Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
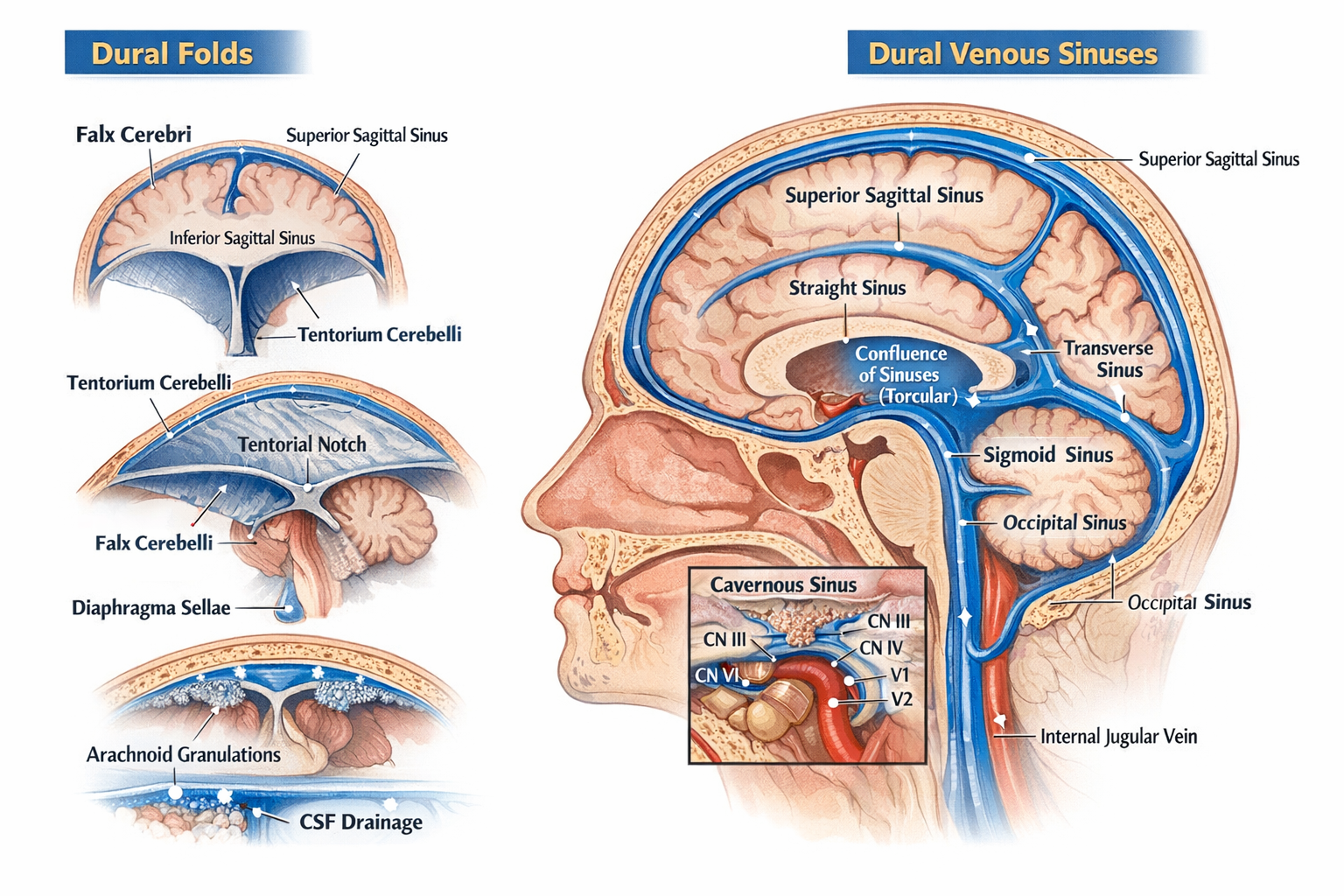
Dural Folds and Dural Venous Sinuses Anatomy, Features and Clinical Significance
## Dural Folds and Dural Venous Sinuses — Complete, Exam-Oriented Anatomy Guide (No Images) --- ## 1. Dura Mater: Brief Context The **dura mater** is the outermost meningeal layer of the brain. It has **two layers**: * **Periosteal (endosteal) layer** – lines the inner surface of the skull * **Meningeal layer** – forms inward folds (**dural folds**) Where these two layers separate, **dural venous sinuses** are formed. 🔗 *Related topic:* [Meninges of Brain](#) --- ## 2. Dural Folds (Dural Septa) Dural folds are **double-layered reflections of meningeal dura mater** that: * Stabilize the brain * Limit excessive movement * Contain venous sinuses at their attachments ### 2.1 Falx Cerebri A **sickle-shaped vertical fold** in the midline. **Attachments** * Anterior: Crista galli of ethmoid * Posterior: Internal occipital protuberance (joins tentorium cerebelli) **Separates** * Right and left cerebral hemispheres **Venous Sinuses Contained** * Superior sagittal sinus (upper border) * Inferior sagittal sinus (free lower border) * Straight sinus (posterior attachment) **Clinical relevance** * Falx meningioma * Subfalcine herniation 🔗 *See also:* [Cerebral Herniation Syndromes](#) --- ### 2.2 Tentorium Cerebelli A **horizontal tent-like fold**. **Attachments** * Anterior: Clinoid processes * Lateral: Superior border of petrous temporal bone * Posterior: Occipital bone **Separates** * Cerebrum (above) from cerebellum (below) **Opening** * Tentorial notch → passage for midbrain **Venous Sinuses Contained** * Transverse sinus * Superior petrosal sinus * Straight sinus (junction with falx cerebri) **Clinical relevance** * Transtentorial (uncal) herniation * Compression of oculomotor nerve 🔗 *Related topic:* [Midbrain Anatomy](#) --- ### 2.3 Falx Cerebelli A **small vertical fold** below the tentorium. **Attachments** * Internal occipital crest **Separates** * Two cerebellar hemispheres (partially) **Venous Sinus** * Occipital sinus --- ### 2.4 Diaphragma Sellae A **small circular dural fold** forming the roof of sella turcica. **Central opening** * Allows passage of pituitary stalk (infundibulum) **Clinical relevance** * Pituitary adenoma expansion * CSF leak after trans-sphenoidal surgery 🔗 *See also:* [Pituitary Gland Anatomy](#) --- ## 3. Dural Venous Sinuses ### Definition **Endothelial-lined venous channels** between layers of dura mater that drain venous blood from brain, meninges, and skull. **Key characteristics** * No valves * No muscular layer * Rigid walls (do not collapse) --- ## 4. Classification of Dural Venous Sinuses ### 4.1 Unpaired Sinuses #### Superior Sagittal Sinus * Location: Upper margin of falx cerebri * Drains: Cerebral veins, CSF via arachnoid granulations * Ends in: Confluence of sinuses **Clinical** * Site of CSF absorption * Thrombosis → raised intracranial pressure --- #### Inferior Sagittal Sinus * Location: Free lower margin of falx cerebri * Drains into: Straight sinus --- #### Straight Sinus * Formed by union of inferior sagittal sinus + great cerebral vein (of Galen) * Ends in: Confluence of sinuses --- #### Occipital Sinus * Smallest sinus * Located in falx cerebelli --- ### 4.2 Paired Sinuses #### Transverse Sinuses * Located along posterolateral margin of tentorium * Drain into: Sigmoid sinuses --- #### Sigmoid Sinuses * S-shaped * Continue as: Internal jugular veins 🔗 *Related topic:* [Internal Jugular Vein](#) --- #### Cavernous Sinus (Highly Important) Located on either side of body of sphenoid. **Contents** * Internal carotid artery * CN VI (abducent nerve) **Lateral wall (superior to inferior)** * CN III * CN IV * V1 * V2 **Drains** * Superior & inferior ophthalmic veins **Clinical** * Cavernous sinus thrombosis * Carotid–cavernous fistula 🔗 *See also:* [Cranial Nerves in Cavernous Sinus](#) --- #### Petrosal Sinuses * **Superior petrosal sinus**: cavernous → transverse * **Inferior petrosal sinus**: cavernous → internal jugular vein --- ## 5. Confluence of Sinuses (Torcular Herophili) * Located at internal occipital protuberance * Receives: * Superior sagittal sinus * Straight sinus * Occipital sinus * Drains into: Transverse sinuses --- ## 6. CSF Drainage and Arachnoid Granulations * CSF absorbed into **superior sagittal sinus** * Via arachnoid villi and granulations 🔗 *Related topic:* [CSF Circulation and Absorption](#) --- ## 7. Clinical Correlation Summary | Condition | Related Structure | | ----------------- | -------------------------- | | Raised ICP | Superior sagittal sinus | | Uncal herniation | Tentorium cerebelli | | Diplopia | Cavernous sinus (CN VI) | | CSF leak | Diaphragma sellae | | Venous thrombosis | Sagittal / cavernous sinus | --- ## 8. One-Line Exam Pearls * Dural folds are formed by **meningeal dura only** * Venous sinuses lack valves and smooth muscle * Cavernous sinus is the **only sinus containing cranial nerves** * Falx cerebri contains **two sagittal sinuses** --- If you want, I can next provide: * **SEO title, meta description, and long-tail keywords** * **20 hard MCQs (including case-based)** * **FAQ schema JSON** * **Internal link structure optimized for a medical website**
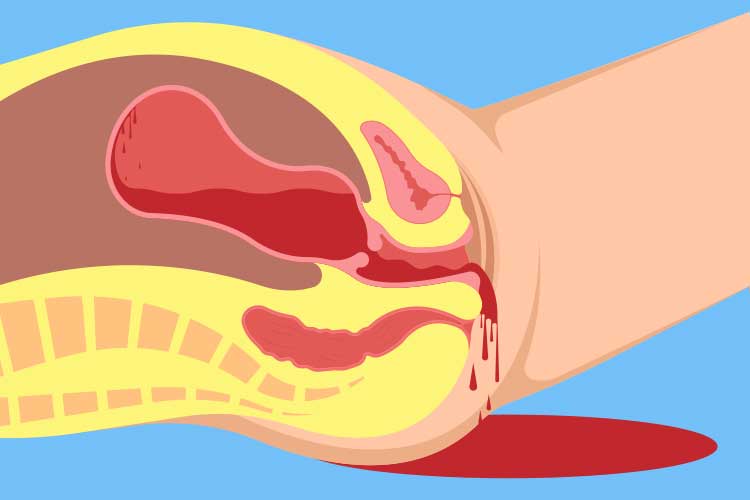
Postpartum Hemorrhage Causes Diagnosis and Management
## **Postpartum Hemorrhage Clinical Guide Causes Diagnosis and Management** ### **Definition** **Postpartum hemorrhage (PPH)** is excessive bleeding after childbirth. * **Primary (early) PPH:** ≥500 mL after vaginal delivery or ≥1000 mL after cesarean section within **24 hours** * **Secondary (late) PPH:** Excessive bleeding from **24 hours to 6 weeks** postpartum --- ## **Epidemiology and Importance** * Leading cause of **maternal mortality worldwide** * Rapid onset and progression require **early recognition and protocol-based management** --- ## **Pathophysiology** Normal hemostasis after delivery depends on **uterine contraction** compressing spiral arteries. Failure of contraction or disruption of clotting leads to uncontrolled bleeding. --- ## **Causes – “4 Ts” Framework** 1. **Tone (most common – uterine atony)** * Overdistended uterus (multiple pregnancy, polyhydramnios, macrosomia) * Prolonged or precipitous labor * Chorioamnionitis 2. **Trauma** * Cervical, vaginal, perineal tears * Uterine rupture * Hematomas 3. **Tissue** * Retained placental tissue * Placenta accreta spectrum 4. **Thrombin** * Coagulopathies (DIC, severe preeclampsia, HELLP, anticoagulant use) --- ## **Risk Factors** * Previous PPH * Operative delivery * Induction or augmentation of labor * Anemia * Placenta previa or accreta --- ## **Clinical Features** * Excessive vaginal bleeding * Boggy or enlarged uterus * Signs of hypovolemia: tachycardia, hypotension, pallor, altered sensorium * Reduced urine output --- ## **Initial Assessment and Diagnosis** **Diagnosis is clinical and urgent** * Quantify blood loss (visual + weighing) * Assess uterine tone * Inspect birth canal * Evaluate placenta completeness ### **Investigations (do not delay treatment)** * CBC (Hb, platelets) * Blood group and cross-match * Coagulation profile (PT, aPTT, fibrinogen) * ABG if severe shock --- ## **Management – Stepwise Approach** ### **Immediate Resuscitation** * Call for help * Airway and oxygen * Two wide-bore IV lines * Crystalloids followed by blood products (1:1:1 PRBC:plasma:platelets if massive) --- ## **Uterotonic Drugs (Cornerstone of Treatment)** ### **1. Oxytocin** * **Indication:** First-line for uterine atony * **Mechanism:** Stimulates uterine smooth muscle contraction * **Dose:** * IV infusion: 10–40 IU in 1 L NS/RL * IM: 10 IU * **Adverse effects:** Hypotension (rapid IV), water intoxication * **Contraindications:** None significant in PPH * **Monitoring:** Uterine tone, vitals * **Counselling:** First-line and safe --- ### **2. Methylergometrine** * **Mechanism:** Sustained uterine contraction via alpha-adrenergic stimulation * **Dose:** 0.2 mg IM (may repeat) * **Adverse effects:** Hypertension, nausea * **Contraindications:** Hypertension, preeclampsia, cardiac disease * **Monitoring:** Blood pressure --- ### **3. Carboprost (15-methyl PGF2α)** * **Mechanism:** Prostaglandin-induced myometrial contraction * **Dose:** 250 µg IM every 15–90 min (max 8 doses) * **Adverse effects:** Bronchospasm, diarrhea, fever * **Contraindications:** Asthma * **Monitoring:** Respiratory status --- ### **4. Misoprostol** * **Mechanism:** Prostaglandin E1 analog * **Dose:** 800–1000 µg rectal or sublingual * **Adverse effects:** Fever, shivering * **Use:** Low-resource settings --- ### **5. Tranexamic Acid** * **Indication:** All PPH within 3 hours of onset * **Mechanism:** Inhibits fibrinolysis * **Dose:** 1 g IV over 10 min (repeat once if bleeding continues) * **Adverse effects:** Rare thrombosis * **Contraindications:** Active thromboembolic disease * **Monitoring:** Renal function if repeated * **Counselling:** Reduces mortality when given early --- ## **Mechanical and Surgical Measures** ### **Mechanical** * Bimanual uterine massage * Uterine balloon tamponade (Bakri balloon) * Uterine packing ### **Surgical** * Uterine compression sutures (B-Lynch) * Uterine artery ligation * Internal iliac artery ligation * **Hysterectomy** (life-saving last resort) --- ## **Management by Cause** * **Atony:** Uterotonics → balloon → surgery * **Trauma:** Immediate repair of tears * **Tissue:** Manual removal, curettage * **Thrombin:** Correct coagulopathy with blood products --- ## **Secondary Postpartum Hemorrhage** **Causes** * Retained products * Subinvolution of uterus * Endometritis **Management** * Antibiotics * Uterotonics * Ultrasound-guided evacuation if indicated --- ## **Complications** * Hypovolemic shock * Acute kidney injury * DIC * Sheehan syndrome * Maternal death --- ## **Prevention** * Active management of third stage of labor * Antenatal anemia correction * Risk stratification and preparedness --- ## **Prognosis** Excellent with early recognition and protocol-driven care; delays increase morbidity and mortality. --- ## **SEO Meta Data** **SEO Title:** Postpartum Hemorrhage Causes Diagnosis and Management **Meta Description:** Comprehensive clinical guide on postpartum hemorrhage covering causes, diagnosis, stepwise management, uterotonic drugs, surgical options, prevention, and complications. **SEO Keywords (comma separated):** postpartum hemorrhage, PPH management, uterine atony, causes of PPH, tranexamic acid PPH, obstetric emergency, maternal hemorrhage, third stage labor complications --- ## **Frequently Asked Questions** **What is the most common cause of postpartum hemorrhage?** Uterine atony. **When should tranexamic acid be given in PPH?** Within 3 hours of onset of bleeding. **What is the first-line drug for PPH?** Oxytocin. **When is hysterectomy indicated in PPH?** When bleeding is uncontrollable and life-threatening despite conservative measures. **Can PPH occur after 24 hours?** Yes, it is termed secondary postpartum hemorrhage. --- If you want, I can **convert this into a CMS-ready HTML or PHP page**, **add FAQ schema and Article schema**, or **create MCQs and case-based questions** for your medical knowledge platform.
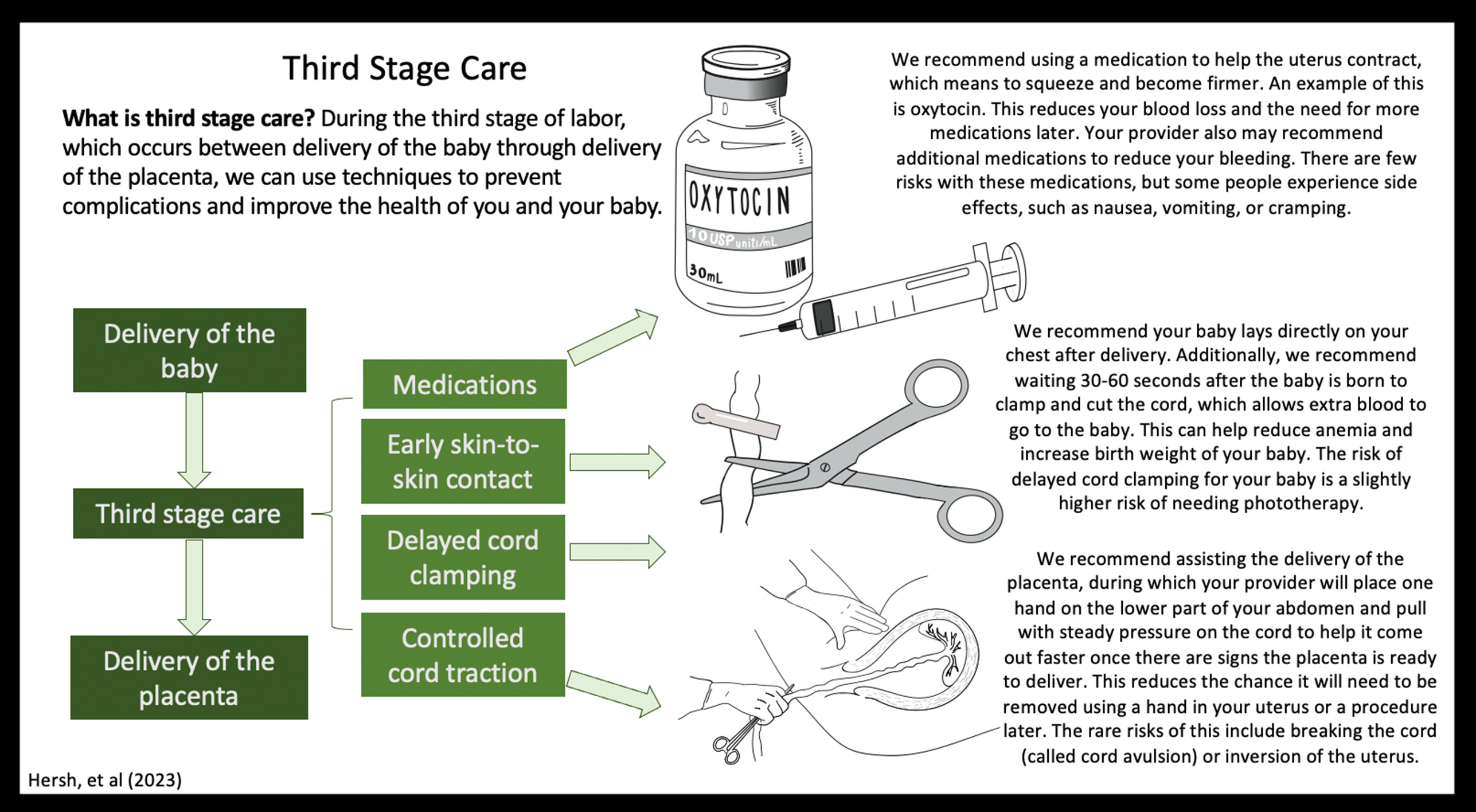
Active Management of Third Stage of Labor Complete Guide for PPH Prevention
Below is a **concise yet complete, exam-oriented, SEO-friendly reference** on **Active Management of Third Stage of Labor (AMTSL)**, structured for **medical students, clinicians, and obstetric exams**. --- # **Active Management of Third Stage of Labor (AMTSL)** ## **Definition** **Active Management of the Third Stage of Labor (AMTSL)** is a **planned set of interventions** performed **immediately after the birth of the baby** to **facilitate placental delivery and prevent postpartum hemorrhage (PPH)**, the leading cause of maternal mortality worldwide. --- ## **Importance and Rationale** * **Postpartum hemorrhage** accounts for a significant proportion of **maternal deaths** * AMTSL **reduces blood loss**, **shortens third stage**, and **lowers risk of uterine atony** * Recommended by **WHO, FIGO, ICM, and ACOG** --- ## **Components of AMTSL (Core Steps)** ### **1. Administration of a Uterotonic Drug (Most Important Step)** * Given **within 1 minute after delivery of the baby** * **After delivery of anterior shoulder or complete birth** * **Before or after placental delivery** (as per guideline) ### **2. Controlled Cord Traction (CCT)** * Gentle traction on umbilical cord * Combined with **counter-traction on uterus** * Performed **only after signs of placental separation** ### **3. Uterine Massage After Placental Delivery** * Ensures **uterine contraction** * Reduces risk of uterine atony * Routine sustained massage **not recommended**, but **assessment of tone is essential** --- ## **Uterotonic Drugs Used in AMTSL** ### **Oxytocin (Drug of Choice)** * **Dose:** 10 IU IM or slow IV * **Onset:** 2–3 minutes * **Advantages:** Highly effective, minimal side effects * **Preferred by WHO** ### **Ergometrine / Methylergometrine** * **Dose:** 0.2 mg IM/IV * **Contraindications:** Hypertension, pre-eclampsia, heart disease * Causes sustained uterine contraction ### **Oxytocin + Ergometrine (Syntometrine)** * More effective but **higher side effects** * Nausea, vomiting, hypertension ### **Misoprostol** * **Dose:** 600 μg orally * Used where injectables unavailable * Side effects: Fever, shivering --- ## **Controlled Cord Traction (CCT): Key Points** * Perform only when uterus is **well contracted** * Look for **signs of placental separation**: * Lengthening of cord * Gush of blood * Uterus becomes globular and rises * Prevents **retained placenta** * Reduces duration of third stage --- ## **Uterine Massage** * After placenta delivery * Assess uterine tone **every 15 minutes for first 2 hours** * Continuous massage is **not routinely advised** --- ## **Timing of Cord Clamping** * **Delayed cord clamping (1–3 minutes)** recommended * Does **not interfere with AMTSL** * Improves neonatal iron stores --- ## **Benefits of AMTSL** * ↓ Postpartum