Comprehensive guide on safe and unsafe drugs in pregnancy including antibiotics, anticoagulants, and antiepileptics. Covers risks, teratogenicity, and clinical management
Explore Related Content
- Home Latest medical posts
- Sitelinks Index Complete site map
- Upload Medical Content Share clinical pearls
- More OBSTETRICS AND GYNAECOLOGY Posts Browse related content
- Reviews & Suggestions Community feedback
- Help & FAQ Upload & SEO tips
- More from this Author View all posts
- About Streamora Medical learning hub
Related Posts
Posts with similar category or tags for stronger sitelinks & internal backlinks.
Aneuploidy Screening in Pregnancy: First Trimester, Quadruple Test, NIPT & Soft Markers | Complete Guide 2025
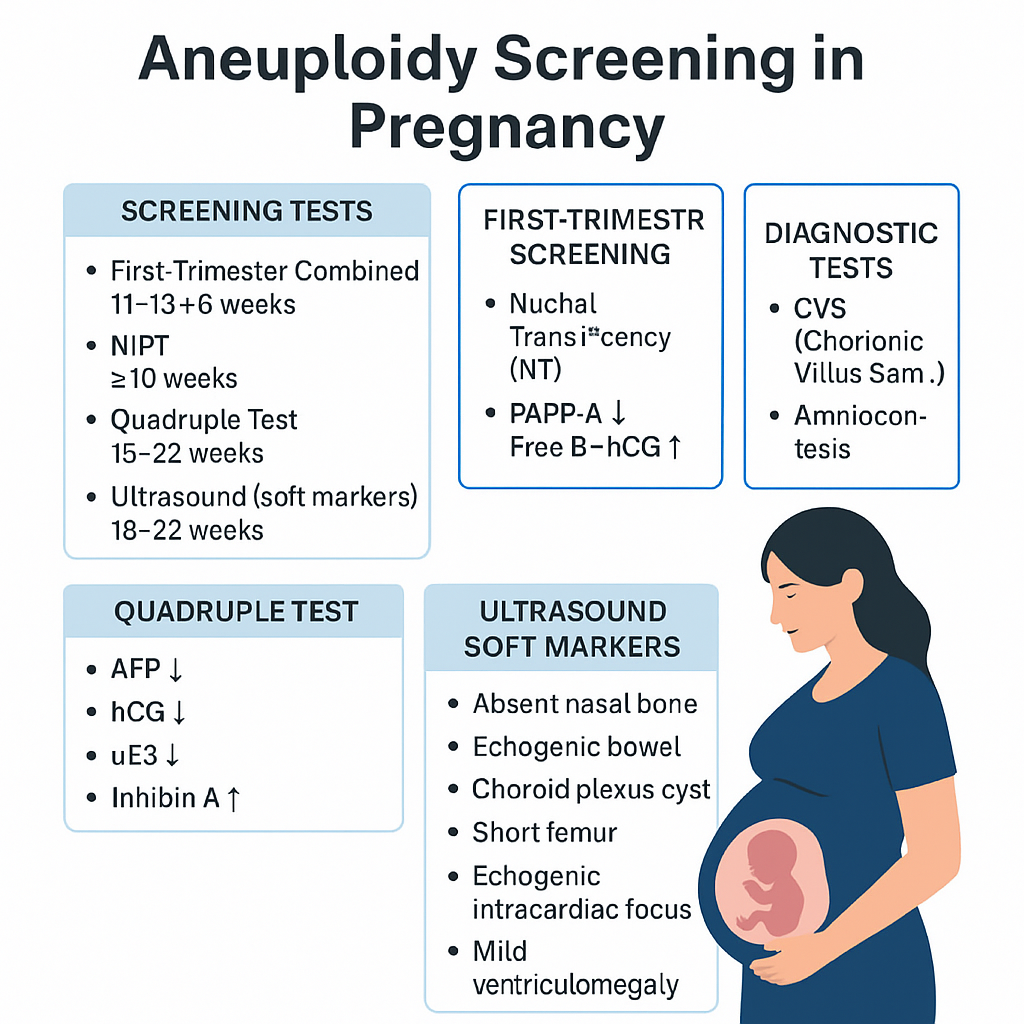
--- # ⭐ **Aneuploidy Screening in Pregnancy — Complete Obstetric Guide** Aneuploidy = **abnormal number of chromosomes** (most clinically relevant: **Trisomy 21, 18, 13**, Turner syndrome). Goal of screening = **identify pregnancies at increased risk** early enough to offer **diagnostic testing**. --- # **1. Why Aneuploidy Occurs (Basic Pathophysiology)** * **Meiotic nondisjunction** → failure of homologous chromosomes/sister chromatids to separate. * **Common in maternal meiosis I** (age-related). * **Trisomy 21 risk increases exponentially with maternal age**. * Mosaicism occurs if nondisjunction happens post-zygotically. --- # **2. High-Risk Factors** * Advanced maternal age (≥35 yrs). * Previous pregnancy with aneuploidy. * Parental balanced translocation (esp. Robertsonian). * Abnormal ultrasound markers (NT ↑, absent nasal bone, echogenic bowel, cardiac defects). * Abnormal biochemical screening results. --- # **3. Overview of Screening Timeline** | Gestation | Test | | ------------------- | ------------------------------------------------------------- | | **11–13+6 weeks** | First-trimester combined screening (NT + PAPP-A + free β-hCG) | | **10 weeks onward** | NIPT / cfDNA (highest accuracy) | | **15–22 weeks** | Second-trimester quadruple test | | **18–22 weeks** | Targeted anomaly scan (soft markers) | **Screening ≠ diagnosis.** Diagnostic tests = **CVS (10–13 wks)**, **Amniocentesis (≥15 wks)**, **FISH/karyotype/microarray**. --- # **4. First-Trimester Screening (11–13+6 Weeks)** ## **Components** 1. **Nuchal translucency (NT):** * Measured at CRL 45–84 mm * **NT >3.5 mm = major risk marker** * Increased NT → Trisomy 21/18/13, cardiac defects, Noonan syndrome, skeletal dysplasias 2. **Biochemical markers:** * **PAPP-A ↓**: Trisomy 21/18, placental insufficiency * **Free β-hCG ↑**: Trisomy 21 * **Free β-hCG ↓**: Trisomy 18/13 ## **Detection rate:** ~85–90% for T21 when combined. --- # **5. NIPT / cfDNA (Non-Invasive Prenatal Testing)** * Can be done **from 10 weeks onward**. * Analyzes **cell-free fetal DNA** in maternal blood. * **Most accurate screening test**. ## **Detects** * **Trisomy 21, 18, 13** * **Sex chromosome aneuploidies** (Turner, Klinefelter) * Microdeletions (low PPV, not recommended routinely) ## **Not diagnostic**, but: * **Sensitivity**: * T21 ≈ 99% * T18 ≈ 97–98% * T13 ≈ 92% ## **Causes of false results** * Confined placental mosaicism * Vanishing twin * Maternal malignancy * Low fetal fraction (<4%) --- # **6. Second-Trimester Quadruple Test (15–22 Weeks)** Markers: * **AFP** * **hCG** * **uE3 (unconjugated estriol)** * **Inhibin-A** ## **Patterns** ### **Trisomy 21** * **AFP ↓** * **uE3 ↓** * **hCG ↑** * **Inhibin-A ↑** ### **Trisomy 18** * **AFP ↓** * **uE3 ↓** * **hCG ↓** * **Inhibin-A normal** ### **Open neural tube defects** * **AFP ↑↑** Detection rate: * **~75% for T21** --- # **7. Ultrasound Soft Markers (18–22 Weeks)** ### **Major structural markers** * Cardiac defects (AV canal) → T21 * Holoprosencephaly → T13 * Omphalocele → T18 * Diaphragmatic hernia * Renal anomalies ### **Soft markers (non-structural)** | Marker | Association | | -------------------------------------- | --------------- | | **Absent nasal bone** | T21 | | **Echogenic intracardiac focus (EIF)** | Mild ↑ T21 risk | | **Echogenic bowel** | T21, CMV, CF | | **Short femur/humerus** | T21 | | **Choroid plexus cyst** | T18 | | **Single umbilical artery** | T18, T13 | | **Mild ventriculomegaly** | Aneuploidy risk | Soft markers **modify risk**, not diagnostic. --- # **8. Integrated & Sequential Screening** ### **Integrated test** * Combines first-trimester + second-trimester results * Highest combined detection before NIPT * Detection: **~94–95%**, but results available only in 2nd trimester ### **Sequential screening** * If first-trimester is high-risk → offer NIPT/CVS * If low-risk → continue with second trimester screening * More practical than integrated approach --- # **9. Diagnostic Tests (When Screening Is Positive)** ## **Chorionic Villus Sampling (CVS)** * **10–13+6 weeks** * Transcervical or transabdominal * Results: karyotype, microarray * Miscarriage risk: **~0.2–0.3%** ## **Amniocentesis** * **≥15 weeks** * Lower miscarriage risk: **0.1–0.2%** ## **Rapid tests** * **FISH** (24–48 hrs): detects T21, T18, T13 * **Microarray**: detects microdeletions/duplications --- # **10. Combined Detection Performance** | Test | Detection rate for T21 | | ------------------------ | ---------------------- | | First trimester combined | 85–90% | | Quadruple test | 75% | | Integrated screening | 94–95% | | **NIPT** | **>99%** | NIPT is **preferred**, especially for high-risk pregnancies. --- # **11. When to Offer NIPT (Indications)** * Maternal age ≥35 yrs * Previous trisomy pregnancy * Abnormal ultrasound markers * Positive biochemical screen * IVF pregnancies (optional but recommended) * Parental chromosomal rearrangement (screening may be inadequate → offer diagnostic test) --- # **12. Management Algorithm (Simplified)** ### **STEP 1: First antenatal visit** * Counsel regarding available screening methods * Offer **NIPT** to all (optimal) ### **STEP 2: If NT scan & biochemistry done** * **High-risk → NIPT or CVS** * **Intermediate risk → NIPT** * **Low risk → routine care** ### **STEP 3: Anomaly scan** * If any major structural abnormality → **Diagnostic test (CVS/Amniocentesis)** irrespective of NIPT result ### **STEP 4: If NIPT positive** * **Never terminate pregnancy based on NIPT alone** * Perform **confirmatory CVS/Amniocentesis** --- # **13. Counseling Points** * Screening ≠ diagnosis * Explain detection rates and false positives * Invasive diagnostic tests carry small miscarriage risks * A normal screen reduces but **does not eliminate** risk * Final decision is patient-centered --- # **14. Key Exam High-Yield Points** * **Most sensitive screening test:** NIPT * **Earliest diagnostic test:** CVS * **Best time for NT scan:** 11–13+6 weeks * **AFP ↑:** NTD, abdominal wall defects, incorrect dating * **AFP ↓ + hCG ↑ + uE3 ↓:** Trisomy 21 * **Choroid plexus cyst:** Trisomy 18 marker * **Absent nasal bone:** Down syndrome strongest soft marker * **Echogenic bowel:** Trisomy 21, CMV, CF ---
Antepartum Fetal Monitoring: Indications, NST, Biophysical Profile, Modified BPP & Vibroacoustic Test | Complete Obstetrics Guide 2025
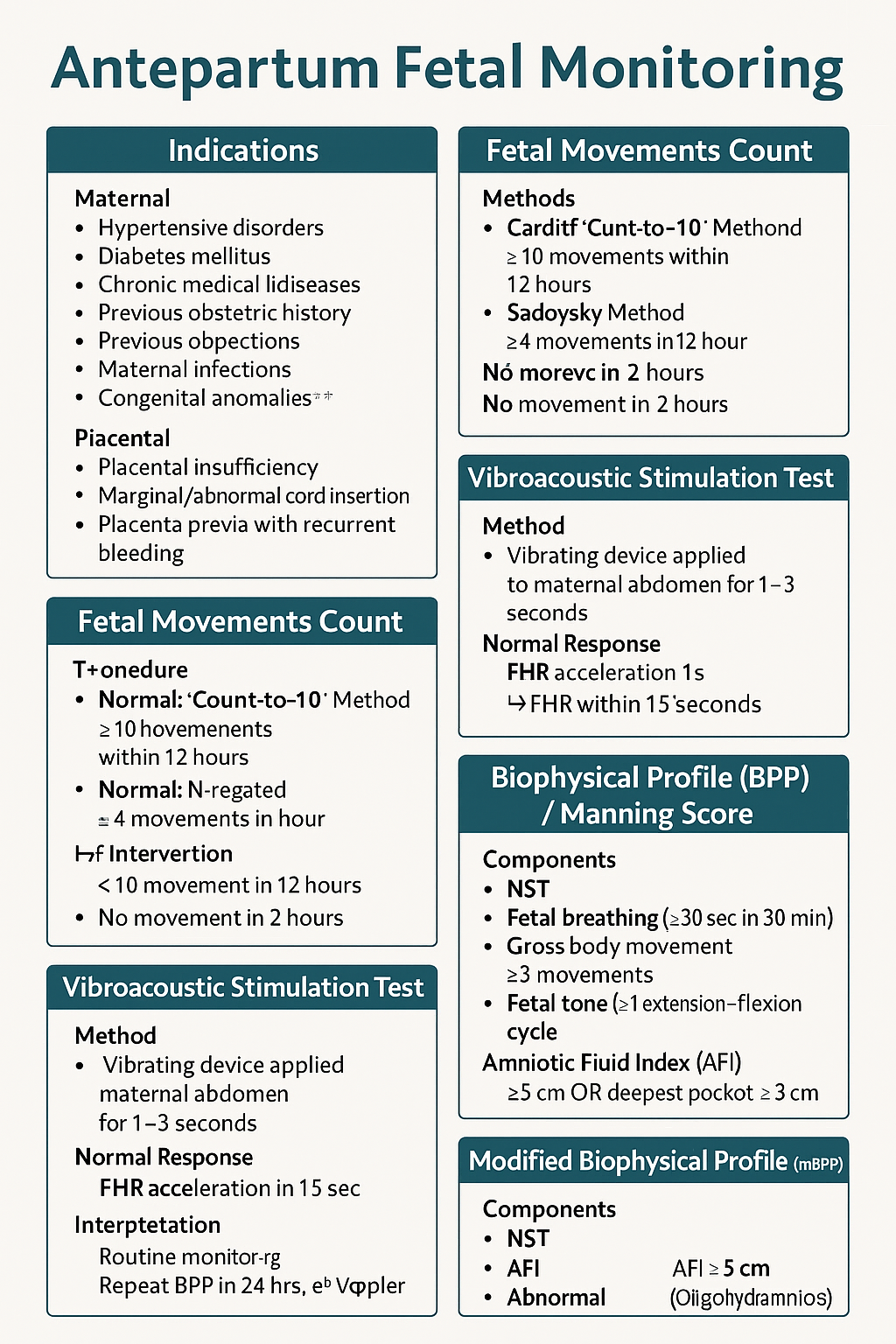
--- # ⭐ **ANTEPARTUM FETAL MONITORING — COMPLETE HIGH-YIELD REFERENCE (NEET PG / INI-CET)** Antepartum fetal surveillance aims to detect **early fetal hypoxia** to prevent stillbirth, reduce perinatal morbidity, and guide timing of delivery. It assesses **placental function**, **oxygenation**, **neurological integrity**, and **fetal compensatory mechanisms**. --- # **1️⃣ Indications for Antepartum Fetal Monitoring** ### **A. Maternal Indications** * **Hypertensive disorders:** Gestational HTN, preeclampsia, eclampsia * **Diabetes mellitus:** GDM requiring insulin/OADs, pre-gestational DM * **Chronic medical diseases:** * Chronic hypertension * Renal disease * Autoimmune disease (SLE, APLA syndrome) * Cardiac disease * Thyroid disease with complications * **Previous obstetric history:** * Previous stillbirth * Previous IUGR baby * Previous neonatal death * Isoimmunization/Rh alloimmunization * **Maternal infections:** TORCH with fetal involvement * **Advanced maternal age (>35)** * **Post-dated pregnancy (>40 weeks)** ### **B. Fetal Indications** * **Decreased fetal movements** * **IUGR (Symmetric/Asymmetric)** * **Oligohydramnios / Polyhydramnios** * **Multiple pregnancy with complications** * **Fetal anemia / hydrops** * **Congenital anomalies** ### **C. Placental Indications** * Placental insufficiency * Marginal/Abnormal cord insertion * Placenta previa with recurrent bleeding --- # **2️⃣ Fetal Movement Count (FMC / Kick Count)** Fetal movements reflect fetal well-being (neurological + metabolic status). ### **Methods** ### **A. Cardiff Count-to-10 Method** * Mother records movements daily. * **Normal:** 10 movements within 12 hours. ### **B. Sadovsky Method** * Count movements for 1 hour after meals. * **Normal:** ≥4 movements/hour. ### **When to worry?