## ⭐ **KEY PRINCIPLES** * Goal: **Seizure control** (maternal seizures are more harmful than drug risk) * Use **monotherapy** at **lowest effective dose** * Supplement **Folic acid 4–5 mg/day preconception → 1st trimester** * Check drug levels in pregnancy (pharmacokinetics change) --- ## ✔ **RELATIVELY SAFE ANTIEPILEPTICS (Preferred)** ### **1. Lamotrigine** * Safest among AEDs * **Teratogenic risk:** Low * **PK:** Increased clearance → dose adjustment needed * **Adverse:** Rash (SJS risk) ### **2. Levetiracetam** * Very safe * Minimal teratogenicity * Well-tolerated ### **3. Carbamazepine (with caution)** * Moderate teratogenic risk * Associated with **neural tube defects (NTD)** (~1%) * Give **high-dose folic acid** --- ## ⚠ **USE WITH CAUTION** | AED | Risk | | ----------------- | ---------------------------------------------------------------------- | | **Phenytoin** | Fetal hydantoin syndrome: growth delay, facial anomalies, limb defects | | **Topiramate** | Cleft lip/palate | | **Phenobarbital** | Cognitive defects, withdrawal | --- ## ❌ **AVOID / HIGHLY TERATOGENIC** ### **Valproic Acid** * **Highest risk of neural tube defects (5–10%)** * Cognitive impairment * Cardiac defects * Dose-dependent teratogenicity * **Avoid in pregnancy unless no alternative** --- # 4️⃣ **IMPORTANT COMPARISON TABLES** ## **A. Safe vs Unsafe Antibiotics** | Safe | Unsafe | | ------------------------------ | -------------------------- | | Penicillins | Tetracycline | | Cephalosporins | Fluoroquinolones | | Azithromycin | Aminoglycosides (ototoxic) | | Metronidazole (after 1st tri) | Chloramphenicol | | Nitrofurantoin (not near term) | Sulfonamides (near term) | --- ## **B. Safe vs Unsafe Anticoagulants** | Safe | Unsafe | | ---- | -------- | | LMWH | Warfarin | | UFH | NOACs | --- ## **C. Safe vs High-Risk Antiepileptics** | Safer | Moderate | High-risk | | ------------- | ------------- | ------------- | | Lamotrigine | Carbamazepine | Valproate | | Levetiracetam | Phenytoin | Phenobarbital | | — | Topiramate | — | --- # 5️⃣ **MANAGEMENT SUMMARY IN PREGNANCY** ### 🔹 **Infection** * Prefer beta-lactams * Avoid teratogenic antibiotics * Treat aggressively because **maternal sepsis harms fetus more** ### 🔹 **Thromboembolism** * **LMWH first-line** * Switch to UFH close to delivery * Avoid warfarin except mechanical valves requiring high-intensity anticoagulation ### 🔹 **Epilepsy** * Continue AEDs (never stop abruptly) * Choose **Lamotrigine or Levetiracetam** * Avoid **Valproate** * High-dose folic acid (4–5 mg/day) --- If you want, I can also generate: ✅ **25 MCQs (HTML/CSS/JS exam mode)** ✅ **Case scenarios with management** ✅ **SEO title + description + keywords** ✅ **Infographics / images for notes** Just tell me!