hemorrhage by **50–70%** * ↓ Severe blood loss (>1000 mL) * ↓ Need for blood transfusion * ↓ Duration of third stage * ↓ Maternal morbidity and mortality --- ## **AMTSL vs Expectant Management** | Feature | AMTSL | Expectant Management | | ------------- | ------------------ | -------------------- | | Uterotonic | Given routinely | Not given | | Cord traction | Yes | No | | Blood loss | Significantly less | More | | Duration | Shorter | Longer | | PPH risk | Low | High | --- ## **Indications** * **All vaginal deliveries** * Especially important in: * Anemia * Multiple pregnancy * Prolonged labor * Polyhydramnios * Grand multiparity --- ## **Contraindications** * No absolute contraindication * Avoid **ergometrine** in: * Hypertension * Preeclampsia * Cardiac disease --- ## **Complications (Rare)** * Retained placenta (if CCT done improperly) * Uterine inversion (improper traction) * Drug side effects (ergometrine, misoprostol) --- ## **WHO Recommended AMTSL Protocol (Summary)** 1. **Oxytocin 10 IU IM/IV** 2. **Delayed cord clamping** 3. **Controlled cord traction** 4. **Assess uterine tone** --- ## **Key Exam Pearls** * **Most important component:** Uterotonic administration * **Drug of choice:** Oxytocin * **Primary aim:** Prevention of postpartum hemorrhage * **Third stage normal duration:** ≤ 30 minutes --- ## **Conclusion** **Active Management of Third Stage of Labor** is a **simple, cost-effective, life-saving obstetric intervention**. Universal implementation of AMTSL significantly reduces **postpartum hemorrhage and maternal mortality**, making it a **standard of care in modern obstetrics**. --- ### If you want next: * **SEO title and meta keywords** * **High-yield MCQs (exam mode) in single HTML-CSS-JS file** * **Clinical flowchart image** * **Comparison table for exams** Just tell me 👍
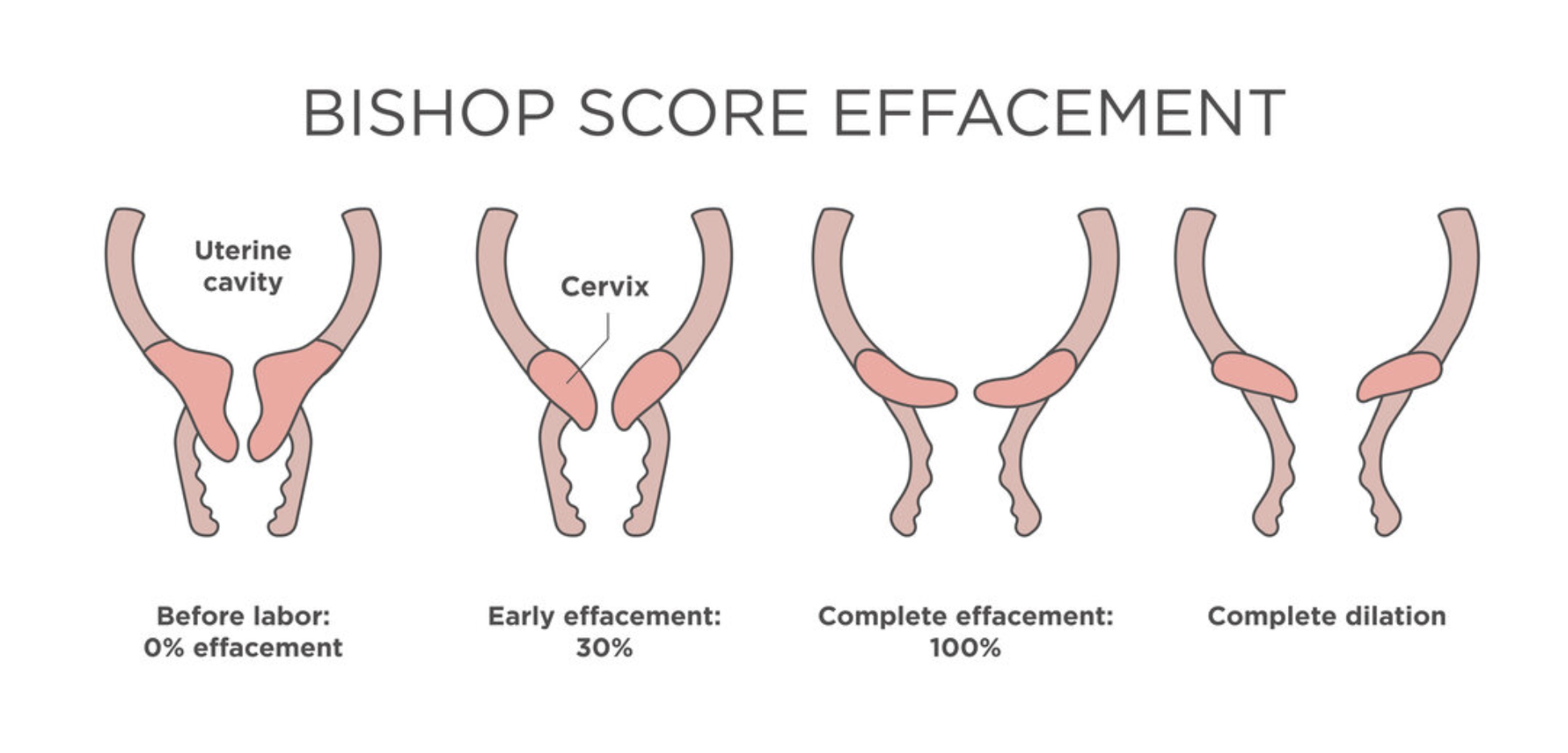
Induction of Labor Indications Methods Contraindications Complications
Below is a **concise yet complete, SEO-friendly, exam-ready reference** on **Induction of Labor**, structured with clear headings (H1–H3 style) and high-yield clinical content. --- # **Induction of Labor** ## **Definition** **Induction of labor (IOL)** is the **artificial initiation of uterine contractions** before the spontaneous onset of labor, with the aim of achieving **vaginal delivery**, when continuation of pregnancy poses **greater maternal or fetal risk** than delivery. --- ## **Indications for Induction of Labor** ### **Maternal Indications** * Post-term pregnancy (≥41 weeks) * Pre-eclampsia and eclampsia * Gestational hypertension * Diabetes mellitus (gestational or pre-existing) * Premature rupture of membranes (PROM) at term * Chorioamnionitis * Rh isoimmunization * Maternal medical disorders (renal, cardiac disease) * Intrauterine fetal demise (IUFD) ### **Fetal Indications** * Intrauterine growth restriction (IUGR) * Oligohydramnios * Non-reassuring fetal status (controlled setting) * Fetal anomalies requiring early delivery ### **Elective Induction** * At ≥39 weeks with confirmed gestational age and favorable cervix --- ## **Contraindications to Induction of Labor** ### **Absolute Contraindications** * Placenta previa * Vasa previa * Transverse lie * Cord prolapse * Previous classical cesarean section * Previous uterine rupture * Invasive cervical cancer * Cephalopelvic disproportion (CPD) ### **Relative Contraindications** * Multiple previous cesarean sections * Grand multiparity * Unstable lie * Active genital herpes --- ## **Pre-Induction Assessment** Show readiness of cervix and maternal-fetal safety. ### **Bishop Score** Assesses **cervical favorability** using: * Cervical dilatation * Effacement * Consistency * Position * Fetal station **Score interpretation:** * **≥6–8** → Favorable cervix (high success) * **<6** → Unfavorable cervix (requires cervical ripening) --- ## **Methods of Induction of Labor** ### **1. Mechanical Methods** * **Membrane sweeping** * **Foley catheter (balloon catheter)** * Double balloon catheter **Advantages:** Low cost, minimal uterine hyperstimulation **Disadvantages:** Discomfort, infection risk --- ### **2. Pharmacological Methods** #### **Prostaglandins** * **Dinoprostone (PGE₂)** – Gel, tablet, vaginal insert * **Misoprostol (PGE₁)** – Oral or vaginal **Actions:** * Cervical ripening * Uterine contractions **Contraindications:** * Previous uterine scar (relative for misoprostol) * Fetal distress * Hypersensitivity --- #### **Oxytocin** * Used after cervical ripening * IV infusion with titration **Mechanism:** Stimulates uterine smooth muscle contraction **Monitoring:** Continuous CTG required --- ### **3. Surgical Methods** * **Amniotomy (Artificial rupture of membranes)** **Prerequisites:** * Engaged head * Favorable cervix * No placenta previa --- ## **Monitoring During Induction** * Continuous fetal heart rate monitoring * Maternal vitals * Uterine contraction pattern * Progress of labor (partograph) --- ## **Complications of Induction of Labor** ### **Maternal Complications** * Uterine hyperstimulation * Uterine rupture * Postpartum hemorrhage * Infection * Failed induction leading to cesarean section ### **Fetal Complications** * Fetal distress * Meconium aspiration * Birth asphyxia * Cord prolapse (after amniotomy) --- ## **Failed Induction** **Definition:** Failure to establish active labor after adequate attempts with appropriate methods. **Management:** * Re-assess indication * Repeat cervical ripening * Cesarean delivery if indicated --- ## **Key Clinical Pearls** * Always confirm **gestational age** before induction * Bishop score guides method selection * Avoid prostaglandins in scarred uterus (especially misoprostol) * Continuous monitoring is mandatory * Individualize induction based on maternal and fetal condition --- ## **Conclusion** Induction of labor is a **critical obstetric intervention** that improves maternal and fetal outcomes when appropriately indicated. Proper **case selection, cervical assessment, method choice, and vigilant monitoring** are essential to maximize success and minimize complications. --- If you want, I can next provide: * **SEO title, meta description, and keywords** * **Exam-oriented tables** * **Case-based MCQs (HTML + CSS + JS, single file, modern UI)** * **Flowcharts for induction decision-making**
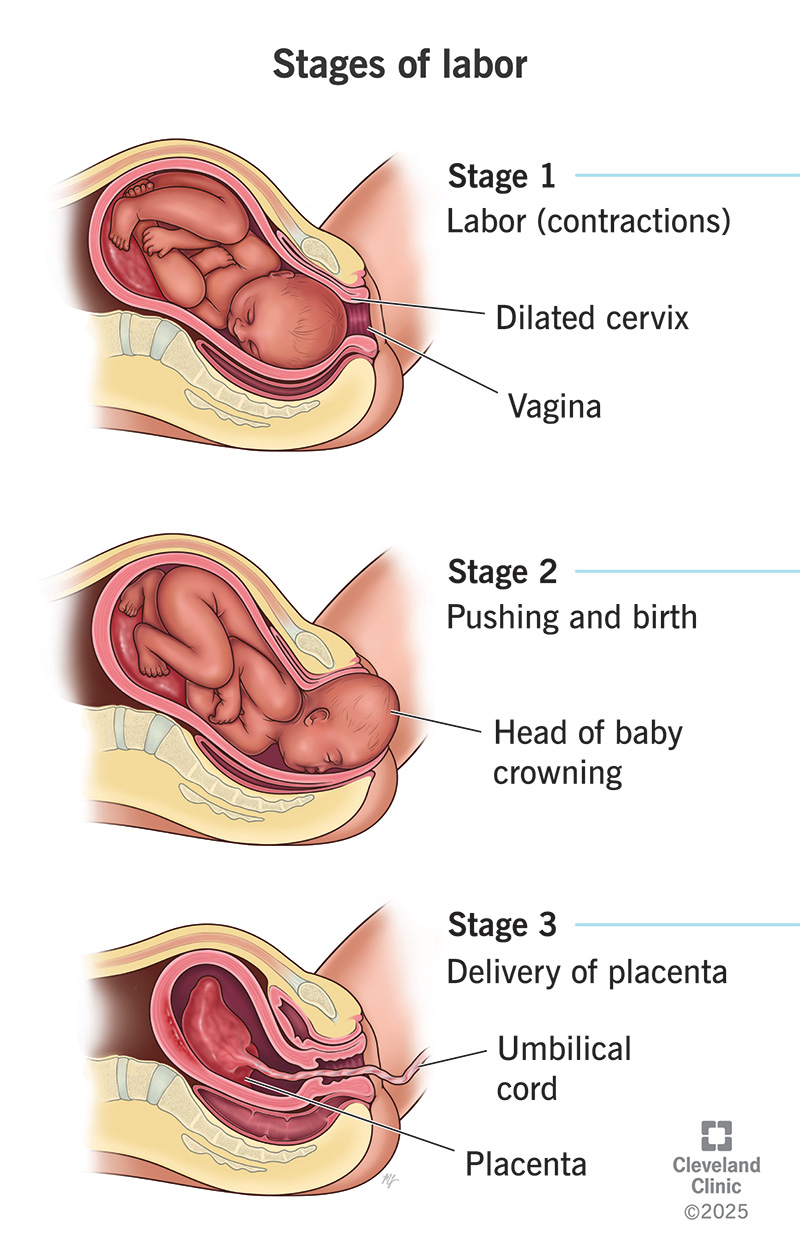
Normal Labour Definition Stages Physiology Management and Clinical Features