** * **<10 movements in 12 hours** * **<4 movements in 1 hour** * **No movement in 2 hours** → urgent evaluation (NST/BPP) ### **Management of Decreased Fetal Movements** 1. Immediate **NST** 2. If NST non-reactive → **BPP** 3. If BPP equivocal → **Doppler studies** 4. If evidence of fetal compromise → **Delivery based on GA** --- # **3️⃣ Non-Stress Test (NST)** NST measures **fetal heart rate accelerations** in response to fetal movements via cardiotocography. ### **Procedure** * Done after **28–32 weeks** (mature autonomic nervous system). * Duration: **20 minutes** (extend to 40 minutes if needed). --- ## **Interpretation (Reactive vs Non-Reactive)** ### ✔ **Reactive NST (Normal)** * **≥2 accelerations** in 20 minutes * Acceleration criteria: * **≥15 bpm for ≥15 sec** (≥32 weeks) * **≥10 bpm for ≥10 sec** (<32 weeks) ### ✔ **Non-Reactive NST** * <2 accelerations in 40 minutes * Suggests fetal sleep cycle, hypoxia, CNS depression. ### **Causes of Non-Reactive NST** * Fetal sleep * Maternal drug intake (MgSO₄, opioids, sedatives) * Hypoxia * Prematurity * Congenital anomalies ### **Next Steps in Non-Reactive NST** * Vibroacoustic stimulation test * BPP * Contraction stress test (rarely used today) * Doppler studies --- # **4️⃣ Vibroacoustic Stimulation Test (VAST)** Used to differentiate fetal sleep from hypoxia in non-reactive NST. ### **Method** * A vibrating device (artificial larynx) applied to maternal abdomen for **1–3 seconds**. ### **Normal Response** * FHR acceleration within **15 seconds** * Converts non-reactive NST → **reactive** ### **Significance** * High negative predictive value * Reduces need for BPP --- # **5️⃣ Biophysical Profile (BPP) / Manning Score** Combines **NST + ultrasound parameters** assessing fetal CNS integrity + oxygenation. ### **Components (Total 10 points)** Each gets **2 = normal**, **0 = abnormal** | Component | Normal Criteria (2 points) | | ------------------------------ | --------------------------------- | | **NST** | Reactive | | **Fetal breathing** | ≥30 sec in 30 min | | **Gross body movement** | ≥3 movements | | **Fetal tone** | ≥1 extension–flexion cycle | | **Amniotic Fluid Index (AFI)** | AFI ≥5 cm OR deepest pocket ≥2 cm | --- ## **Scoring & Interpretation** | Score | Interpretation | Management | | -------- | -------------- | ------------------------------------------- | | **8–10** | Normal | Routine monitoring | | **6** | Equivocal | Repeat BPP in 24 hrs; evaluate Doppler | | **4** | Abnormal | Risk of fetal hypoxia → Delivery if ≥34 wks | | **0–2** | Severe hypoxia | Immediate delivery | --- # **6️⃣ Modified Biophysical Profile (mBPP)** Simplified & widely used. ### **Components** 1. **NST** 2. **AFI (Amniotic Fluid Index)** ### **Interpretation** * **Normal:** Reactive NST + AFI ≥5 cm * **Abnormal:** * Non-reactive NST * AFI <5 cm (Oligohydramnios) → placental insufficiency ### **Management** * If abnormal mBPP → full BPP or Doppler; consider delivery based on GA. --- # **7️⃣ Contraction Stress Test (OBSOLETE mostly)** Assesses fetal response to **uterine contractions** → risk of late decelerations. Rarely done due to risk + availability of Doppler and BPP. --- # **8️⃣ Putting It All Together — Management Algorithm** ### **Decreased fetal movements →** 1. **NST** 2. If reactive → reassure 3. If non-reactive → repeat + VAST 4. If still non-reactive → BPP 5. * **BPP ≤4** → Delivery * **BPP 6** → Repeat in 24 hrs * **BPP 8–10** → Continue routine follow-ups 6. Assess **AFI, Doppler, maternal condition** --- # **9️⃣ Important Clinical Correlations** ### **NST becomes abnormal earliest in fetal hypoxia** CNS activity reduces → loss of accelerations. ### **BPP components lost in sequence during hypoxia (Late → Early loss)** 1. **NST** 2. **Fetal breathing** 3. **Gross movement** 4. **Fetal tone** (last to disappear) 5. **AFI reduced** from chronic utero-placental insufficiency ### **AFI is chronic marker**; NST is acute marker. --- # ⭐ **HIGH-YIELD VALUES (MUST REVISE)** * Reactive NST: **≥2 accelerations** (15 × 15) * Tone: 1 flexion–extension * Breathing: ≥1 episode ≥30 sec * Movement: ≥3 body movements * AFI: Normal ≥5 cm * Modified BPP = NST + AFI * Sleep cycle: **20–40 min** → extend NST to 40 min --- --- # ⭐ **25 CASE SCENARIOS WITH DETAILED MANAGEMENT** *(Antepartum Fetal Surveillance: FMC, NST, BPP, VAST, mBPP)* --- # **1️⃣ Case Scenario – Decreased Fetal Movements at 34 Weeks** A 28-year-old G2P1 at 34 weeks reports **no fetal movements for 8 hours**. ### **Management** 1. Immediate **NST** 2. If **reactive** → reassure, daily kick count 3. If **non-reactive** → extend to 40 min 4. If still non-reactive → **VAST** 5. If remains non-reactive → **BPP** 6. * **BPP ≥8** → Follow-up * **BPP ≤4** → Deliver based on GA --- # **2️⃣ Case Scenario – Non-Reactive NST in a Diabetic Mother** GDM on insulin at 36 weeks undergoes NST → **non-reactive** after 40 minutes. ### **Management** 1. Perform **VAST** 2. If reactive → repeat NST in 1 week 3. If still non-reactive → **Full BPP** 4. If BPP score **≤4** → Plan delivery 5. Assess **AFI & Doppler** for placental insufficiency --- # **3️⃣ Case Scenario – Oligohydramnios with IUGR** 30-year-old at 32 weeks with **AFI = 4 cm**, EFW <10th percentile. ### **Management** 1. Start **modified BPP (NST + AFI)** 2. Daily NST 3. Doppler: **Umbilical artery S/D ratio** 4. If AEDF/REDF → **Immediate delivery** 5. If NST non-reactive → full BPP 6. Steroids if <34 weeks --- # **4️⃣ Case – Post-Dated Pregnancy (41 Weeks)** Patient at 41+2 weeks shows decreased fetal movement. ### **Management** 1. **NST + AFI** 2. If NST reactive & AFI normal → induce labour within 24–48 hrs 3. If NST non-reactive → BPP 4. BPP ≤6 → Deliver 5. Continuous intrapartum monitoring --- # **5️⃣ Case – Preeclampsia with Severe Features** 32 weeks, BP 160/110, proteinuria +++, fetus active. ### **Management** 1. Daily **NST** 2. Twice-weekly **BPP** 3. Doppler (UA + MCA) weekly 4. Magnesium sulfate for seizure prophylaxis 5. Deliver at 34 weeks or earlier if fetal compromise --- # **6️⃣ Case – Chronic Hypertension with Reduced Movements** 35-year-old with chronic HTN reports <4 kicks in 1 hr. ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. If AFI <5 → suspect placental insufficiency 4. Admit, daily surveillance 5. Deliver if BPP ≤4 or Doppler abnormal --- # **7️⃣ Case – IUGR with Normal NST** 29 weeks, IUGR but **reactive NST**. ### **Management** 1. Continue **twice-weekly NST** 2. Weekly Doppler (UA/ MCA/ CPR ratio) 3. Growth scan every 2 weeks 4. Deliver if Doppler deteriorates or NST becomes abnormal --- # **8️⃣ Case – Polyhydramnios with GDM** 30-year-old with polyhydramnios, NST reactive. ### **Management** 1. Twice-weekly NST 2. AFI monitoring 3. Doppler weekly 4. Induce at 38–39 weeks 5. Prepare for shoulder dystocia risk --- # **9️⃣ Case – Decreased Fetal Movement in Obese Mother** NST shows **baseline variability minimal**. ### **Management** 1. Rule out maternal meds, sleep cycle 2. Extend NST + VAST 3. If still abnormal → BPP 4. Deliver if BPP ≤4 --- # **🔟 Case – Rh-Isoimmunization** 28 weeks, MCA PSV >1.5 MOM (fetal anemia suspected). ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. Plan **intrauterine transfusion** 4. After IUT: Daily NST --- # **1️⃣1️⃣ Case – Twin Pregnancy with Growth Discordance** NST non-reactive for smaller twin. ### **Management** 1. VAST 2. If still non-reactive → BPP for each twin 3. Doppler UA/MCA/ Ductus venosus 4. Deliver if evidence of compromise --- # **1️⃣2️⃣ Case – Maternal Hypoglycemia Before NST** NST shows no accelerations. ### **Management** 1. Give oral glucose 2. Repeat NST 3. If becomes reactive → normal 4. If persistently non-reactive → VAST → BPP --- # **1️⃣3️⃣ Case – Placental Abruption Suspicion** Pain + bleeding + reduced movements. ### **Management** 1. **Immediate NST** 2. If late decelerations / bradycardia → **Immediate delivery** 3. Stabilize mother --- # **1️⃣4️⃣ Case – COVID Positive Mother with Decreased Movements** NST non-reactive. ### **Management** 1. Rule out maternal fever, hypoxia 2. Oxygen + hydration 3. VAST 4. If still non-reactive → BPP 5. Deliver if fetal compromise --- # **1️⃣5️⃣ Case – Smoking Mother with IUGR** NST shows decreased variability. ### **Management** 1. VAST 2. BPP 3. Doppler UA 4. Nicotine cessation + fetal surveillance every 2–3 days --- # **1️⃣6️⃣ Case – Absent Fetal Breathing on BPP** BPP = 6/10 (breathing absent). ### **Management** 1. Repeat BPP in 24 hrs 2. If repeat BPP ≤6 → Deliver 3. Continuous NST monitoring --- # **1️⃣7️⃣ Case – Low AFI but Reactive NST** AFI = 4 cm at 37 weeks. ### **Management** 1. Diagnose **oligohydramnios** 2. Admit, hydration 3. Modified BPP daily 4. Deliver at 37–38 weeks --- # **1️⃣8️⃣ Case – Maternal Seizure on MgSO₄** NST shows minimal variability (drug effect). ### **Management** 1. Continue monitoring 2. Do not interpret variability during MgSO₄ therapy 3. Use **BPP** instead of NST --- # **1️⃣9️⃣ Case – Poorly Controlled Diabetes** 36 weeks, polyhydramnios + macrosomia. ### **Management** 1. NST every 2–3 days 2. Weekly BPP 3. Deliver at 38 weeks 4. Prepare for shoulder dystocia --- # **2️⃣0️⃣ Case – Maternal Dehydration** NST non-reactive. ### **Management** 1. Give IV fluids 2. Repeat NST 3. If reactive → dehydration cause 4. If persists → BPP --- # **2️⃣1️⃣ Case – Postpartum Hemorrhage Risk Mother** Placenta previa major. ### **Management** 1. Weekly NST 2. BPP if NST abnormal 3. Plan elective C-section at 36–37 weeks --- # **2️⃣2️⃣ Case – Fetal Tachycardia** FHR 170 bpm in NST. ### **Management** 1. Exclude maternal fever, dehydration, drugs 2. Treat maternal cause 3. If persists → BPP + Doppler 4. Consider delivery if fetal compromise --- # **2️⃣3️⃣ Case – Mother on Sedatives** NST non-reactive. ### **Management** 1. Document medication effect 2. Perform BPP instead of repeating NST 3. Reassure if BPP normal --- # **2️⃣4️⃣ Case – Sudden IUD Suspicion** No FHR detected in NST. ### **Management** 1. Confirm with ultrasound 2. Evaluate cause (abruption, cord accident) 3. Manage according to GA and maternal stability --- # **2️⃣5️⃣ Case – Preterm (<32 Weeks) Non-Reactive NST** At 30 weeks, NST non-reactive. ### **Management** 1. Extend NST to 40 min 2. Apply VAST 3. If still non-reactive → BPP 4. If BPP ≤4 → Deliver after steroid cover 5. If BPP normal → prematurity likely cause ---
Intrapartum Fetal Monitoring: CTG Interpretation, Decelerations, Sinusoidal Pattern & Complete Management Guide 2025
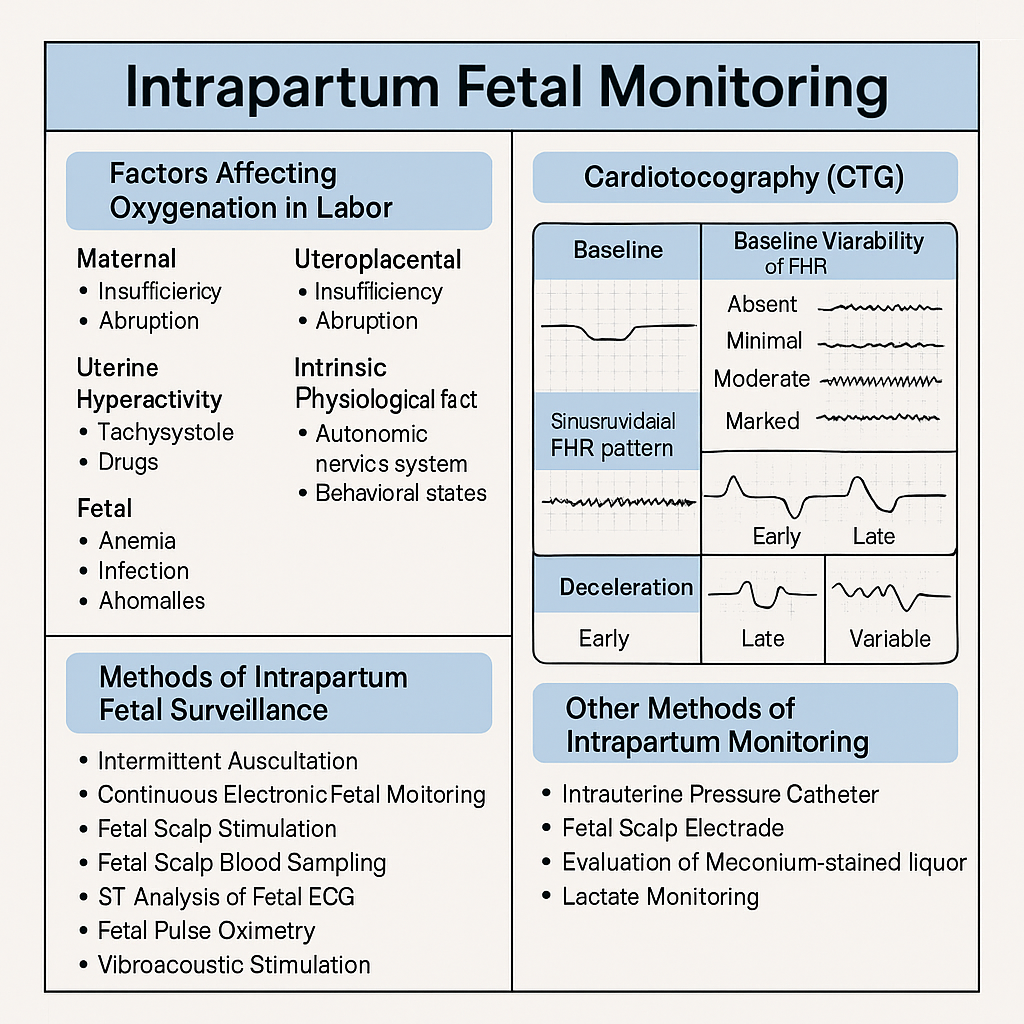
Below are **30 detailed intrapartum fetal monitoring case scenarios with complete management**, written in **NEET PG / INI-CET exam style**. Each scenario includes **clinical context → CTG finding → diagnosis → step-wise management**. --- # ✅ **30 CASE SCENARIOS WITH DETAILED MANAGEMENT (Intrapartum Fetal Monitoring)** --- ## **1️⃣ Case — Late Decelerations in a Preeclamptic Mother** A 25-year-old primigravida, 4 cm dilated, on oxytocin. CTG shows **recurrent late decelerations**, baseline 150, variability <5 bpm. ### **Diagnosis** Uteroplacental insufficiency from **preeclampsia + hyperstimulation**. ### **Management** 1. Stop oxytocin 2. Left lateral position 3. IV fluids 4. If contraction frequency >5/10 min → **tocolysis (terbutaline 0.25 mg SC)** 5. If no improvement → **FBS** 6. If pH <7.20 or tracing deteriorates → **Emergency LSCS** --- ## **2️⃣ Case — Variable Decelerations with Oligohydramnios** G2P1, term labor, CTG shows **variable decelerations with shoulders**, adequate variability. ### **Diagnosis** Cord compression due to oligohydramnios. ### **Management** 1. Maternal repositioning 2. Amnioinfusion 3. Continue labor if variability normal 4. If severe recurrent variables + loss of variability → expedite delivery --- ## **3️⃣ Case — Sinusoidal Pattern** Rh-negative woman, fetus 38 weeks. CTG: **true sinusoidal pattern**. ### **Diagnosis** Severe fetal anemia. ### **Management** 1. Immediate evaluation (Kleihauer test, ultrasound MCA Doppler if time permits) 2. **Emergency LSCS** 3. Prepare NICU for transfusion --- ## **4️⃣ Case — Prolonged Deceleration from Cord Prolapse** During vaginal exam, a loop of cord felt. CTG shows **bradycardia at 80 bpm** for 4 minutes. ### **Management** 1. Lift presenting part manually 2. Knee–chest position 3. Call for emergency LSCS 4. Warm sterile saline-soaked gauze to prevent vasospasm 5. Deliver within **<30 minutes** --- ## **5️⃣ Case — Tachysystole-Induced Late Decelerations** Oxytocin infusion running, contractions 6/10 min. CTG: recurrent late decels. ### **Management** 1. Stop oxytocin immediately 2. Terbutaline 0.25 mg SC 3. Lateral position 4. Reassess 5. If persists → expedite delivery --- ## **6️⃣ Case — Minimal Variability for 50 Minutes** Primigravida in active labor. CTG: baseline 140, variability <5 bpm for 50 min, no decels. ### **Diagnosis** Non-reassuring CTG, possibly fetal sleep or medication effect. ### **Management** 1. Scalp stimulation 2. If acceleration present → reassuring 3. If absent → FBS or continuous monitoring 4. Continue labor if other parameters normal --- ## **7️⃣ Case — Meconium-Stained Liquor with Abnormal CTG** Thick meconium + variable decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. Amnioinfusion (if available) 3. Prepare for operative delivery 4. NICU standby for Meconium Aspiration Syndrome --- ## **8️⃣ Case — Prolonged Deceleration After Epidural** Immediately after epidural, FHR drops to 90 bpm for 3 minutes. ### **Diagnosis** Maternal hypotension causing decreased uteroplacental flow. ### **Management** 1. Left lateral position 2. IV fluid bolus 3. Vasopressor (phenylephrine preferred) 4. If persists beyond 5 minutes → consider LSCS --- ## **9️⃣ Case — Fetal Tachycardia with Maternal Fever** CTG shows FHR 180 bpm, moderate variability; maternal temp 101°F. ### **Diagnosis** Chorioamnionitis. ### **Management** 1. Broad-spectrum antibiotics 2. Acetaminophen 3. Expedite delivery (not LSCS solely for fever) 4. Avoid prolonged labor --- ## **🔟 Case — Arrest of Descent + Late Decelerations** Second stage, fully dilated, prolonged pushing, late decels appear. ### **Management** 1. Check for instrumental eligibility 2. **Forceps or vacuum** if head low 3. If not eligible → emergency LSCS --- ## **1️⃣1️⃣ Case — Recurrent Severe Variable Decelerations** CTG: variable decels dropping to 70 bpm for 60–90 sec. ### **Management** 1. Lateral positioning 2. Amnioinfusion 3. Reduce contractions if tachysystole 4. If persistent → operative delivery --- ## **1️⃣2️⃣ Case — Fetal Scalp pH Borderline** FBS pH = 7.22. ### **Management** 1. Correct reversible causes 2. Repeat FBS in 30 min 3. If worsens → expedite delivery --- ## **1️⃣3️⃣ Case — Loss of Variability with Bradycardia** Baseline 90 bpm, absent variability. ### **Diagnosis** Advanced fetal hypoxia. ### **Management** 1. Immediate decision for LSCS 2. No role of waiting or FBS --- ## **1️⃣4️⃣ Case — CTG Unable to Trace Due to Obesity** During labor, external CTG poor quality. ### **Management** 1. Switch to **fetal scalp electrode (FSE)** 2. Use IUPC for contraction monitoring 3. Continue labor normally if FHR normal --- ## **1️⃣5️⃣ Case — Category III CTG in Trial of Labor After Cesarean (TOLAC)** Late decels + minimal variability + scar tenderness. ### **Diagnosis** Scar rupture suspected. ### **Management** 1. Immediate emergency LSCS 2. Do NOT attempt instrumental delivery --- ## **1️⃣6️⃣ Case — Hyperstimulation Causing Decelerations** Misoprostol induction; CTG shows tachysystole + decels. ### **Management** 1. Stop prostaglandin 2. Tocolysis 3. Continuous monitoring 4. If fetal distress → emergency delivery --- ## **1️⃣7️⃣ Case — True Sinusoidal Pattern from Fetomaternal Hemorrhage** CTG sinusoidal; Kleihauer test positive. ### **Management** 1. Emergency delivery 2. Neonatal transfusion preparation --- ## **1️⃣8️⃣ Case — Prolonged Decel During Second Stage** Mother pushing vigorously; CTG shows bradycardia. ### **Management** 1. Stop pushing 2. Reassess for instrument delivery 3. If head + station → vacuum/forceps 4. Otherwise → LSCS --- ## **1️⃣9️⃣ Case — Mild Variable Decelerations with Normal Variability** Intermittent variables, contraction-associated. ### **Management** 1. Reassurance 2. Continue monitoring No intervention required. --- ## **2️⃣0️⃣ Case — Shoulder Dystocia + Bradycardia** Delivery nearly complete, FHR falls to 70 bpm. ### **Management** 1. McRoberts + suprapubic pressure 2. Deliver shoulders quickly 3. Neonatal resuscitation readiness --- ## **2️⃣1️⃣ Case — Cord Around Neck Detected on Ultrasound Before Labor** During labor → variable decels appear. ### **Management** 1. Continue monitoring 2. If severe or persistent → expedite delivery 3. Do not intervene solely for nuchal cord --- ## **2️⃣2️⃣ Case — Prolapsed Cord in Breech** CTG severe bradycardia. ### **Management** 1. Knee–chest position 2. Manual elevation of presenting part 3. Emergency LSCS --- ## **2️⃣3️⃣ Case — Minimal Variability from Opioid Analgesia** Given pethidine 15 min ago; variability <5. ### **Management** 1. Observe for 30–60 min 2. If variability recovers → continue 3. If not → evaluate for fetal hypoxia --- ## **2️⃣4️⃣ Case — Reassuring CTG in Low-Risk Labor** Baseline 140, variability 10, accelerations present. ### **Management** Continue routine monitoring. --- ## **2️⃣5️⃣ Case — Excessive Maternal Dehydration** CTG shows fetal tachycardia 170 bpm. ### **Management** 1. IV fluid bolus 2. Assess maternal vitals 3. Continue monitoring --- ## **2️⃣6️⃣ Case — Placental Abruption Suspected** Pain + bleeding + fetal tachycardia → later bradycardia. ### **Management** 1. Stabilize mother 2. Immediate LSCS if fetus alive 3. Vaginal delivery only if imminent --- ## **2️⃣7️⃣ Case — IUGR Baby with Recurrent Late Decelerations** CTG: late decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. No role for prolonged labor 3. **Expedite delivery** --- ## **2️⃣8️⃣ Case — Maternal Seizure (Eclampsia)** CTG: prolonged decel. ### **Management** 1. Stabilize mother (MgSO₄, airway) 2. Left lateral position 3. If fetal recovery absent → LSCS --- ## **2️⃣9️⃣ Case — Vaginal Birth After Multiple Variables** CTG mostly reassuring except mild variables. ### **Management** 1. Continue monitoring 2. Check for cord issues 3. No intervention unless severe --- ## **3️⃣0️⃣ Case — Failure of Fetal Response to Scalp Stimulation** Minimal variability, no acceleration after stimulation. ### **Diagnosis** Hypoxia suspected. ### **Management** 1. FBS if available 2. If pH abnormal → immediate delivery 3. If not available → treat as pathological CTG → expedite delivery --- If you want, I can also produce: ✅ **HTML + CSS + JS EXAM MODE MCQs (25/30/50)** ✅ **SEO title/description/keywords** ✅ **A medical diagram image for intrapartum fetal monitoring** Just say **“generate MCQs”**, **“generate image”**, or **“give SEO”**. Below is your **complete, concise-but-exhaustive master reference** on **Intrapartum Fetal Monitoring** — fully aligned with NEET PG / INI-CET high-yield requirements. --- # ⭐ **INTRAPARTUM FETAL MONITORING — COMPLETE DETAILED NOTES (2025)** --- ## **1️⃣ Factors Affecting Fetal Oxygenation During Labor** Fetal oxygenation depends on uninterrupted flow across **four levels**: ### **A. Maternal Factors** * **Maternal oxygenation:** Hypoxia, severe anemia, pulmonary disease. * **Uterine perfusion:** Hypotension (epidural, hemorrhage), dehydration, aortocaval compression. * **Uterine hyperactivity:** Tachysystole (>5 contractions/10 min), hypertonus ↓ intervillous blood flow. * **Drugs:** β-agonists ↑ fetal tachycardia; opioids ↓ variability. ### **B. Uteroplacental Factors** * Placental insufficiency (hypertension, preeclampsia, post-maturity). * Placental abruption, infarction, previa, accreta spectrum. * Umbilical cord compression (oligohydramnios, cord prolapse, tight nuchal cord). ### **C. Fetal Factors** * Fetal anemia, infections, acidosis. * Congenital anomalies (especially CNS, cardiac). * Prematurity → reduced variability. ### **D. Intrinsic Physiological Factors** * Autonomic nervous system balance (sympathetic/parasympathetic). * Fetal behavioral states (quiet sleep cycles ↓ variability). --- ## **2️⃣ Methods of Intrapartum Fetal Surveillance** ### **A. Intermittent Auscultation (IA)** * Using **Pinard stethoscope** or **Doppler**. * Low-risk pregnancies. * Frequency: * **1st stage:** every 30 min * **2nd stage:** every 5 min * Look for: baseline, accelerations, decelerations. ### **B. Continuous Electronic Fetal Monitoring (EFM / CTG)** * External US transducer + tocodynamometer. * Internal scaling: scalp electrode + IUPC (intrauterine pressure catheter) when needed. ### **C. Fetal Scalp Stimulation** * Acceleration after stimulation → reassuring (pH > 7.2). ### **D. Fetal Scalp Blood Sampling (FBS)** → Direct measure of fetal acid-base status. * **Normal pH ≥ 7.25** * **Borderline 7.21–7.24** * **Abnormal < 7.20** → urgent delivery. ### **E. ST-Analysis of Fetal ECG (STAN)** * Detects myocardial hypoxia (ST changes). * Used with CTG. ### **F. Fetal Pulse Oximetry (rare)** * Reassurance if SpO₂ > 30%. ### **G. Vibroacoustic Stimulation** * Sound stimulus → acceleration = good oxygenation. --- ## **3️⃣ Cardiotocography (CTG) – Complete Interpretation** CTG has **5 components**: **Baseline, Variability, Accelerations, Decelerations, Contractions.** --- ## **3.1 Baseline Fetal Heart Rate** Normal: **110–160 bpm** ### **Tachycardia (>160 bpm) causes:** * Maternal fever (chorioamnionitis) * Fetal hypoxia early * Fetal anemia * Drugs: β-agonists, atropine ### **Bradycardia (<110 bpm) causes:** * Vagal stimulation (head compression) * Cord compression * Prolonged deceleration → late sign of hypoxia --- ## **3.2 Baseline Variability (BV)** Reflects fetal autonomic integrity. | **Type** | **Range** | **Significance** | | --------------------- | ------------ | ------------------------------------------ | | Absent | 0 bpm | Severe hypoxia, acidosis, drugs | | Minimal | <5 bpm | Sleep cycle, opioids, prematurity, hypoxia | | **Moderate (Normal)** | **6–25 bpm** | Good oxygenation | | Marked | >25 bpm | Early hypoxia, cord compression | --- ## **3.3 Accelerations** * Abrupt ↑ in FHR by ≥15 bpm for ≥15 sec. * **Reassuring sign** → fetal well-being. --- ## **3.4 Decelerations — Types & Complete Interpretation** ### **A. Early Decelerations** * Mirror contractions. * Due to **head compression**. * **Benign, no treatment.** ### **B. Late Decelerations** * Begin after the contraction peak → return after contraction ends. * Due to **uteroplacental insufficiency**. * **Always concerning**, esp. with absent variability. ### **C. Variable Decelerations** * Abrupt fall in FHR, variable shape. * Due to **cord compression**. * May have "shoulders" (pre- & post-acceleration). * Severe if >60 bpm drop lasting >60 sec. ### **D. Prolonged Deceleration** * FHR drop ≥15 bpm lasting **2–10 min**. * > 10 min = change in baseline. ### **E. Sinusoidal Pattern (MOST IMPORTANT)** **True Sinusoidal Pattern** * Smooth, regular, sine-wave oscillation (3–5 cycles/min) * Amplitude 5–15 bpm * No variability, no accelerations * **Causes:** * Severe fetal anemia (Rh isoimmunization, fetomaternal hemorrhage) * Twin-to-twin transfusion * Hypoxia late stage * **Immediate delivery required** **Pseudo-sinusoidal:** * Seen with opioids — benign. --- ## **4️⃣ NICE 2024 Categories of CTG Interpretation** | Category | Findings | Action | | ------------------------------- | -------------------------------------------------------- | ------------------------------------------------ | | **Normal (Category I)** | Baseline 110–160, Variability 6–25, No repetitive decels | Continue | | **Suspicious (Category II)** | One non-reassuring feature | Correct reversible causes, close monitoring | | **Pathological (Category III)** | ≥1 abnormal feature OR ≥2 non-reassuring | Immediate evaluation, FBS, or expedited delivery | ### **Features** **Reassuring:** * Baseline 110–160 * Variability 6–25 * No decelerations / early decels * Accelerations present **Non-reassuring:** * Baseline 100–109 or 161–180 * Variability <5 for 40–90 min * Variable decels with features * Single prolonged decel <3 min **Abnormal:** * Baseline <100 or >180 * Variability <5 for >90 min * Late decels / prolonged decels >3 min * Sinusoidal pattern --- ## **5️⃣ Management of Abnormal CTG** ### **A. Correct Reversible Causes** * Left lateral position * IV fluids → treat maternal hypotension * Stop oxytocin (if tachysystole) * Tocolysis if uterine hyperstimulation (Terbutaline 0.25 mg SC) * Oxygen (only if maternal hypoxia) ### **B. Fetal Assessment** * Fetal scalp stimulation * FBS (pH or lactate) ### **C. Delivery** * If pH <7.20 OR pathological CTG persists * Emergency LSCS or instrumental delivery depending on stage --- ## **6️⃣ Other Methods of Intrapartum Monitoring** ### **A. Intrauterine Pressure Catheter (IUPC)** * Measures **Montevideo units** * Adequate labor: **>200 MVU** ### **B. Fetal Scalp Electrode (FSE)** * Accurate beat-to-beat FHR * Used when external CTG is poor. ### **C. Meconium-stained liquor evaluation** * Thick meconium + abnormal CTG → intrapartum hypoxia risk. ### **D. Lactate Monitoring** * Fetal scalp lactate <4.8 mmol/L reassuring. --- ## **7️⃣ Quick High-Yield Revision Table** | Topic | Key Points | | ------------------------------- | ------------------------------- | | Best indicator of fetal hypoxia | **Reduced variability** | | Worst CTG sign | **Sinusoidal pattern** | | Earliest sign of hypoxia | **Tachycardia** | | Most common deceleration | **Variable (cord compression)** | --- If you want, I can also generate: ✅ SEO title, description & keywords ✅ 25 hard case-based MCQs (HTML + CSS + JS EXAM MODE) ✅ 25 case scenarios with management ✅ Medical diagram image (via image generator) Just tell me **“continue”** with what you need.