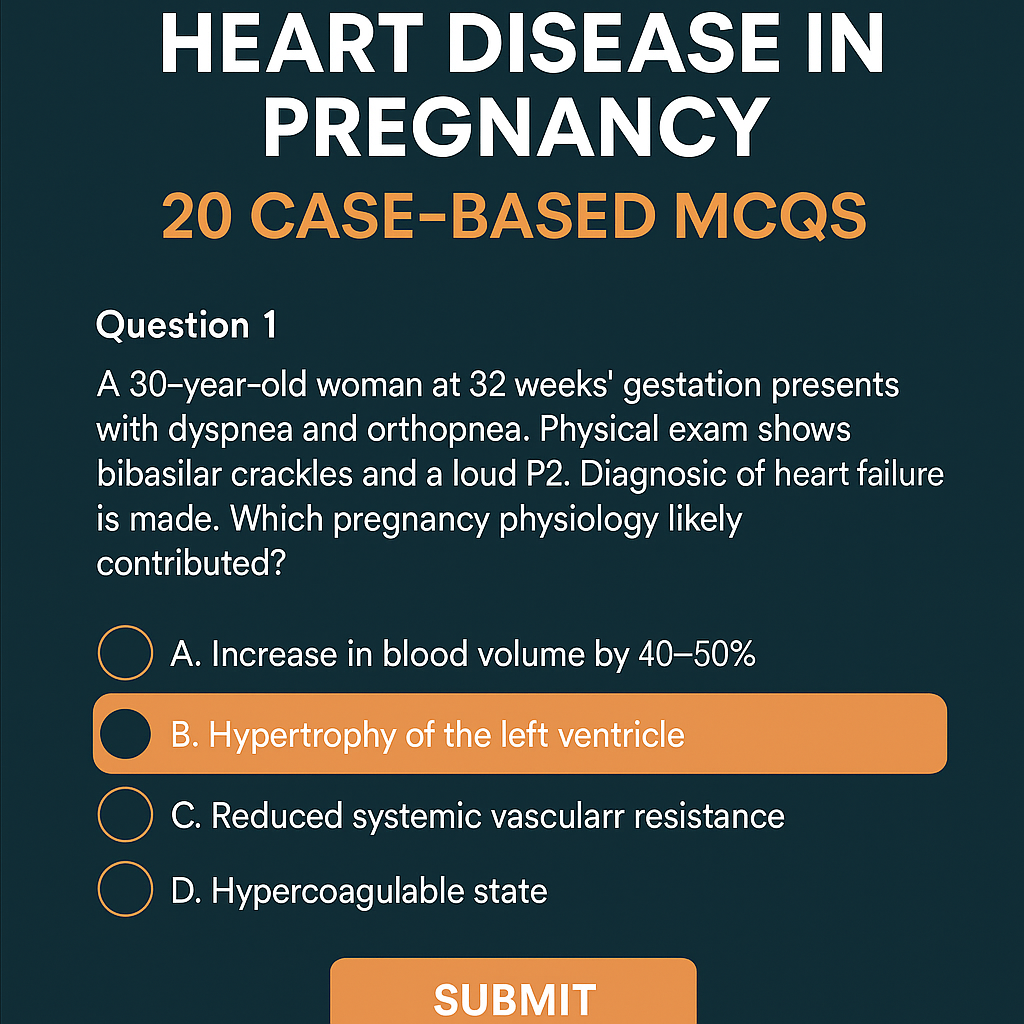
Heart Disease in Pregnancy: Causes, Risks, Management & 20 Case-Based MCQs (With Answers & Explanations)
Below is a **complete, exam-ready, concise-but-exhaustive reference** for **Heart Disease in Pregnancy** — covering definition, physiology, classification, clinical features, investigations, management (stepwise), drug details, labor/delivery planning, postpartum care, and contraindications. --- # **Heart Disease in Pregnancy – Complete Overview** ! --- ## **1. Definition** Heart disease in pregnancy refers to **pre-existing cardiac disorders** (congenital or acquired) or **pregnancy-induced cardiac dysfunction** (e.g., peripartum cardiomyopathy) that complicate pregnancy, labor, or postpartum period. --- ## **2. Why Pregnancy Worsens Heart Disease (Physiological Changes)** Pregnancy causes major hemodynamic changes that peak at **28–32 weeks**: * **↑ Blood volume by 40–50%** * **↑ Cardiac output by 30–50%** * **↑ Heart rate by 10–20 bpm** * **↓ Systemic vascular resistance** * **Hypercoagulable state** * **During labor:** CO ↑ 20–30% more * **Immediately postpartum:** Autotransfusion ↑ CO up to 80% These changes may **unmask latent heart disease** or **worsen existing cardiac failure**. --- ## **3. Types of Heart Diseases Seen in Pregnancy** ### **A. Congenital Heart Disease (CHD)** * Atrial septal defect (ASD) * Ventricular septal defect (VSD) * Patent ductus arteriosus (PDA) * Tetralogy of Fallot (repaired/unrepaired) * Eisenmenger syndrome (very high-risk) ### **B. Acquired Heart Disease** * Rheumatic heart disease * Mitral stenosis (most common serious lesion in pregnancy) * Mitral regurgitation * Aortic stenosis * Cardiomyopathies * **Peripartum cardiomyopathy** * Ischemic heart disease * Arrhythmias * Hypertensive heart disease --- ## **4. WHO Classification of Maternal Cardiovascular Risk** ### **WHO Class I – Low Risk** * Small ASD/VSD * PDA * Mitral valve prolapse * Successfully repaired simple CHD ### **WHO Class II – Moderate Risk** * Unrepaired ASD/VSD * Repaired TOF * Mild LV dysfunction ### **WHO Class III – High Risk** * Mechanical valves * Cyanotic congenital heart disease * Moderate LV dysfunction * Previous peripartum cardiomyopathy with normal EF now ### **WHO Class IV – Extremely High Risk (Pregnancy Contraindicated)** * **Pulmonary hypertension / Eisenmenger syndrome** * **Severe LV dysfunction (EF < 30%)** * **Severe mitral stenosis or aortic stenosis** * **Marfan syndrome with aorta > 45 mm** * **Previous peripartum cardiomyopathy with persistent dysfunction** --- ## **5. Clinical Features** ### **Symptoms** * Dyspnea (especially