Below is a **concise yet complete, SEO-friendly medical reference** on **Normal Labour**, structured with clear **H1–H3 headings** and exam-oriented clarity. --- # **Normal Labour** ## **Definition of Normal Labour** Normal labour is a **physiological process** in which a **term pregnancy (37–42 weeks)** culminates in the **spontaneous onset of labour**, resulting in **vaginal delivery of a single, live fetus in vertex presentation**, followed by expulsion of the placenta, **without maternal or fetal complications**. --- ## **Criteria of Normal Labour** Normal labour fulfills all of the following: * **Gestational age:** 37–42 weeks * **Onset:** Spontaneous * **Presentation:** Vertex (cephalic) * **Number of fetus:** Singleton * **Progress:** Regular uterine contractions with progressive cervical dilatation * **Mode of delivery:** Vaginal, without operative intervention * **Outcome:** Healthy mother and baby --- ## **Physiology of Normal Labour** Labour is initiated by a complex interaction of: * **Hormonal factors:** ↑ Estrogen, ↓ Progesterone dominance, ↑ Prostaglandins, ↑ Oxytocin receptors * **Uterine activity:** Coordinated, rhythmic contractions starting from fundus * **Cervical changes:** Effacement and dilatation due to collagen remodeling * **Fetal contribution:** Fetal HPA axis activation and cortisol release --- ## **Stages of Normal Labour** ### **First Stage of Labour** **From onset of true labour pains to full cervical dilatation (10 cm)** #### Latent Phase * Cervical dilatation: 0–3/4 cm * Contractions: Mild, irregular * Duration: * Primigravida: up to 8–12 hours * Multigravida: shorter #### Active Phase * Cervical dilatation: 4–10 cm * Contractions: Regular, strong, 3–5 per 10 minutes * Rate of dilatation: * Primigravida: ~1 cm/hour * Multigravida: ~1.5 cm/hour --- ### **Second Stage of Labour** **From full dilatation to delivery of the fetus** * Duration: * Primigravida: ≤2 hours (≤3 hours with epidural) * Multigravida: ≤1 hour * Mechanism of labour occurs: * Engagement * Descent * Flexion * Internal rotation * Extension * Restitution and external rotation * Expulsion --- ### **Third Stage of Labour** **From delivery of fetus to expulsion of placenta** * Duration: ≤30 minutes * Placental separation mechanisms: * Schultze (central separation) * Duncan (marginal separation) * Managed actively to prevent postpartum hemorrhage --- ## **Mechanism of Normal Labour (Vertex Presentation)** 1. Engagement 2. Descent 3. Flexion 4. Internal rotation 5. Extension 6. Restitution 7. External rotation 8. Expulsion --- ## **Signs of True Labour** * Regular, painful uterine contractions * Progressive cervical effacement and dilatation * Show (blood-stained mucus) * Descent of presenting part --- ## **Monitoring in Normal Labour** * **Maternal:** Pulse, BP, temperature, uterine contractions * **Fetal:** Fetal heart rate monitoring * **Progress:** Partograph assessment of cervical dilatation, descent, and contractions --- ## **Management Principles of Normal Labour** * Supportive care and reassurance * Adequate hydration and nutrition * Pain relief (non-pharmacologic or pharmacologic) * Asepsis and bladder care * Continuous monitoring for deviations from normal --- ## **Outcome of Normal Labour** * Vaginal birth without complications * Minimal maternal morbidity * Healthy neonate with good Apgar score --- ## **Clinical Importance** * Benchmark for identifying **abnormal labour patterns** * Essential for **obstetric exams**, labour ward practice, and safe maternal care * Basis for using **partograph** and deciding interventions --- If you want, I can next provide: * **SEO title, meta description, and keywords** * **Abnormal labour comparison** * **Partograph-based exam notes** * **MCQs or case-based questions in HTML/CSS/JS (single file, modern UI)**
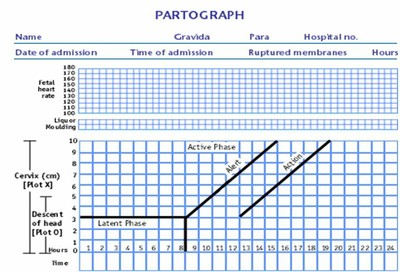
Partogram in Obstetrics Complete Guide for Monitoring Labour Progress
Below is a **single-place, exam-ready, clinically complete, SEO-friendly reference** on **Partogram**, written in a **clear H1–H4 structure** suitable for medical students, nurses, midwives, and clinicians. --- # **Partogram in Obstetrics: Complete Guide for Monitoring Labour Progress** ## **Introduction to Partogram** A **partogram (partograph)** is a **graphical tool** used to **monitor the progress of labour**, assess **maternal and fetal well-being**, and guide **timely clinical interventions**. It is a **WHO-recommended, low-cost, high-impact tool** for preventing **prolonged and obstructed labour**, thereby reducing **maternal and perinatal morbidity and mortality**. --- ## **Definition of Partogram** A **partogram** is a **chart that plots cervical dilatation against time**, along with **uterine contractions, fetal condition, and maternal parameters**, to provide a **continuous visual record of labour**. --- ## **Objectives of Using a Partogram** * Detect **abnormal labour progress early** * Identify **prolonged labour** * Prevent **obstructed labour** * Reduce **maternal complications** (PPH, sepsis, uterine rupture) * Reduce **fetal complications** (birth asphyxia, stillbirth) * Assist in **decision-making and referral** --- ## **Types of Partogram** ### **1. WHO Modified Partogram** * **Active phase starts at 4 cm cervical dilatation** * **Latent phase excluded** * Most commonly used in clinical practice ### **2. WHO Composite Partogram (Older)** * Includes **latent and active phase** * Latent phase up to **8 hours** * Less commonly used now ### **3. Simplified Partogram** * Focuses on **key parameters only** * Used in **low-resource settings** --- ## **Components of a Partogram** ### **A. Fetal Condition** Monitored to assess fetal well-being. #### **1. Fetal Heart Rate (FHR)** * Recorded **every 30 minutes** * Normal: **110–160 beats/min** * Abnormal: * <110 → Bradycardia * > 160 → Tachycardia #### **2. Amniotic Fluid** * **I** – Intact membranes * **C** – Clear liquor * **M** – Meconium-stained * **B** – Blood-stained #### **3. Moulding of Fetal Skull** * 0 → Sutures separated * * → Sutures touching * ++ → Sutures overlapping (reducible) * +++ → Sutures overlapping (irreducible) → **danger sign** --- ### **B. Progress of Labour** #### **1. Cervical Dilatation** * Plotted with **X** * Expected rate in active phase: **≥1 cm/hour** * Starts at **4 cm** #### **2. Descent of Head** * Plotted with **O** * Measured in **fifths palpable abdominally** * Or by **station (–5 to +5)** --- ### **C. Uterine Contractions** Recorded **every 30 minutes**: | Number / 10 min | Interpretation | | --------------- | ---------------- | | <2 | Inadequate | | 3–4 | Adequate | | ≥5 | Hyperstimulation | **Duration**: * <20 sec – Mild * 20–40 sec – Moderate * > 40 sec – Strong --- ### **D. Alert Line and Action Line** #### **Alert Line** * Drawn from **4 cm to full dilatation at 1 cm/hour** * Labour to the **left** → Normal * Crossing → **Slow progress** #### **Action Line** * Drawn **4 hours to the right of alert line** * Crossing → **Immediate intervention required** --- ### **E. Maternal Condition** #### **1. Pulse** * Every **30 minutes** #### **2. Blood Pressure** * Every **4 hours** * More frequent if abnormal #### **3. Temperature** * Every **2 hours** #### **4. Urine Examination** * Volume * Protein * Ketones --- ## **Interpretation of Partogram** ### **Normal Labour** * Cervical dilatation remains **left of alert line** * Adequate contractions * Normal fetal heart rate ### **Prolonged Labour** * Cervical dilatation crosses **alert line** * Requires: * Re-assessment * Amniotomy * Oxytocin augmentation * Referral if needed ### **Obstructed Labour** * Cervical dilatation reaches **action line** * Features: * No descent of head * Severe moulding (+++) * Maternal exhaustion * Management: * Operative