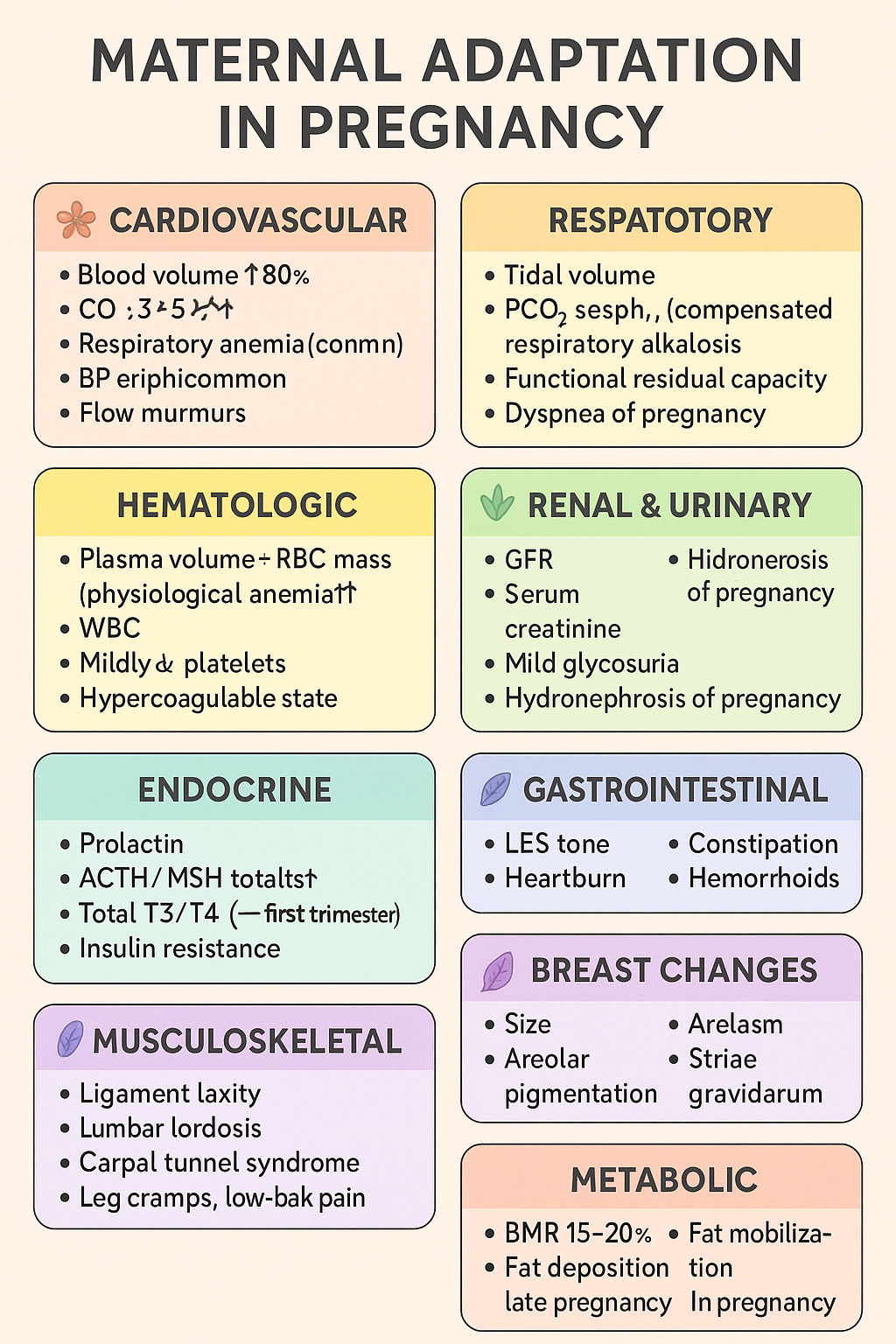
Maternal Adaptations in Pregnancy: Cardiovascular, Respiratory, Renal, Endocrine & Hematologic Changes | Complete Obstetrics Guide 2025
Below is your **complete, crisp but exhaustive stylish note** on **MATERNAL ADAPTATION IN PREGNANCY** — perfect for **NEET PG / INI-CET** and LWT article publishing. Presented in **high-yield, section-boxed format**. --- # ⭐ **MATERNAL ADAPTATIONS IN PREGNANCY — COMPLETE STYLISH NOTE (2025)** Pregnancy induces **multi-system physiologic adaptations** to support fetal growth, prepare for labor, and protect the mother from hemodynamic stresses. --- ## 🌸 **1. Cardiovascular Adaptations** ### 🔹 *Changes* * **Blood volume ↑ 40–50%** (plasma ↑ > RBC mass ↑ → *physiological anemia*). * **CO ↑ 30–50%** → peaks at 20–24 weeks. * **HR ↑ 10–20 bpm**. * **Systemic vascular resistance ↓** (progesterone-mediated vasodilation). * **BP ↓ in 2nd trimester**, returns to baseline in 3rd. * **Peripheral edema common** due to venous compression by gravid uterus. * **Flow murmurs, S3 may appear**. ### 🔹 *Clinical significance* * ↑ preload → protects from blood loss during delivery. * Supine position → **supine hypotension syndrome** (IVC compression). * Murmurs usually benign; still evaluate if symptomatic. --- ## 🌸 **2. Respiratory Adaptations** ### 🔹 *Changes* * **Tidal volume ↑ 30–40%**, minute ventilation ↑. * **PCO₂ ↓ → respiratory alkalosis (compensated)**. * **Functional residual capacity ↓** (diaphragm elevation by 4 cm). * **Dyspnea of pregnancy common** (physiological). ### 🔹 *Clinical significance* * Low PCO₂ → facilitates **placental CO₂ transfer**. * Increased ventilation → improved oxygenation for fetus. --- ## 🌸 **3. Hematologic Adaptations** ### 🔹 *Changes* * **Plasma volume ↑ 50%**, **RBC mass ↑ 20–30%** → dilution → **Hb ↓ (physiologic anemia)**. * **WBC ↑** (can reach 12–16k). * **Platelets mildly ↓** (gestational thrombocytopenia). * **Hypercoagulable state** → fibrinogen ↑, clotting factors ↑. ### 🔹 *Clinical significance* * Protects from postpartum hemorrhage. * ↑ VTE risk — especially postpartum. --- ## 🌸 **4. Renal & Urinary Adaptations** ### 🔹 *Changes* * **GFR ↑ 40–50%** (starts early). * **Serum creatinine ↓ 0.4–0.6 mg/dL**. * **Mild glycosuria** common. * **Hydronephrosis of pregnancy** (right > left) due to progesterone + uterine compression. ### 🔹 *Clinical significance* * Minor proteinuria acceptable (<300 mg/day). * Avoid misinterpreting physiologic glycosuria as diabetes. --- ## 🌸 **5. Endocrine Adaptations** ### 🔹 *Pituitary* * **Prolactin ↑** 10-fold → lactation prep. * **ACTH & MSH ↑** → pigmentation changes. ### 🔹 *Thyroid* * **Estrogen ↑ TBG**, total T3/T4 ↑; **free T4 normal**. * **hCG weak TSH activity → TSH ↓** (first trimester). ### 🔹 *Pancreas* * Early pregnancy: **insulin sensitivity ↑**. * Late pregnancy: **insulin resistance ↑** (placental hormones: hPL, cortisol) → predisposes to **GDM**. --- ## 🌸 **6. Gastrointestinal Adaptations** ### 🔹 *Changes* * **Progesterone ↓ LES tone** → heartburn. * **Gastric emptying ↓** → nausea/vomiting. * **Constipation** from prolonged transit time. * **Hemorrhoids** due to venous congestion. ### 🔹 *Clinical significance* * Morning sickness peaks at 9–10 weeks. * Hyperemesis gravidarum requires electrolyte correction. --- ## 🌸 **7. Musculoskeletal Adaptations** ### 🔹 *Changes* * **Relaxin + progesterone → ligament laxity**. * **Lumbar lordosis ↑** due to uterine weight. * **Carpal tunnel syndrome** possible. * **Leg cramps**, **low-back pain** common. ### 🔹 *Clinical significance* * Risk of falls increases. * Proper posture + exercises advised. --- ## 🌸 **8. Breast Changes** * **Size ↑**, ducts proliferate. * **Areolar pigmentation**, Montgomery tubercles prominent. * **Colostrum secretion** by late pregnancy. --- ## 🌸 **9. Dermatologic Adaptations** * **Linea nigra**, **melasma**, **striae gravidarum**. * **Spider angiomas**, palmar erythema (estrogen related). --- ## 🌸 **10. Metabolic Adaptations** * **Basal metabolic rate ↑ 15–20%**. * **Fat deposition ↑** early pregnancy. * Late pregnancy: catabolic → **fat mobilization** for maternal energy, glucose spared for fetus. --- # ⭐ **ULTRA-SHORT MEMORY HACK TABLE** | System | Key Adaptation | Why it Happens | | --------------- | ---------------------- | ---------------------------------------------------- | | CVS | CO ↑ 50%, plasma ↑ 50% | To meet fetal perfusion & buffer delivery blood loss | | Respiratory | TV ↑, PCO₂ ↓ | Better fetal CO₂ removal | | Renal | GFR ↑ 50% | Remove maternal/fetal waste | | Hematologic | Hypercoagulable | Prevent PPH | | Endocrine | Insulin resistance | Ensure fetal glucose | | GI | ↓ Motility | Progesterone effect | | Musculoskeletal | Ligament laxity | Prepare pelvis for birth | --- If you want, I can generate: ✅ **HTML-CSS-JS formatted article** (like your LWT posts) ✅ **MCQs (20/25/30 hard case-based)** ✅ **SEO title + description + keywords** ✅ **Custom medical diagram for maternal adaptations** Just tell me **which output you want next**.