NYHA III–IV) * Orthopnea / PND * Fatigue * Palpitations * Chest pain * Syncope ### **Warning Features of Cardiac Decompensation** * Dyspnea at rest * Hemoptysis * Cyanosis * Loud P2 / RV heave * Basal crepitations * New arrhythmias --- ## **6. Investigations** ### **Basic** * CBC * ECG * **Echocardiography – Most important** * BNP (optional) ### **Advanced** * Cardiac MRI (safe without gadolinium) * Holter monitoring * Exercise testing (pre-pregnancy only) ### **Avoid** * CT angiography unless life-saving * ACE inhibitors / ARBs history to be checked --- ## **7. Complications** * **Maternal:** Heart failure, arrhythmias, thromboembolism, endocarditis, cardiac arrest * **Fetal:** IUGR, preterm birth, fetal hypoxia, congenital heart disease (3–5% risk) --- # **8. Management of Heart Disease in Pregnancy (Stepwise)**   --- ## **A. Preconception Counselling** * Risk assessment + WHO classification * Optimize cardiac status (e.g., balloon valvotomy for MS) * Stop teratogenic drugs (ACE inhibitors, ARBs, statins, warfarin if possible) --- ## **B. Antenatal Management** ### **1. Lifestyle** * Adequate rest * Left lateral position * Avoid anemia (treat aggressively) * Avoid excessive weight gain * Salt restriction if HF symptoms ### **2. Drugs Used** Below are the major drug classes **with indications, mechanism, dosing, adverse effects, contraindications, interactions, and counselling.** --- ## **i. Diuretics (Furosemide)** **Indication:** Heart failure, pulmonary edema **MOA:** Loop diuretic → inhibits Na-K-2Cl in loop of Henle **Dose:** 20–40 mg PO/IV, repeat as required **PK:** Rapid onset, renal excretion **AEs:** Hypokalemia, dehydration **Contra:** Severe electrolyte imbalance **Interactions:** Digoxin ↑ toxicity if hypokalemia **Counselling:** Monitor weight, urine output, electrolytes --- ## **ii. Beta-blockers (Metoprolol preferred)** **Indication:** Rate control, arrhythmias, ischemic heart disease **MOA:** Blocks β1 receptors → ↓ HR & contractility **Dose:** 25–100 mg/day **AEs:** IUGR (minimal), bradycardia **Contra:** Severe asthma **Interactions:** Calcium channel blockers → heart block risk **Counselling:** Do not stop suddenly --- ## **iii. Anticoagulants** ### **a. LMWH (Enoxaparin) – Preferred** **Indication:** Mechanical valves, AF, thromboembolism **MOA:** Enhances antithrombin III → inhibits Xa **Dose:** 1 mg/kg twice daily **Monitoring:** Anti-Xa levels **AEs:** Bleeding **Contra:** Active bleeding ### **b. Warfarin – Teratogenic (avoid 6–12 weeks)** Used only when valve thrombosis risk is very high. --- ## **iv. Vasodilators (Hydralazine, Nitrates)** **Indication:** HF with