delivery (CS / instrumental) --- ## **Indications for Using a Partogram** * All women in **active labour** * Especially useful in: * Primigravida * Induced labour * Previous prolonged labour * Referral cases --- ## **Contraindications / Limitations** * Not used in **latent phase (<4 cm)** * Less effective without **trained staff** * Requires **regular monitoring** --- ## **Advantages of Partogram** * Simple and cost-effective * Visual and easy to interpret * Reduces: * Prolonged labour * Obstructed labour * Unnecessary interventions * Improves maternal and neonatal outcomes --- ## **Disadvantages** * Incorrect plotting may mislead decisions * Requires training and adherence * Limited use without timely action --- ## **Role of Partogram in Modern Obstetrics** * Key tool in **Safe Motherhood Initiative** * Recommended by **WHO, FIGO** * Essential in **institutional deliveries** * Supports **evidence-based labour management** --- ## **Exam-Oriented Clinical Pearls** * **Alert line crossing** → Observe and evaluate * **Action line crossing** → Act immediately * **Moulding +++** → Suggests CPD * **Meconium liquor** → Fetal distress * **Rate <1 cm/hr** → Prolonged labour --- ## **Conclusion** The **partogram is a cornerstone of intrapartum care**, enabling **early detection of abnormal labour**, guiding **timely interventions**, and significantly improving **maternal and neonatal outcomes**. Proper understanding and correct use of the partogram are essential skills for all healthcare providers involved in childbirth. --- If you want next: * **SEO title, meta description, and keywords** * **Image-based explanation** * **25 hard case-based MCQs** * **HTML CSS JS interactive partogram simulator** Just tell me 👍
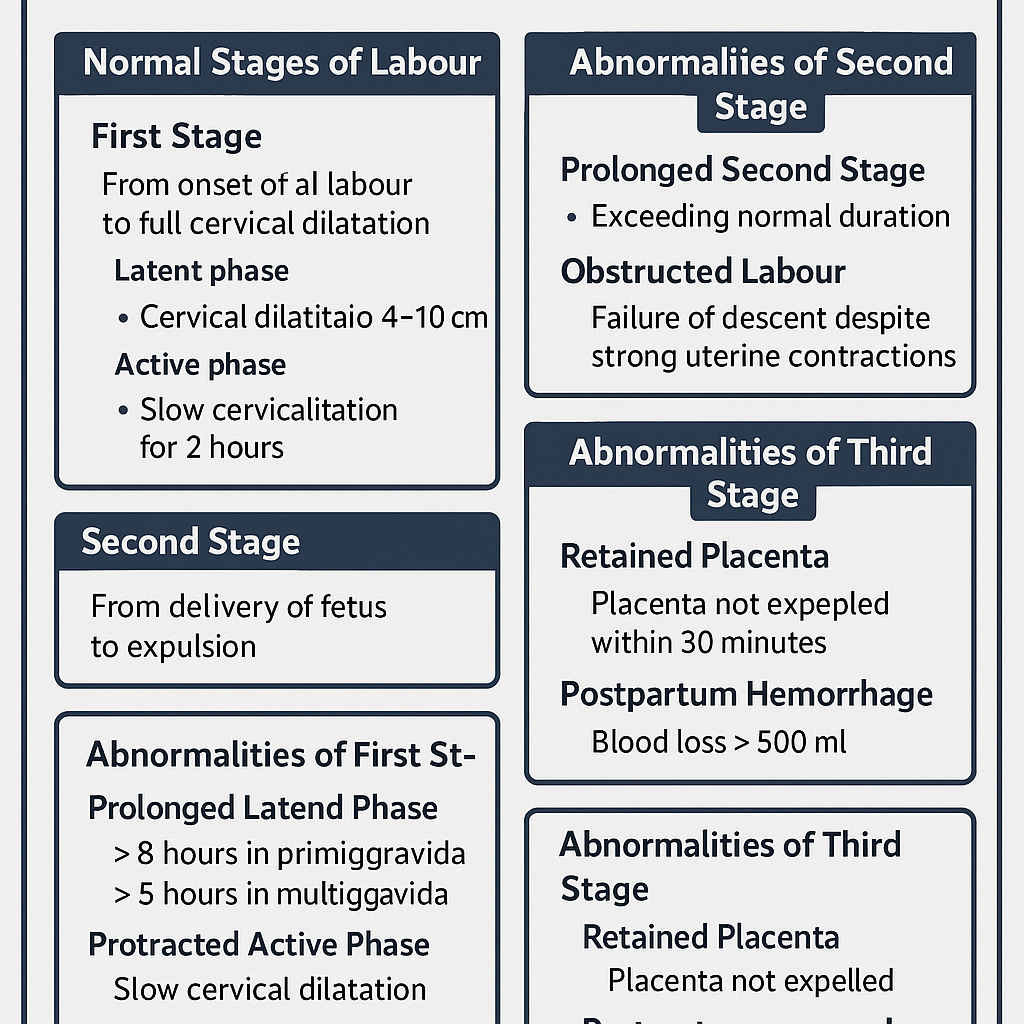
Stages of Labour Normal and Abnormal Progress Complete Clinical Guide
## **Stages of Labour Normal and Abnormal Progress Complete Clinical Guide** ### **SEO Description** Comprehensive obstetrics guide explaining normal and abnormal stages of labour with mechanisms, duration, clinical features, diagnosis, complications, and management for exams and clinical practice. ### **SEO Keywords** stages of labour, normal labour stages, abnormal labour, prolonged labour, obstructed labour, dysfunctional labour, first stage labour, second stage labour, third stage labour, active labour management, obstetrics labour guide --- # **Stages of Labour Normal and Abnormal** Labour is the **physiological process by which the fetus, placenta, and membranes are expelled from the uterus after fetal viability** through coordinated uterine contractions resulting in cervical effacement and dilatation. --- ## **Classification of Labour** * **Normal Labour**: Spontaneous onset, singleton, cephalic presentation, term pregnancy, no complications, vaginal delivery. * **Abnormal Labour**: Any deviation in onset, duration, progress, or outcome of labour. --- # **Normal Stages of Labour** ## **First Stage of Labour** **Definition:** Period from onset of true labour pains to full cervical dilatation (10 cm). ### **Phases** #### **Latent Phase** * Cervical dilatation: 0–3 cm * Cervical effacement occurs * Contractions mild to moderate * Duration: * Primigravida: up to 8 hours * Multigravida: up to 5 hours #### **Active Phase** * Cervical dilatation: 4–10 cm * Rapid dilatation * Strong, regular contractions * Rate of dilatation: * Primigravida: ~1 cm/hour * Multigravida: ~1.5 cm/hour ### **Normal Mechanism** * Uterine contractions * Cervical effacement and dilatation * Formation of forewaters and bulging membranes --- ## **Second Stage of Labour** **Definition:** Period from full cervical dilatation to delivery of the fetus. ### **Characteristics** * Strong expulsive uterine contractions * Voluntary maternal bearing down * Fetal descent, flexion, rotation, extension, restitution, expulsion ### **Duration** * Primigravida: up to 2 hours (3 hours with epidural) * Multigravida: up to 1 hour (2 hours with epidural) --- ## **Third Stage of Labour** **Definition:** Period from delivery of fetus to expulsion of placenta and membranes. ### **Mechanism** * Placental separation * Placental descent * Placental expulsion ### **Duration** * Usually within 5–15 minutes * Maximum acceptable: 30 minutes ### **Signs of Placental Separation** * Uterus becomes globular and firm * Lengthening of umbilical cord * Sudden gush of blood * Uterine fundus rises --- # **Abnormal Labour** Abnormal labour occurs due to problems related to **powers, passenger, or passage**. --- ## **Abnormalities of First Stage** ### **Prolonged Latent Phase** * > 8 hours in primigravida * > 5 hours in multigravida > **Causes** * Ineffective uterine contractions * Anxiety, dehydration * False labour **Management** * Reassurance * Hydration and analgesia * Rule out cephalopelvic disproportion --- ### **Protracted Active Phase** * Slow cervical dilatation **Causes** * Uterine inertia * Malposition * Mild CPD **Management** * Partograph monitoring * Amniotomy * Oxytocin augmentation if indicated --- ### **Arrest of Dilatation** * No cervical dilatation for 2 hours **Causes** * Obstructed labour * Malpresentation **Management** * Evaluate cause * Cesarean delivery if obstruction present --- ## **Abnormalities of Second Stage** ### **Prolonged Second Stage** * Exceeds normal duration **Causes** * Ineffective pushing * Epidural analgesia * Fetal malposition * Pelvic inadequacy **Complications** * Maternal exhaustion * Fetal distress **Management** * Assisted vaginal delivery * Cesarean section if indicated --- ### **Obstructed Labour** **Definition:** Failure of descent despite strong uterine contractions. **Causes** * Cephalopelvic disproportion * Fetal anomalies * Pelvic tumors **Complications** * Uterine rupture * Fetal hypoxia **Management** * Emergency cesarean section --- ## **Abnormalities of Third Stage** ### **Retained Placenta** * Placenta not expelled within 30 minutes **Types** * Placenta adherens * Trapped placenta * Placenta accreta spectrum **Management** * Active management * Manual removal under anesthesia --- ### **Postpartum Hemorrhage** * Blood loss >500 ml vaginal delivery **Causes** * Uterine atony * Retained placental tissue **Management** * Uterotonics * Bimanual compression * Surgical intervention if required --- # **Clinical Monitoring of Labour** * Partograph use * Fetal heart rate monitoring * Maternal vitals * Progress of cervical dilatation and descent --- # **Summary Table** | Stage | Normal Duration | Common Abnormalities | | ------ | --------------- | ---------------------- | | First | Latent + Active | Prolonged, Arrest | | Second | ≤2 hours | Prolonged, Obstructed | | Third | ≤30 minutes | Retained placenta, PPH | --- ## **Key Exam Pearls** * Active phase starts at 4 cm dilatation * Arrest disorders require prompt intervention * Third stage complications cause most maternal morbidity * Partograph is essential for early detection of abnormal labour --- If you want, I can **add MCQs, case based questions, management algorithms, or convert this into an exam-ready PDF or website content**.