Complete guide on anaemia in pregnancy including causes, WHO definition, diagnosis, iron requirements, IFA tablets, NIAP, Anemia Mukt Bharat, treatment & management.
Great — I made **30 concise, high-yield case scenarios** on anaemia in pregnancy. Each case includes: brief history/exam, key labs, working diagnosis, immediate management, definitive treatment plan, and follow-up. I kept dosing and practical steps clear so you can paste these into teaching slides, case banks or clinical notes. --- # 30 Case Scenarios — Anaemia in Pregnancy (with management) > Legend: FS 325 mg ≈ 65 mg elemental Fe; typical oral treatment: **60–120 mg elemental Fe/day** (commonly 1 FS 325 mg once–three times daily depending on severity/tolerance). IV iron options: **iron sucrose** (commonly 100–200 mg per infusion repeated to calculated total) or **ferric carboxymaltose (FCM)** (single doses up to 750–1000 mg per product guidance). Transfusion generally considered for **Hb ≤7.0 g/dL** or symptomatic/hemodynamically unstable patient; tailor to obstetric context. --- ### Case 1 — Mild IDA, first trimester * Presentation: 24 y, G1P0, 10 wks, fatigue. Exam: pallor only. * Labs: Hb 10.2 g/dL, MCV 74 fL, ferritin 8 ng/mL, Mentzer >13. Smear: microcytic hypochromic. * Dx: Iron deficiency anaemia (mild). * Immediate mgmt: Start oral iron — **FS 325 mg once daily** (≈65 mg elemental) + folic acid 400 µg; counsel on absorption and side effects. * Definitive plan: Check Hb at 4 weeks; if Hb rising by ~1 g/dL, continue 3 months after normalization to replete stores. Diet & deworm if indicated. --- ### Case 2 — Moderate IDA, second trimester, poor diet * Presentation: 29 y, 20 wks, progressive exertional dyspnea. * Labs: Hb 8.3 g/dL, MCV 68 fL, ferritin 9 ng/mL. * Dx: Moderate IDA. * Immediate mgmt: Oral iron **FS 325 mg twice daily** (≈130 mg elemental/day) + folic acid; start vitamin C with dose. Consider adherence issues. * Definitive plan: Reassess Hb in 2–3 weeks. If poor response or intolerance → switch to IV iron (calculate total deficit; consider FCM 1000 mg single or iron sucrose series). --- ### Case 3 — Severe symptomatic anaemia late pregnancy * Presentation: 31 y, 36 wks, chest tightness, syncope history. Exam: tachycardia, low BP. * Labs: Hb 5.8 g/dL, MCV 75 fL, ferritin 5 ng/mL. * Dx: Severe IDA with hemodynamic compromise. * Immediate mgmt: Resuscitate (IV fluids as needed), **blood transfusion** (matched PRBCs) — aim to stabilise; crossmatch and transfuse per obstetric transfusion protocol. * Definitive plan: After stabilization, give IV iron (iron sucrose/FCM) to replete stores; counsel for delivery planning and postpartum follow-up. --- ### Case 4 — Late presentation, intolerance to oral iron * Presentation: 26 y, 34 wks, vomiting with oral iron causing severe nausea. * Labs: Hb 9.0 g/dL, ferritin 10 ng/mL. * Dx: IDA with oral intolerance. * Immediate mgmt: Stop oral iron; offer **IV iron** (iron sucrose series or FCM depending on availability) to correct quickly pre-delivery. Monitor vitals during infusion. * Follow-up: Hb/ferritin 2–4 weeks post-infusion; resume oral prophylaxis postpartum. --- ### Case 5 — Refractory anaemia despite oral iron * Presentation: 28 y, 22 wks, on FS 325 mg TID x 6 weeks, minimal Hb rise. * Labs: Hb 9.2 g/dL, ferritin 6 ng/mL, reticulocyte low-normal. * Dx: Non-response to oral iron (malabsorption, non-adherence, ongoing loss). * Immediate mgmt: Evaluate adherence, check for parasites/GI blood loss. If adherence OK → **IV iron**. Consider stool testing for hookworm. Screen for celiac if suspicion. * Definitive plan: Treat underlying cause; calculate iron deficit and give IV iron. --- ### Case 6 — Microcytosis suspicious for thalassaemia trait * Presentation: 21 y, 12 wks, mild pallor. Labs: Hb 10.8 g/dL, MCV 65 fL, RBC count high, Mentzer <13, ferritin normal 50 ng/mL. * Dx: Likely β-thalassaemia trait. * Mgmt: Confirm with **Hb electrophoresis (elevated HbA₂)**. Do **not** give high-dose iron if ferritin normal. Genetic counselling and partner screening. Provide routine antenatal care; avoid unnecessary iron. --- ### Case 7 — Anaemia of chronic disease (ACD) * Presentation: 34 y, known lupus, 28 wks, fatigue. Labs: Hb 9.6 g/dL, ferritin 180 ng/mL, low serum iron, low TIBC. CRP high. * Dx: ACD due to chronic inflammation. * Mgmt: Treat underlying disease flare; iron supplementation only if true iron deficiency coexists (assess transferrin saturation). Consider erythropoiesis-stimulating agents only in specialist settings; consult rheumatology/hematology. --- ### Case 8 — Folate deficiency plus iron deficiency * Presentation: 30 y, 18 wks, glossitis, neural tube risk concern. Labs: Hb 9.4 g/dL, MCV 102 fL, low folate. Smear: macro-ovalocytes. Ferritin low-normal. * Dx: Mixed folate deficiency ± iron deficiency. * Mgmt: Start **folic acid 5 mg daily** (treatment dose) + oral iron (if ferritin low). Investigate diet, malabsorption. Reassess CBC after 2–4 weeks. --- ### Case 9 — B12 deficiency in pregnancy * Presentation: 27 y, 24 wks, paresthesia, macrocytic indices. Labs: Hb 8.9 g/dL, MCV 108 fL, low B12. * Dx: B12 deficiency. * Mgmt: **IM/SC cyanocobalamin** replacement (e.g., 1000 µg IM weekly × several doses then monthly) depending on cause; treat concurrently with folate if needed. Neurologic signs may take months to improve. --- ### Case 10 — Postpartum haemorrhage with acute blood loss * Presentation: 35 y, day 1 postpartum after PPH, tachycardic, Hb 6.1 g/dL. * Dx: Acute severe anaemia from blood loss. * Mgmt: Immediate resuscitation; **urgent transfusion** (PRBCs), manage bleeding source (surgical/medical). After stabilization consider IV iron for repletion. --- ### Case 11 — Twin pregnancy with increased iron need * Presentation: 32 y, twin gestation 28 wks, fatigue. Labs: Hb 9.0 g/dL, ferritin 12 ng/mL. * Dx: IDA in multiple pregnancy. * Mgmt: Start **oral iron** at treatment dose (FS 325 mg twice daily) and consider early IV iron if inadequate response or near-term to optimize Hb before delivery. Close monitoring. --- ### Case 12 — Hyperemesis gravidarum causing iron deficiency * Presentation: 22 y, 10 wks, severe vomiting; poor intake. Labs: Hb 9.8 g/dL, ferritin 15 ng/mL. * Dx: IDA from poor intake. * Mgmt: Correct dehydration, antiemetics + start **oral iron** when tolerated (consider IV iron if vomiting prevents oral intake). Nutritional support and folate. --- ### Case 13 — Hookworm infection causing chronic blood loss * Presentation: 25 y, 26 wks, pica, eosinophilia. Labs: Hb 8.7 g/dL, ferritin 7 ng/mL. Stool: ova consistent with hookworm. * Dx: IDA due to helminthiasis. * Mgmt: Treat hookworm per local protocol (deworming timing per antenatal policy; e.g., single-dose albendazole often after first trimester in many settings), start oral iron or IV iron if severe; public-health measures. --- ### Case 14 — Malaria-associated anaemia in pregnancy * Presentation: 28 y, febrile 30 wks, pallor, splenomegaly. Labs: Hb 7.9 g/dL, smear positive for Plasmodium. * Dx: Malaria-related anaemia. * Mgmt: Treat malaria urgently with pregnancy-safe antimalarial per local guideline; transfuse if severe/symptomatic; start iron only after clearing infection and per clinician judgment. --- ### Case 15 — HIV with anaemia of multifactorial cause * Presentation: 29 y, known HIV on ART, 20 wks, fatigue. Labs: Hb 9.0 g/dL, ferritin 90 ng/mL, MCV variable. * Dx: Multifactorial (ACD, drug-related, nutritional). * Mgmt: Review ART (e.g., zidovudine can cause anaemia), treat nutritional deficiencies, consider IV iron if IDA confirmed and oral therapy fails; coordinate with HIV care. --- ### Case 16 — Renal disease with anemia in pregnancy * Presentation: 36 y, CKD stage 3, 24 wks, low energy. Labs: Hb 8.6 g/dL, ferritin 150 ng/mL, low reticulocyte. * Dx: Anaemia of CKD/ACD. * Mgmt: Nephrology consult; consider IV iron if iron-deficient; consider erythropoiesis stimulating agents in specialist setting; optimise dialysis/renal care. --- ### Case 17 — Recurrent anemia after oral iron completion * Presentation: 27 y, previously treated IDA, returns 3 months postpartum with Hb 9.5 g/dL. Ferritin low 12 ng/mL. * Dx: Recurrent iron deficiency. * Mgmt: Reassess for ongoing bleeding; restart iron therapy; investigate heavy menstrual bleeding; counsel on compliance and diet; consider long-term iron strategy until cause fixed. --- ### Case 18 — Anaemia with allergic reaction to IV iron history * Presentation: 30 y, history of anaphylaxis to IV iron dextran. Now 30 wks, Hb 7.5 g/dL. * Dx: Severe IDA with prior IV iron allergy. * Mgmt: Avoid offending agent; use non-dextran formulations (iron sucrose or FCM) under monitored conditions with resuscitation available; consider transfusion if urgent and risk high. --- ### Case 19 — Mixed thalassaemia trait + iron deficiency * Presentation: 23 y, MCV 68 fL, Mentzer borderline, ferritin low 10 ng/mL. * Dx: Mixed iron deficiency + thalassaemia trait. * Mgmt: Treat iron deficiency (oral/IV as needed) — correct iron first and reassess indices; refer to hematology/genetic counselling for thalassaemia. --- ### Case 20 — Severe anaemia with cardiac compromise * Presentation: 38 y, 34 wks, signs of high-output cardiac failure (orthopnea), Hb 6.5 g/dL. * Dx: Severe anaemia causing cardiac strain. * Mgmt: Urgent transfusion and cardiac support; plan delivery in appropriate setting once stabilized; consider IV iron after haemodynamic stability. --- ### Case 21 — Antenatal screening finds microcytic anaemia in partner/partner screening scenario * Presentation: 26 y, first visit, Hb 11.1 g/dL but MCV 72 fL. Ferritin 40 ng/mL. RBC count high. Mentor index <13. * Dx: Possible thalassaemia trait carrier. * Mgmt: Do Hb electrophoresis; if positive, offer partner testing and genetic counselling; avoid unnecessary iron if iron stores adequate. --- ### Case 22 — Severe anaemia in adolescent pregnant patient * Presentation: 17 y, 18 wks, symptomatic, Hb 7.2 g/dL. * Dx: Severe IDA. * Mgmt: Consider transfusion if symptomatic; otherwise start IV iron if available; add nutritional counselling, address social determinants (poverty/diet), involve adolescent health services. --- ### Case 23 — Anaemia discovered during labour * Presentation: 30 y, in labor, known Hb 8.0 g/dL on admission. * Dx: Moderate IDA at delivery. * Mgmt: Plan for blood availability if bleeding risk high; give IV iron postpartum if Hb fails to improve and prolonged recovery expected; active management of third stage of labour to avoid PPH. --- ### Case 24 — Severe IDA with late booking and need for rapid correction before c-section * Presentation: 33 y, booked at 38 wks, Hb 8.0 g/dL, scheduled c-section next week. * Dx: IDA needing rapid optimization. * Mgmt: Give **IV iron (FCM 1000 mg if available)** to increase Hb/iron stores quickly pre-op; if immediate correction required and Hb very low → transfuse perioperatively. --- ### Case 25 — Anaemia in pregnancy with concurrent sepsis * Presentation: 29 y, fever, Hb 8.4 g/dL, high CRP. * Dx: Anaemia with infective/inflammatory component. * Mgmt: Treat infection promptly; avoid confounding ferritin interpretation; if iron deficiency coexists and severe → consider IV iron once infection controlled; transfuse if hemodynamically unstable. --- ### Case 26 — Peripartum transfusion reaction risk scenario * Presentation: 35 y, urgent PPH, requires transfusion; prior transfusion history with antibodies. * Dx: Acute blood loss anaemia with alloimmunisation risk. * Mgmt: Coordinate blood bank for phenotype-matched units; transfuse as required; consider tranexamic acid and uterotonics; document antibody and counsel for future pregnancies. --- ### Case 27 — Anaemia with hemolysis (autoimmune) * Presentation: 31 y, jaundice, Hb 7.6 g/dL, elevated LDH, indirect bilirubin, positive direct Coombs. * Dx: Autoimmune hemolytic anemia (AIHA) in pregnancy. * Mgmt: Hematology consult; treat (corticosteroids first-line), transfusion if needed (with crossmatch); avoid IV iron while active hemolysis unless iron deficient; monitor fetus for hydrops if severe. --- ### Case 28 — Iron overload concern (hemochromatosis suspicion) * Presentation: 34 y, elevated ferritin 500 ng/mL, high transferrin saturation, mild anemia. Family history of hemochromatosis. * Dx: Possible iron overload or inflammation. * Mgmt: Evaluate for hereditary hemochromatosis outside pregnancy (genetic testing, specialist input); avoid unnecessary iron; treat underlying cause of high ferritin (inflammation vs overload). --- ### Case 29 — Antenatal prophylaxis non-adherence with borderline anaemia * Presentation: 28 y, missed many ANC visits, Hb 10.6 g/dL, ferritin 22 ng/mL. * Dx: Borderline anemia/early IDA. * Mgmt: Reinforce routine prophylaxis (30–60 mg elemental iron + folic acid), provide education, address barriers (side effects, access), recheck Hb in 4 weeks and treat if progresses. --- ### Case 30 — Severe postpartum anaemia with breastfeeding * Presentation: 27 y, 2 weeks postpartum, Hb 6.8 g/dL, symptomatic (dizziness), breastfeeding. * Dx: Severe postpartum anaemia (likely iron deficient). * Mgmt: Consider transfusion if symptomatic/severe; give IV iron if breastfeeding and stable (IV iron safe in lactation); if oral is chosen, counsel on adherence and side effects; follow-up Hb and ferritin, continue iron 3 months after repletion. --- # Quick management reminders (pasteable) * **Screening**: Hb at booking and at 28 wks. * **Oral iron**: FS 325 mg ≈ 65 mg elemental; treatment = **60–120 mg elemental/day** until stores replete. Take on empty stomach with vitamin C; separate from antacids. * **IV iron**: Use for intolerance, non-response, late pregnancy needing rapid correction, malabsorption, or severe anaemia when oral not feasible. Iron sucrose (100–200 mg per dose) or FCM (single large dose 750–1000 mg). Monitor for reactions. * **Transfusion**: Individualise. Usually **Hb ≤7.0 g/dL** or symptomatic/hemodynamic compromise → transfuse. In obstetrics, clinical scenario dictates threshold. * **Follow-up**: Check Hb 2–4 weeks after therapy start and continue iron for 3 months after normalization. --- If you want, I can now: * Convert these into a **printable PDF** or a **spreadsheet** for easy use; * Expand any selected cases into **full exam-style long cases** (history prompts, viva questions, stepwise management) or **MCQs** derived from these cases; * Produce the **25 MCQs in stylish exam mode** (single HTML file with CSS/JS) instead — tell me which format you prefer next and I’ll produce it immediately. # Anaemia in pregnancy — complete, stylish clinical note > Compact, exam-friendly, evidence-backed reference you can paste into notes or teaching slides. Sources for the most important guideline facts are cited inline. --- ## 1) Definition (WHO) Anaemia = low haemoglobin (Hb) or red-cell mass causing reduced O₂-carrying capacity. **WHO threshold in pregnancy:** **Hb < 110 g/L (11.0 g/dL)** = anaemia; **severe** = **< 70 g/L (7.0 g/dL)**. ([World Health Organization][1]) --- ## 2) Pathophysiology (short) * Pregnancy → plasma volume ↑ ≈ 30–50% while red-cell mass ↑ less → physiologic haemodilution (lower Hb). * Pathologic anaemia results when iron supply (diet + stores) cannot meet increased maternal/fetal demands → reduced haemoglobin synthesis → microcytic hypochromic RBCs (longstanding). * Other mechanisms: haemoglobinopathy, folate/B12 deficiency, chronic inflammation (anemia of chronic disease, ACD), hemolysis, acute blood loss. --- ## 3) Iron requirements in pregnancy & prophylaxis (practical) * Pregnancy increases iron need substantially (for maternal RBC mass, placenta and fetus). Guidelines recommend **daily oral iron 30–60 mg elemental iron + 400 µg folic acid** for routine antenatal prophylaxis (start early, usually from 12 weeks or at first contact per local policy). For treatment, higher elemental doses are used (see below). ([World Health Organization][2]) --- ## 4) Public-health: Anemia Mukt Bharat & IFA logistics (India) * **Anemia Mukt Bharat (NHM)** emphasises six strategic actions including IFA supplementation, deworming, food fortification, testing & treatment, behaviour change and special management of severe cases. Weekly IFA formulations for adolescents/adults vary by group (e.g., 45–60 mg elemental iron + folic acid 400–500 µg for weekly program tablets); pregnant women receive daily IFA through ANC (tablet composition and supply per NHM/ANC). ([National Health Mission][3]) > Note about **“I-NIAP”**: I searched for a standard term “I-NIAP” and could not find an established definition. In obstetric literature you’ll see **AIP / NAIP** (Anemia In Pregnancy / Non-Anemic In Pregnancy) used in studies. If you meant a specific program/term, tell me and I’ll fetch it. ([sid.ir][4]) --- ## 5) Clinical history (what to ask) * Symptoms: fatigue, exertional dyspnoea, palpitations, syncope, orthopea, pica (pagophagia), restless legs, diminished exercise tolerance. * Obstetric: prior PPH, multiple pregnancies, short interpregnancy interval, hyperemesis, dietary restrictions, bleeding (menorrhagia pre-pregnancy), parasites, recent infections. * Drugs: antacids, calcium, tetracyclines (interfere with iron). * Family history: haemoglobinopathies (thalassaemia trait). --- ## 6) Physical examination (key findings) * Pallor (conjunctiva, palmar crease), tachycardia, glossitis, koilonychia (severe chronic), systolic flow murmur, signs of heart failure if severe. Look for hepatosplenomegaly (hemolysis/thalassaemia), lymphadenopathy (chronic disease). --- ## 7) Investigations — how to approach & interpretation **First-line tests** * CBC with RBC indices (Hb, Hct, MCV, MCH, MCHC), reticulocyte count, peripheral smear. * Ferritin (best single test for iron stores unless inflammation present), serum iron, TIBC/transferrin, transferrin saturation. ([MSD Manuals][5]) **Key numbers** * **MCV normal** ≈ 80–100 fL (microcytic <80 fL). (Use lab reference ranges.) ([MSD Manuals][5]) **Mentzer index** (practical discriminator) * **Mentzer = MCV (fL) / RBC count (10^6/µL)**. * **>13 → likely Iron Deficiency Anaemia (IDA)**. * **<13 → likely β-thalassaemia trait**. ([PMC][6]) **Peripheral smear** * IDA: microcytic hypochromic RBCs, anisopoikilocytosis, pencil cells. * ACD: often normocytic or mildly microcytic with low serum iron but low TIBC. Ferritin is normal or high in ACD (acute phase reactant). **Hb electrophoresis** * Indication: to detect β-thalassaemia trait or other hemoglobinopathies when indices suggest trait (normal/high RBC count, low MCV, Mentzer <13). Confirm with HbA₂ levels. ([PMC][7]) **Ferritin interpretation** * Low ferritin confirms iron deficiency; ferritin is raised in inflammation — interpret with CRP/ESR. WHO/technical guidance gives ferritin cutoffs and handling when inflammation present. ([World Health Organization][8]) --- ## 8) IDA vs Anaemia of Chronic Disease (ACD) — key contrasts * **IDA:** low ferritin, low serum iron, high TIBC (or normal), low transferrin saturation; microcytic hypochromic RBCs. * **ACD:** low serum iron, **low/normal TIBC**, normal/high ferritin, low transferrin saturation; usually occurs with infection/inflammation/chronic disease. Treatment targets underlying disease + careful iron management. ([World Health Organization][8]) --- ## 9) Differential diagnoses to consider * Iron deficiency, haemoglobinopathies (thalassaemia trait), folate/B12 deficiency, ACD, hemolytic anaemias, blood loss (antepartum/PPH), bone marrow disorders. --- ## 10) Complications & adverse effects of anaemia in pregnancy **Maternal effects** * Fatigue, reduced work capacity, increased risk of cardiac failure if severe, increased risk of peripartum transfusion and infection, poor wound healing, higher maternal mortality in severe anaemia. ([World Health Organization][9]) **Fetal/neonatal effects** * Preterm birth, low birth weight, intrauterine growth restriction, perinatal mortality, impaired neurodevelopment if severe/untreated. --- ## 11) Management — overview (prevention → treat → rescue) **Goals:** correct Hb, replete iron stores (ferritin), prevent recurrence, avoid transfusion when possible. ### A. Prevention (policy/antenatal) * Diet counselling (iron-rich foods + vitamin C to increase absorption; avoid tea/coffee with meals). * Routine **daily IFA prophylaxis: 30–60 mg elemental iron + 400 µg folic acid** (WHO). For national programs (India) follow Anemia Mukt Bharat / ANC protocols for supply and deworming. ([World Health Organization][2]) ### B. Oral iron — first-line for mild–moderate IDA and prophylaxis **Common salts & elemental iron content (practical)** * **Ferrous sulfate 325 mg** ≈ **65 mg elemental iron** (varies with hydrate). * **Ferrous fumarate 300 mg** ≈ **99–100 mg elemental iron**. * **Ferrous gluconate 300/325 mg** ≈ **35–39 mg elemental iron**. (Check product label.) ([NCBI][10]) **Indication (pregnancy):** treatment when IDA confirmed (mild–moderate), prophylaxis as above. **Dosing (typical)** * **Prophylaxis:** 30–60 mg elemental iron daily + 400 µg folic acid. ([World Health Organization][2]) * **Treatment (common practice):** many formularies use **60–120 mg elemental iron daily** (often given as 1 tab of ferrous sulfate 325 mg × 1–3 daily depending on severity) or **single daily higher elemental dose**; some guidelines/recent studies favour **lower daily doses (e.g., 60–80 mg elemental once daily)** or alternate-day dosing to improve tolerance and absorption — tailor to local guidance and tolerance. ([ScienceDirect][11]) **Mechanism of action:** provides elemental iron for haemoglobin synthesis; absorbed in duodenum via DMT1 after reduction to ferrous form. **Pharmacokinetics (summary):** oral iron variably absorbed (5–30% depending on iron status, enhancers/inhibitors). Food reduces absorption; vitamin C enhances. **Adverse effects (oral):** GI upset, nausea, abdominal pain, constipation or diarrhoea, black