hypertension **AEs:** Headache, hypotension --- ## **v. Digoxin** **Indication:** HF with atrial fibrillation **MOA:** Na-K ATPase inhibition → ↑ Ca → ↑ contractility **Dose:** 0.125–0.25 mg daily **AEs:** Toxicity (nausea, vision changes) **Monitor:** Serum levels --- ## **Drugs Contraindicated in Pregnancy** * **ACE inhibitors / ARBs** → renal failure, skull defects * **Amiodarone** → fetal thyroid dysfunction * **Warfarin (first trimester)** unless essential * **Statins** --- ## **C. Follow-up Schedule** * Monthly (WHO I–II) * Fortnightly (WHO III) * Weekly (WHO IV — pregnancy discouraged) --- # **9. Labor and Delivery Management**   ### **Preferred Mode:** **Vaginal delivery with epidural anesthesia** ### **Indications for Caesarean Section** * Severe aortic stenosis * Marfan with aortic root dilation * Eisenmenger * Severe HF * Anticoagulation not stopped ### **Intrapartum Measures** * Continuous ECG + pulse oximetry * Avoid fluid overload * Slow, assisted second stage (forceps/vacuum) ### **Anesthesia** * Epidural preferred * Avoid general anesthesia (↑ cardiac stress) --- # **10. Postpartum Care** * Highest risk of heart failure in **first 24–72 hours** * Gradual mobilization * Restart anticoagulation after 6 hours (if needed) * Contraception counselling * **Avoid estrogen pills** * Prefer: IUCD, progestin-only methods --- # **11. High-Risk Specific Conditions** ## **A. Mitral Stenosis** * Most dangerous RHD lesion in pregnancy * Tachycardia → ↑ LA pressure → pulmonary edema * Management: β-blockers + diuretics * Balloon valvotomy if severe --- ## **B. Eisenmenger Syndrome** * **Pregnancy contraindicated (WHO IV)** * Maternal mortality 30–50% * No effective treatment → counselling for termination --- ## **C. Peripartum Cardiomyopathy** * Heart failure in last month of pregnancy or 5 months postpartum * EF < 45% * Treatment: * Diuretics * Beta-blockers * Bromocriptine (stops prolactin → improves function) * Avoid future pregnancy if EF not normalized --- # **12. Fetal Risks** * Prematurity * Growth restriction * Neonatal asphyxia * Congenital heart disease (if mother has CHD) --- # **13. Key Prevention Strategies** * Early diagnosis * Control anemia * Avoid excessive fluids * Use cardiac medications judiciously * Multidisciplinary care (obstetrician + cardiologist) --- # **Would you like a SEO-optimized title & description for this topic, or a high-ranking blog article version?**
Comments & Discussion
Use this thread like a mini viva: add differentials, staging systems, drug regimens and exam tricks.
Login or register to comment.
No comments yet – start by adding exam-style discussion points.