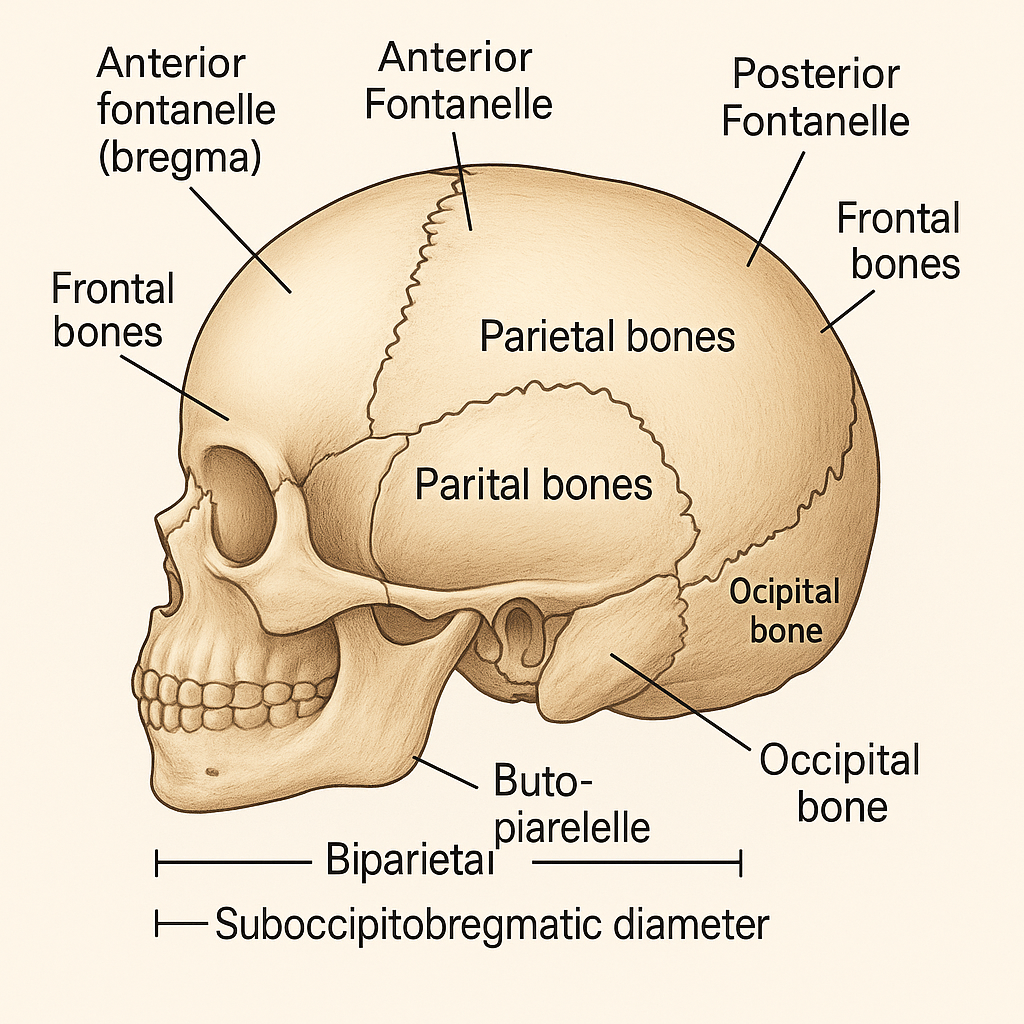
Fetal Skull Anatomy in Obstetrics: Sutures, Fontanelles, Diameters and Clinical Importance
## **SEO Title** **Fetal Skull Anatomy in Obstetrics: Sutures, Fontanelles, Diameters and Clinical Importance** ## **Meta Description** Comprehensive obstetrics-focused guide on fetal skull anatomy covering bones, sutures, fontanelles, diameters, molding, and their clinical significance during labor and delivery. ## **SEO Keywords** fetal skull obstetrics, fetal skull anatomy, sutures of fetal skull, fontanelles fetal skull, fetal skull diameters, molding of fetal skull, obstetric diameters, fetal head engagement, labor mechanism fetal skull --- # **Fetal Skull – Complete Obstetric Guide** ## **Introduction** The **fetal skull** is the most important part of the fetus in obstetrics because its **size, shape, flexibility, and diameters** determine the **mechanism of labor**, engagement, descent, and mode of delivery. --- ## **1. Structure of the Fetal Skull** The fetal skull is divided into **three main parts**: ### **A. Vault (Cranium) – Obstetrically Most Important** * Formed by **membranous bones** * Flexible and compressible * Allows **molding during labor** **Bones of the vault:** * 2 Frontal bones * 2 Parietal bones * Upper part of occipital bone --- ### **B. Base of the Skull** * Formed by **cartilaginous bones** * Rigid and non-compressible * Not affected by molding **Bones include:** * Sphenoid * Temporal * Lower occipital bone --- ### **C. Face** * Small obstetric significance * Important in **face presentation** --- ## **2. Sutures of the Fetal Skull** **Sutures** are fibrous joints between skull bones that allow overlapping during labor. | Suture | Location | Obstetric Importance | | ---------------------------- | ---------------------------------- | ---------------------------- | | **Sagittal suture** | Between parietal bones | Determines head position | | **Coronal suture** | Between frontal & parietal bones | Identifies degree of flexion | | **Lambdoid suture** | Between parietal & occipital bones | Helps locate occiput | | **Frontal (metopic) suture** | Between frontal bones | Indicates head attitude | --- ## **3. Fontanelles** Fontanelles are **membranous gaps** at the junction of sutures. ### **A. Anterior Fontanelle (Bregma)** * Diamond-shaped * Junction of **sagittal, coronal, and frontal sutures** * Closes by **18 months** * Palpation indicates **deflexed head** ### **B. Posterior Fontanelle (Lambda)** * Triangular * Junction of **sagittal and lambdoid sutures** * Closes by **6–8 weeks** * Palpation indicates **well-flexed vertex** **👉 Posterior fontanelle is the key landmark in normal labor** --- ## **4. Diameters of the Fetal Skull** Diameters are classified into **transverse and anteroposterior**. ### **A. Transverse Diameters** | Diameter | Measurement | Importance | | ----------------------------- | ----------- | ----------------- | | **Biparietal diameter (BPD)** | **9.5 cm** | Engaging diameter | | Bitemporal | 8 cm | Internal fit | | Bimastoid | 7.5 cm | Base diameter | --- ### **B. Anteroposterior Diameters** | Diameter | Measurement | Presentation | | ------------------------ | ----------- | -------------------------- | | **Suboccipitobregmatic** | **9.5 cm** | Well-flexed vertex (ideal) | | Suboccipitofrontal | 10 cm | Incomplete flexion | | Occipitofrontal | 11.5 cm | Deflexed vertex | | Mentovertical | 13.5 cm | Brow presentation | | Submentobregmatic | 9.5 cm | Face presentation | --- ## **5. Circumferences of the Fetal Head** | Circumference | Measurement | | -------------------- | ----------- | | Suboccipitobregmatic | ~32 cm | | Occipitofrontal | ~34 cm | | Mentovertical | ~38 cm | --- ## **6. Molding of the Fetal Skull** **Molding** refers to **overlapping of skull bones during labor**. ### **Grades of Molding** * **+ (Mild):** Sutures touching * **++ (Moderate):** Sutures overlapping but reducible * **+++ (Severe):** Overlapping not reducible (suggests CPD) **Clinical Importance** * Facilitates vaginal delivery * Excessive molding → fetal distress or obstructed labor --- ## **7. Caput Succedaneum** * Edematous swelling of scalp * Crosses suture lines * Appears at birth * Resolves spontaneously --- ## **8. Cephalhematoma** * Subperiosteal hemorrhage * Does **not cross suture lines** * Appears hours after birth * Resolves slowly --- ## **9. Obstetric Importance of the Fetal Skull** * Determines **engagement** * Helps assess **presentation and position** * Influences **mechanism of labor** * Guides **decision for vaginal delivery vs cesarean** * Critical in diagnosing **CPD and malpresentations** --- ## **Key Clinical Points** * **Best diameter for vaginal delivery:** Suboccipitobregmatic (9.5 cm) * **Most dangerous presentation:** Brow (mentovertical 13.5 cm) * **Posterior fontanelle palpable → normal vertex** * **Excessive molding → obstructed labor** --- If you want, I can also provide: * **SEO FAQs** * **Exam-oriented tables** * **25 hard case-based MCQs in HTML/CSS/JS (single file, modern UI)** * **Illustration prompts for image generation** Just tell me 👍

Contracted Pelvis and Cephalopelvic Disproportion Types Diagnosis Management
Below is a **concise yet complete, exam-oriented and SEO-friendly medical reference** covering **Contracted Pelvis, Cephalopelvic Disproportion (CPD), and Types of Pelvis**. Structured with **H1–H4 headings**, keyword-rich language, and clear clinical flow. **No images included**, as requested. --- # Contracted Pelvis and Cephalopelvic Disproportion: Types, Diagnosis and Management ## Introduction **Contracted pelvis** and **cephalopelvic disproportion (CPD)** are major causes of **obstructed labor**, **prolonged labor**, and **operative delivery**. Understanding **pelvic anatomy**, **pelvic types**, and **fetal–pelvic relationships** is essential for safe obstetric practice. --- ## Contracted Pelvis ### Definition A **contracted pelvis** is a pelvis in which **one or more pelvic diameters are reduced** below normal, interfering with the **descent and delivery of the fetus**. --- ### Causes of Contracted Pelvis #### Developmental Causes * Congenital pelvic abnormalities * Malnutrition during childhood * Rickets and osteomalacia #### Acquired Causes * Pelvic fractures with malunion * Tuberculosis of bones * Spinal deformities (kyphosis, scoliosis) * Previous pelvic surgery --- ### Classification of Contracted Pelvis #### 1. Anatomical Contracted Pelvis * **True contraction** of one or more diameters * Diagnosed by **pelvimetry** #### 2. Functional Contracted Pelvis * Pelvic diameters normal * Obstruction due to: * Large fetus * Malposition or malpresentation * Deflexed fetal head --- ### Degrees of Contracted Pelvis (Based on Obstetric Conjugate) | Degree | Obstetric Conjugate | Clinical Significance | | -------- | ------------------- | ------------------------- | | Mild | 9–10 cm | Vaginal delivery possible | | Moderate | 7.5–9 cm | Trial of labor | | Severe | <7.5 cm | Cesarean section | --- ## Cephalopelvic Disproportion (CPD) ### Definition **Cephalopelvic disproportion** occurs when the **fetal head is too large** or the **maternal pelvis too small** to allow vaginal delivery. --- ### Types of CPD #### 1. Absolute CPD * Gross pelvic contraction * Vaginal delivery **impossible** #### 2. Relative CPD * Borderline pelvis * Delivery depends on: * Fetal head molding * Position and attitude * Strength of uterine contractions --- ### Causes of CPD #### Maternal Factors * Contracted pelvis * Pelvic tumors * Short stature #### Fetal Factors * Macrosomia * Hydrocephalus * Occipitoposterior position * Deflexed head --- ### Clinical Features of CPD * Failure of head engagement * Prolonged labor * Cervical dystocia * Increasing caput and molding * Maternal exhaustion * Fetal distress --- ### Diagnosis of CPD #### Antenatal Assessment * History of difficult labor * Clinical pelvimetry * Ultrasound for fetal weight #### Intrapartum Diagnosis * Lack of descent despite good contractions * Non-progress of labor * Rising Bandl’s ring --- ### Management of CPD #### Antenatal * Identify high-risk cases * Plan mode of delivery #### Intrapartum * **Trial of labor** in selected cases * Continuous maternal and fetal monitoring #### Definitive Management * **Cesarean section** for: * Absolute CPD * Failed trial of labor * Fetal distress --- ## Types of Pelvis (Caldwell–Moloy Classification) ### 1. Gynecoid Pelvis * Most favorable for vaginal delivery * Rounded inlet * Wide subpubic angle * Straight side walls --- ### 2. Android Pelvis * Male-type pelvis * Heart-shaped inlet * Narrow mid-pelvis * Common cause of **arrest of descent** --- ### 3. Anthropoid Pelvis * Oval inlet (anteroposterior diameter increased) * Occipitoposterior position common * Vaginal delivery usually possible --- ### 4. Platypelloid Pelvis * Flattened pelvis * Wide transverse diameter * Narrow anteroposterior diameter * Engagement delayed --- ## Comparison of Pelvic Types | Pelvic Type | Inlet Shape | Labor Outcome | | ------------ | ------------ | ------------------ | | Gynecoid | Round | Best | | Android | Heart-shaped | Difficult | | Anthropoid | Oval (AP) | OP common | | Platypelloid | Flat | Engagement delayed | --- ## Clinical Importance * Major determinant of **mode of delivery** * Prevention of **obstructed labor** * Reduces maternal and perinatal morbidity * Essential for **exam preparation** and **clinical decision-making** --- ## Conclusion **Contracted pelvis and CPD** remain critical challenges in obstetrics. Accurate **pelvic assessment**, understanding **pelvic types**, and timely intervention ensure safe outcomes for both mother and fetus. --- ### SEO Keywords (Comma-Separated) contracted pelvis, cephalopelvic disproportion, CPD in obstetrics, types of pelvis, gynecoid pelvis, android pelvis, anthropoid pelvis, platypelloid pelvis, obstructed labor causes, pelvic contraction degrees, CPD diagnosis management If you want, I can also provide **case-based MCQs**, **exam notes**, or a **single-file HTML CSS JS quiz** on this topic.
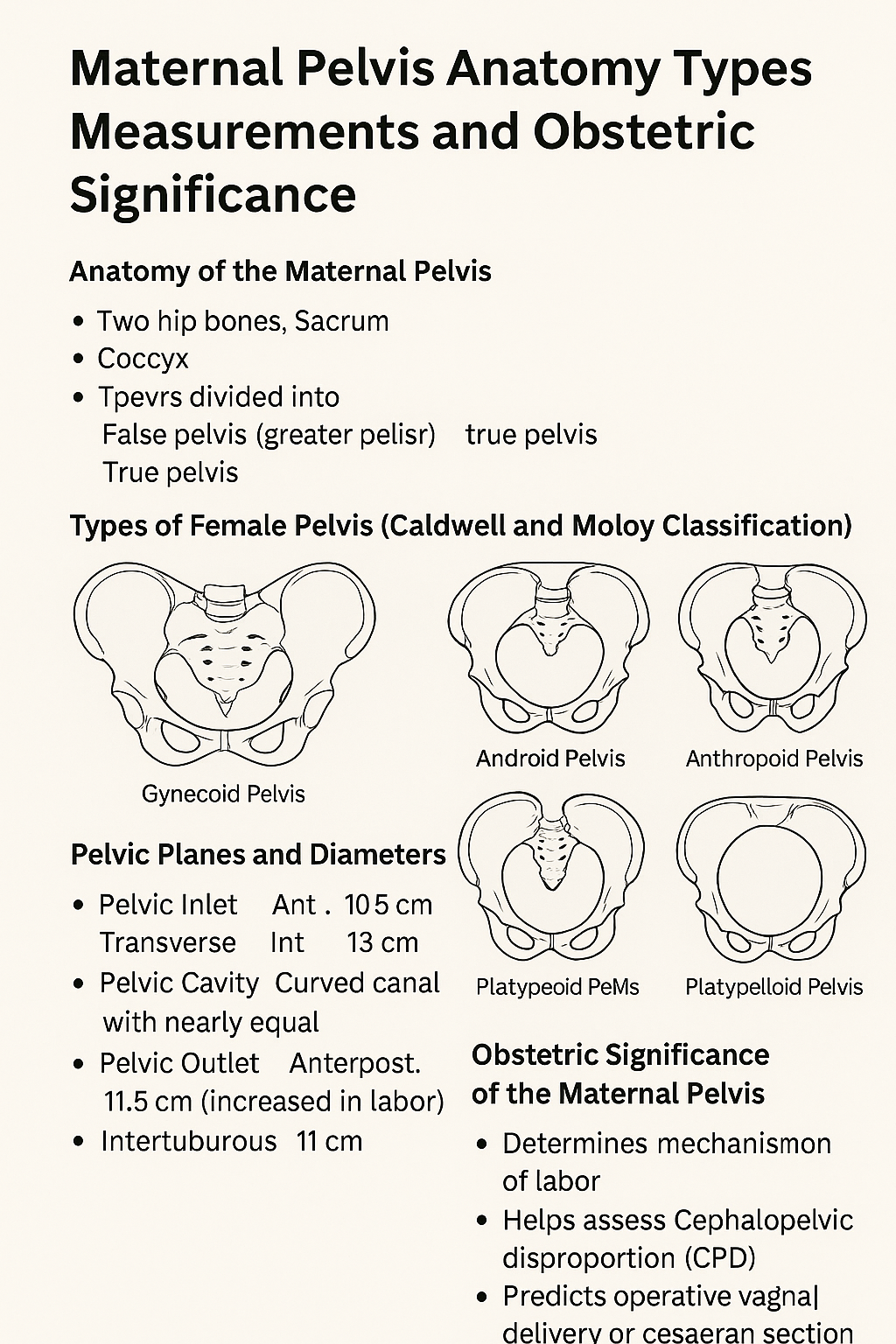
Maternal Pelvis Anatomy Types Measurements and Obstetric Significance
# **Maternal Pelvis Anatomy Types Measurements and Obstetric Significance** ## **Introduction** The **maternal pelvis** is a rigid bony structure that forms the birth canal. Its **shape, size, and dimensions** are critical determinants of **labor progression, fetal descent, and delivery outcome**. In obstetrics, detailed assessment of the maternal pelvis helps predict **normal vaginal delivery, obstructed labor, and cephalopelvic disproportion**. --- ## **Anatomy of the Maternal Pelvis** ### **1. Bones Forming the Pelvis** * **Two hip bones** (each formed by ilium, ischium, and pubis) * **Sacrum** * **Coccyx** These bones unite to form a **bony ring** that supports pelvic organs and provides a passage for childbirth. --- ## **Divisions of the Maternal Pelvis** ### **1. False Pelvis (Greater Pelvis)** * Located above the pelvic brim * Supports the gravid uterus * Has **no direct role in labor** ### **2. True Pelvis (Lesser Pelvis)** * Located below the pelvic brim * Forms the **birth canal** * Obstetrically important part --- ## **Pelvic Brim (Inlet)** The pelvic brim separates the false and true pelvis. ### **Boundaries** * Sacral promontory (posterior) * Ala of sacrum * Linea terminalis * Upper border of pubic symphysis (anterior) --- ## **Planes and Diameters of the Maternal Pelvis** ### **1. Pelvic Inlet** **Important diameters** * **Anteroposterior (Obstetric conjugate)**: ~10.5 cm * **Transverse diameter**: ~13 cm * **Oblique diameter**: ~12 cm **Clinical importance** * Determines engagement of fetal head --- ### **2. Pelvic Cavity** * Curved canal with nearly equal AP and transverse diameters * Smooth lateral walls favor rotation of the fetal head --- ### **3. Pelvic Outlet** **Boundaries** * Ischial tuberosities * Coccyx * Lower border of pubic arch **Important diameters** * **Anteroposterior**: ~11.5 cm (increases during labor due to coccygeal movement) * **Intertuberous diameter**: ~11 cm **Clinical importance** * Determines completion of vaginal delivery --- ## **Types of Female Pelvis (Caldwell and Moloy Classification)** ### **1. Gynecoid Pelvis** * Rounded inlet * Wide subpubic angle * Straight side walls **Most favorable for vaginal delivery** ### **2. Android Pelvis** * Heart-shaped inlet * Narrow forepelvis * Prominent ischial spines **Associated with deep transverse arrest** ### **3. Anthropoid Pelvis** * Oval inlet with long AP diameter * Favors occipitoposterior positions **Vaginal delivery usually possible** ### **4. Platypelloid Pelvis** * Flattened inlet * Wide transverse diameter * Short AP diameter **Engagement may be difficult** --- ## **Obstetric Significance of the Maternal Pelvis** * Determines **mechanism of labor** * Helps assess **cephalopelvic disproportion** * Predicts **operative vaginal delivery or cesarean section** * Influences fetal head **engagement, rotation, and descent** --- ## **Clinical Assessment of the Maternal Pelvis** ### **1. Clinical Pelvimetry** * Performed per vaginum * Assesses pelvic inlet, cavity, and outlet ### **2. Imaging Pelvimetry** * X-ray, CT, or MRI pelvimetry * Reserved for selected cases --- ## **Common Obstetric Problems Related to Pelvis** * Contracted pelvis * Obstructed labor * Prolonged labor * Fetal malposition and malrotation --- ## **Conclusion** The **maternal pelvis** plays a decisive role in childbirth. Knowledge of **pelvic anatomy, dimensions, and pelvic types** is essential for safe obstetric practice, early identification of labor complications, and appropriate delivery planning. --- ### **SEO Keywords** maternal pelvis anatomy, types of female pelvis, obstetric pelvis, pelvic inlet outlet diameters, gynecoid pelvis, android pelvis, anthropoid pelvis, platypelloid pelvis, pelvic planes obstetrics, clinical pelvimetry If you want, I can **generate 25 hard case-based MCQs in a single HTML CSS JS file**, or **convert this into exam notes or infographic-ready content**.

Post Term Pregnancy and Fetal Macrosomia Causes Risks Diagnosis and Management
Below is a **SEO-friendly, exam-oriented, and clinically complete guide** on **Post-Term Pregnancy and Fetal Macrosomia**, written in clear **H1–H3 structure** and optimized for medical websites. --- ## **SEO Title** **Post Term Pregnancy and Fetal Macrosomia Clinical Guide 2025** --- ## **SEO Meta Description** Comprehensive medical guide on post term pregnancy and fetal macrosomia covering definition, causes, risks, diagnosis, management, induction of labor, complications, and prevention for obstetric practice and exams. --- ## **SEO Keywords** post term pregnancy, postdated pregnancy management, fetal macrosomia, macrosomia causes, post term pregnancy complications, induction of labor post term, macrosomic baby risks, shoulder dystocia, large for gestational age fetus, obstetrics clinical guide --- # **Post Term Pregnancy and Fetal Macrosomia** ## **1. Post Term Pregnancy** ### **Definition** Post term pregnancy is defined as a pregnancy that **extends beyond 42 completed weeks (≥294 days)** from the first day of the last menstrual period. --- ### **Classification** * **Late term:** 41⁰–41⁶ weeks * **Post term:** ≥42⁰ weeks --- ### **Etiology and Risk Factors** * Incorrect dating of pregnancy * Primigravida * Previous post term pregnancy * Male fetus * Maternal obesity * Genetic factors --- ### **Pathophysiology** * Progressive **placental aging and insufficiency** * Reduced uteroplacental perfusion * Oligohydramnios * Increased risk of fetal hypoxia --- ### **Maternal Complications** * Prolonged labor * Increased operative delivery * Perineal trauma * Postpartum hemorrhage * Infection --- ### **Fetal and Neonatal Complications** * Macrosomia * Meconium aspiration syndrome * Shoulder dystocia * Birth asphyxia * Stillbirth * Postmaturity syndrome (dry, peeling skin, decreased fat) --- ### **Diagnosis** * Accurate gestational age assessment (early ultrasound) * Fundal height * Ultrasound for: * Amniotic fluid index (AFI) * Estimated fetal weight * Fetal surveillance: * Non-stress test (NST) * Biophysical profile (BPP) --- ### **Management** * **41 weeks:** Begin antenatal surveillance * **≥41–42 weeks:** Induction of labor * **Cervical ripening:** Prostaglandins or Foley catheter * **Cesarean section:** If failed induction or fetal distress --- ## **2. Fetal Macrosomia** ### **Definition** Fetal macrosomia refers to a fetus with **birth weight ≥4,000 g** (some definitions use ≥4,500 g), irrespective of gestational age. --- ### **Risk Factors** * Maternal diabetes (gestational or pregestational) * Post term pregnancy * Maternal obesity * Excessive gestational weight gain * Multiparity * Previous macrosomic infant * Male fetus --- ### **Pathophysiology** * Maternal hyperglycemia → fetal hyperinsulinemia * Increased fat deposition and organ enlargement * Disproportionate growth of shoulders and trunk --- ### **Maternal Complications** * Prolonged labor * Operative vaginal delivery * Cesarean section * Postpartum hemorrhage * Genital tract injuries --- ### **Fetal and Neonatal Complications** * Shoulder dystocia * Brachial plexus injury * Clavicle fracture * Birth asphyxia * Neonatal hypoglycemia * Childhood obesity and metabolic syndrome --- ### **Diagnosis** * Clinical assessment (fundal height, Leopold maneuvers) * Ultrasound estimated fetal weight (EFW) * Limitations: ±10–15% error in late pregnancy --- ### **Management** * **Antenatal** * Optimize glycemic control * Monitor fetal growth * **Intrapartum** * Trial of labor if EFW <4,500 g (non-diabetic) * Elective cesarean if: * EFW ≥4,500 g (diabetic mother) * EFW ≥5,000 g (non-diabetic) * **Preparedness** * Anticipate shoulder dystocia * Skilled birth attendants --- ## **3. Relationship Between Post Term Pregnancy and Macrosomia** * Prolonged gestation allows continued fetal growth * Increased risk of large for gestational age fetus * Higher rates of operative delivery and birth trauma * Combined risk increases perinatal morbidity --- ## **4. Prevention Strategies** * Accurate pregnancy dating (first-trimester ultrasound) * Timely induction at 41 weeks * Optimal maternal weight and glucose control * Regular antenatal follow-up --- ## **5. Key Clinical Pearls** * Post term pregnancy significantly increases perinatal mortality * Macrosomia cannot be diagnosed with certainty antenatally * Induction at 41 weeks reduces stillbirth risk * Shoulder dystocia is the most feared complication of macrosomia --- If you want, I can next: * **Generate exam-oriented MCQs (HTML CSS JS single file)** * **Create FAQ schema for SEO** * **Generate medical illustrations** * **Convert this into a publish-ready SEO article page**
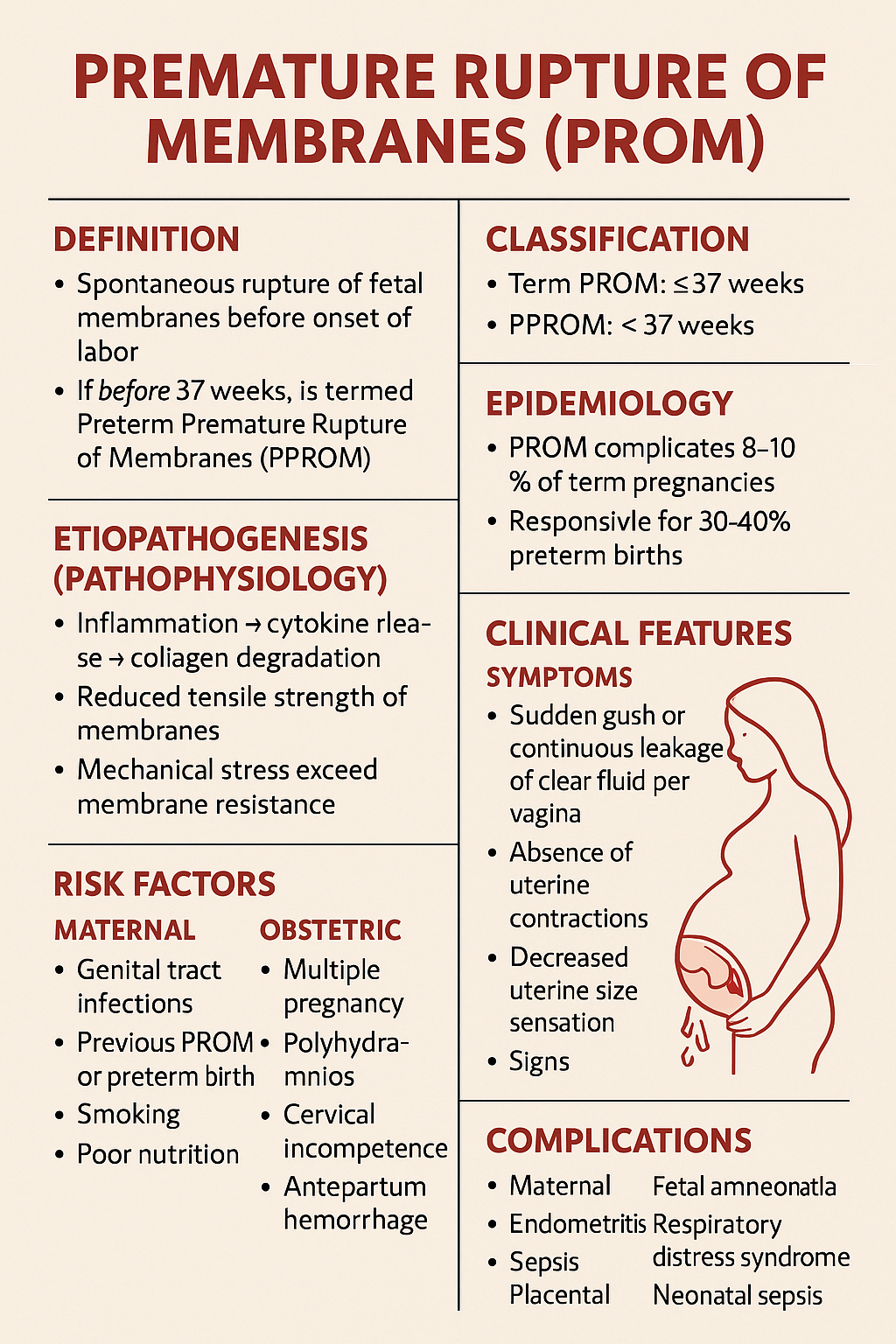
Premature Rupture of Membranes PROM – Causes Diagnosis Management and Complications
Below is a **complete, SEO-friendly, exam-oriented, single-place medical reference** on **Premature Rupture of Membranes (PROM)**, structured with clear **H1–H4 headings**, rich keywords, and clinically accurate content suitable for **medical students, clinicians, and health websites**. --- # **Premature Rupture of Membranes (PROM)** ## **Definition** **Premature Rupture of Membranes (PROM)** is defined as **spontaneous rupture of the fetal membranes before the onset of labor**, irrespective of gestational age. * If it occurs **before 37 completed weeks**, it is termed **Preterm Premature Rupture of Membranes (PPROM)**. --- ## **Classification** ### **1. Based on Gestational Age** * **Term PROM**: ≥ 37 weeks * **PPROM**: < 37 weeks ### **2. Based on Duration** * **Recent PROM**: < 18 hours * **Prolonged PROM**: ≥ 18 hours (↑ risk of infection) --- ## **Epidemiology** * PROM complicates **8–10% of term pregnancies** * PPROM accounts for **2–3% of all pregnancies** * Responsible for **30–40% of preterm births** --- ## **Etiopathogenesis (Pathophysiology)** ### **Normal Membrane Integrity** * Maintained by **collagen, elastin, and extracellular matrix** * Balance between **matrix synthesis and degradation** ### **Mechanisms Leading to PROM** * **Inflammation → cytokine release → collagen degradation** * **Reduced tensile strength of membranes** * **Mechanical stress exceeding membrane resistance** --- ## **Risk Factors** ### **Maternal Factors** * Genital tract infections (BV, UTI, STIs) * Previous PROM or preterm birth * Smoking * Poor nutrition * Low socioeconomic status ### **Obstetric Factors** * Multiple pregnancy * Polyhydramnios * Cervical incompetence * Antepartum hemorrhage ### **Iatrogenic Factors** * Amniocentesis * Cervical procedures --- ## **Clinical Features** ### **Symptoms** * Sudden **gush or continuous leakage of clear fluid per vagina** * Absence of uterine contractions initially * Decreased uterine size sensation ### **Signs** * Pooling of liquor in posterior fornix * Wet perineum * Reduced amniotic fluid volume --- ## **Diagnosis** ### **History** * Timing, amount, color, and odor of fluid * Associated fever, pain, reduced fetal movements ### **Physical Examination** * **Sterile speculum examination (preferred)** * Avoid digital vaginal examination unless in labor --- ### **Confirmatory Tests** #### **1. Bedside Tests** * **Nitrazine test**: Alkaline pH (false positives possible) * **Fern test**: Crystallization pattern on microscopy #### **2. Biochemical Tests** * PAMG-1 (AmniSure) * IGFBP-1 (Actim PROM) #### **3. Ultrasound** * Reduced Amniotic Fluid Index (AFI) * Assessment of fetal growth and presentation --- ## **Differential Diagnosis** * Urinary incontinence * Physiological vaginal discharge * Seminal fluid * Vaginal infections --- ## **Complications** ### **Maternal** * Chorioamnionitis * Endometritis * Sepsis * Placental abruption ### **Fetal and Neonatal** * Prematurity * Respiratory distress syndrome * Neonatal sepsis * Umbilical cord prolapse * Pulmonary hypoplasia (early PPROM) --- ## **Management of PROM** Management depends on **gestational age**, **infection status**, and **fetal condition**. --- ## **Management at Term PROM (≥ 37 Weeks)** ### **Principles** * Aim for **delivery** * Reduce infection risk ### **Management** * Induction of labor within **12–24 hours** * Oxytocin preferred * Prophylactic antibiotics if GBS positive --- ## **Management of PPROM (< 37 Weeks)** ### **General Principles** * Balance between **prematurity risks** and **infection risks** * Expectant management if stable --- ### **Stepwise Management** #### **1. Hospitalization and Monitoring** * Maternal vitals, fetal heart rate * Signs of infection #### **2. Antibiotic Therapy** **Indication**: Prolong latency, reduce infection **Standard Regimen** * Ampicillin IV → Amoxicillin oral * Erythromycin / Azithromycin **Benefits** * ↓ Chorioamnionitis * ↓ Neonatal sepsis * ↑ Latency period --- #### **3. Corticosteroids** **Indication**: 24–34 weeks **Drugs** * Betamethasone 12 mg IM × 2 doses (24 hours apart) **Benefits** * ↓ RDS * ↓ IVH * ↓ NEC --- #### **4. Tocolysis** * **Not routinely recommended** * Short-term use only to complete steroid course --- #### **5. Magnesium Sulfate** **Indication**: < 32 weeks **Purpose**: Fetal neuroprotection --- ### **Indications for Immediate Delivery** * Clinical chorioamnionitis * Non-reassuring fetal status * Placental abruption * Advanced labor * Severe oligohydramnios with distress --- ## **Prevention** * Screening and treatment of genital infections * Smoking cessation * Cervical cerclage in indicated cases * Adequate antenatal care --- ## **Prognosis** * **Term PROM**: Excellent with timely delivery * **PPROM**: Depends on gestational age and infection * Neonatal outcome improves significantly after **32–34 weeks** --- ## **Key Exam Points** * Avoid digital vaginal examination in PROM * Antibiotics increase latency in PPROM * Corticosteroids between 24–34 weeks * Infection = indication for delivery at any gestation --- ## **SEO Keywords (Comma-Separated)** premature rupture of membranes, prom pregnancy, pprom obstetrics, prom diagnosis management, preterm premature rupture membranes, prom complications, amniotic fluid leakage pregnancy, chorioamnionitis prom, prom treatment guidelines, pprom antibiotics steroids --- If you want, I can next: * Generate **SEO-optimized title and meta description** * Create **25 hard case-based MCQs (HTML CSS JS in one file)** * Generate **FAQ schema for SEO** * Provide **image prompts or medical diagrams**
Browse by Medical Category
Explore content organized by medical specialties and systems