stools; adherence often limited by GI side effects. ([National Health Mission][12]) **Contraindications:** known hypersensitivity; caution with hemochromatosis. Check for haemoglobinopathy before prolonged high-dose therapy. **Key interactions:** antacids, calcium, tetracyclines, some antibiotics — separate dosing by 2–3 hours. Vitamin C coadministration improves absorption. **Monitoring:** Hb every 2–4 weeks until rise (aim Hb ↑ by ~1 g/dL in 2–4 weeks), ferritin at baseline and after repletion; monitor adherence and GI side effects. **Counselling points to patient:** take on empty stomach if tolerated (or with small vitamin-C-rich juice), avoid tea/coffee within 1–2 hours, black stools are common and harmless, constipation can be managed with stool softener/diet. Keep out of reach of children (ingestion is toxic). --- ### C. Parenteral (IV) iron — when to use **Indications in pregnancy** * Severe IDA not corrected by oral iron, intolerance or non-adherence to oral iron, late pregnancy where rapid correction needed, malabsorption, ongoing significant bleeding, or when quick Hb rise needed before delivery/cesarean. Avoid routine use in first trimester when possible. ([Wiley Online Library][13]) **Preparations & dosing (practical)** * **Iron sucrose (Venofer):** repeated doses (e.g., 100–200 mg per infusion; typical cumulative calculated by Ganzoni or dosing tables). Max ~200 mg per infusion commonly used; total depends on deficit. ([transfusionguidelines.org][14]) * **Ferric carboxymaltose (FCM; Injectafer/Ferinject):** allows **larger single doses (up to ~750–1000 mg per infusion, product-specific limits ~15–20 mg/kg, max 1000 mg single dose)** — useful to correct iron deficit quickly in 1–2 visits. ([injectaferhcp.com][15]) **Mechanism:** IV complexes deliver iron directly to reticuloendothelial system for incorporation into ferritin/haemoglobin. **Adverse effects (IV):** infusion reactions (including rare anaphylaxis with older dextran formulations), transient hypotension, nausea, arthralgia, local irritation; hypophosphatemia reported with some agents (e.g., FCM). Monitor for hypersensitivity during infusion. ([PMC][16]) **Monitoring:** vitals during infusion, monitor Hb/ferritin 2–4 weeks post infusion; check phosphate if using FCM and high cumulative dose. **Counselling:** explain need for IV access, possible transient side effects, and post-infusion monitoring. --- ### D. Blood transfusion — when & how (obstetric specifics) **Indications:** individualised — combine clinical state and Hb level. Many guidelines say transfusion is usual when **Hb < 60–70 g/L** or if symptomatic/hemodynamically unstable; rarely needed if Hb > 100 g/L. In obstetrics, clinical context (ongoing bleeding, cardiovascular compromise, labour) is decisive. Cross-match and plan ahead for high-risk women. Use single donor PRBCs, match Rh/K testing, and consider component therapy. ([RCOG][17]) **Risks:** transfusion reactions, alloimmunisation, infection risk (low with modern screening), transfusion-associated circulatory overload; plan restrictive transfusion strategy where safe. --- ## 12) Stepwise treatment algorithm (practical summary) 1. **Screen all pregnant women at booking** (Hb + RBC indices). If Hb <110 g/L → further tests (CBC, ferritin ± iron studies). ([World Health Organization][1]) 2. **If IDA confirmed (low ferritin):** start/optimise oral iron (elemental 60–120 mg/day, adjust to tolerance). Counsel. Monitor Hb rise at 2–4 weeks. If inadequate response or very late pregnancy / urgent correction required → **IV iron** (calculate total deficit; consider FCM or iron sucrose per availability). ([ScienceDirect][11]) 3. **If severe symptomatic anaemia (Hb <70 g/L) or haemodynamic instability:** consider blood transfusion (obstetric judgement). ([RCOG][17]) --- ## 13) Prevention of recurrence & antenatal program tips * Give full course until 3 months postpartum if previously anaemic, ensure deworming (in areas endemic for helminths) per national policy, ensure adequate dietary counselling, consider screening for haemoglobinopathies if family history or persistent microcytosis after iron repletion. Use Anemia Mukt Bharat operational modules to plan community IFA distribution and counselling. ([i4n.in][18]) --- ## 14) Quick bedside pocket facts (copy-paste) * **WHO anaemia in pregnancy:** Hb <11.0 g/dL. ([World Health Organization][1]) * **Routine prophylaxis:** **30–60 mg elemental iron + 400 µg folic acid daily.** ([World Health Organization][2]) * **Oral elemental iron examples:** ferrous sulfate 325 mg ≈ 65 mg Fe; ferrous fumarate 300 mg ≈ 99 mg Fe; ferrous gluconate 300 mg ≈ 35 mg Fe. ([NCBI][10]) * **Mentzer index:** MCV/RBC; **>13 → IDA**, **<13 → thalassaemia trait**. ([PMC][6]) --- ## 15) Practical templates (for your notes) **A. ANC counselling line:** “You have mild iron deficiency. I’m starting oral iron (example: ferrous sulfate 325 mg **once daily** = ~65 mg elemental iron) + folic acid — take on empty stomach or with orange juice, expect black stools; call if severe abdominal pain or fainting.” **B. IV iron note:** “Given poor response/intolerance to oral iron or late pregnancy, plan IV ferric carboxymaltose **(calculate total deficit; often one 1000 mg infusion)** — monitor vitals during infusion, check Hb & ferritin at 2–4 weeks.” --- ## 16) References / further reading (selected, guideline-level) * WHO Anaemia fact sheet & Hb thresholds. ([World Health Organization][9]) * WHO recommendations: daily iron & folic acid supplementation in pregnancy. ([World Health Organization][2]) * Anemia Mukt Bharat training & operational guidance (India/NHM). ([National Health Mission][3]) * Mentzer index & RBC indices literature. ([PMC][6]) * IV iron reviews & product dosing (iron sucrose, ferric carboxymaltose) and obstetric use. ([PMC][16]) * RCOG / Green-top on blood transfusion in obstetrics. ([RCOG][17]) --- If you want, I can now: * Convert this into a **stylish one-page printable handout (PDF)**; * Generate **30 case scenarios with management** (you previously asked for many cases) or **25 MCQs in exam mode** with HTML/CSS/JS; * Produce an **SEO title/description/keywords** and **an illustrative image** (I can generate an image for a teaching slide). Tell me which follow-up you want and I’ll produce it in the same detailed style. [1]: https://cdn.who.int/media/docs/default-source/anaemia-in-women-and-children/hb-methods-for-gather.pdf?sfvrsn=da0fbb5f_11&utm_source=chatgpt.com "WHO methods and data sources for mean haemoglobin ..." [2]: https://www.who.int/tools/elena/interventions/daily-iron-pregnancy?utm_source=chatgpt.com "Daily iron and folic acid supplementation during pregnancy" [3]: https://nhm.gov.in/index1.php?lang=1&level=3&lid=797&sublinkid=1448&utm_source=chatgpt.com "Anaemia Mukt Bharat" [4]: https://www.sid.ir/paper/1056249/en?utm_source=chatgpt.com "Haemoglobin Level of Pregnant Women on First ..." [5]: https://www.msdmanuals.com/professional/multimedia/table/typical-normal-serum-values-for-iron-iron-binding-capacity-ferritin-and-transferrin-saturation?utm_source=chatgpt.com "Table: Typical Normal Serum Values for Iron, Iron-Binding ..." [6]: https://pmc.ncbi.nlm.nih.gov/articles/PMC9121960/?utm_source=chatgpt.com "Role of Mentzer index for differentiating iron deficiency ..." [7]: https://pmc.ncbi.nlm.nih.gov/articles/PMC5467296/?utm_source=chatgpt.com "Iron Deficiency Anemia or β-Thalassemia Trait? - PMC" [8]: https://www.who.int/docs/default-source/micronutrients/ferritin-guideline/ferritin-guidelines-brochure.pdf?sfvrsn=76a71b5a_4&utm_source=chatgpt.com "ferritin-guidelines-brochure.pdf" [9]: https://www.who.int/news-room/fact-sheets/detail/anaemia?utm_source=chatgpt.com "Anaemia" [10]: https://www.ncbi.nlm.nih.gov/books/NBK548214/table/Iron.T1/?utm_source=chatgpt.com "[Table, Concentrations of elemental iron in typical iron tablets]" [11]: https://www.sciencedirect.com/science/article/pii/S0098299720300364?utm_source=chatgpt.com "Oral iron supplementation in iron-deficient women" [12]: https://nhm.gov.in/images/pdf/programmes/wifs/guidelines/icds_operational_guidelines_for_wifs.pdf?utm_source=chatgpt.com "Operational Guidelines for Weekly IFA Supplementation ..." [13]: https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.27220?utm_source=chatgpt.com "Expert consensus guidelines: Intravenous iron uses, ..." [14]: https://www.transfusionguidelines.org/document-library/documents/protocol-for-the-use-of-iv-iron-sucrose/download-file/rtc-eeng_protocol_iv_iron_sucrose.pdf?utm_source=chatgpt.com "IV iron sucrose Venofer protocol v1.0 Jan08" [15]: https://injectaferhcp.com/iron-injection-administration?utm_source=chatgpt.com "Dosing and Administration" [16]: https://pmc.ncbi.nlm.nih.gov/articles/PMC9722303/?utm_source=chatgpt.com "Ferric Carboxymaltose in the Management of Iron ..." [17]: https://www.rcog.org.uk/media/sdqcorsf/gtg-47.pdf?utm_source=chatgpt.com "Blood Transfusion in Obstetrics" [18]: https://www.i4n.in/wp-content/uploads/2023/05/Anemia-Mukt-Bharat-Training-Modules-english.pdf?utm_source=chatgpt.com "ANEMIA MUKT BHARAT"
Heart Disease in Pregnancy: Causes, Risks, Management & 20 Case-Based MCQs (With Answers & Explanations)
Below is a **complete, exam-ready, concise-but-exhaustive reference** for **Heart Disease in Pregnancy** — covering definition, physiology, classification, clinical features, investigations, management (stepwise), drug details, labor/delivery planning, postpartum care, and contraindications. --- # **Heart Disease in Pregnancy – Complete Overview** ! --- ## **1. Definition** Heart disease in pregnancy refers to **pre-existing cardiac disorders** (congenital or acquired) or **pregnancy-induced cardiac dysfunction** (e.g., peripartum cardiomyopathy) that complicate pregnancy, labor, or postpartum period. --- ## **2. Why Pregnancy Worsens Heart Disease (Physiological Changes)** Pregnancy causes major hemodynamic changes that peak at **28–32 weeks**: * **↑ Blood volume by 40–50%** * **↑ Cardiac output by 30–50%** * **↑ Heart rate by 10–20 bpm** * **↓ Systemic vascular resistance** * **Hypercoagulable state** * **During labor:** CO ↑ 20–30% more * **Immediately postpartum:** Autotransfusion ↑ CO up to 80% These changes may **unmask latent heart disease** or **worsen existing cardiac failure**. --- ## **3. Types of Heart Diseases Seen in Pregnancy** ### **A. Congenital Heart Disease (CHD)** * Atrial septal defect (ASD) * Ventricular septal defect (VSD) * Patent ductus arteriosus (PDA) * Tetralogy of Fallot (repaired/unrepaired) * Eisenmenger syndrome (very high-risk) ### **B. Acquired Heart Disease** * Rheumatic heart disease * Mitral stenosis (most common serious lesion in pregnancy) * Mitral regurgitation * Aortic stenosis * Cardiomyopathies * **Peripartum cardiomyopathy** * Ischemic heart disease * Arrhythmias * Hypertensive heart disease --- ## **4. WHO Classification of Maternal Cardiovascular Risk** ### **WHO Class I – Low Risk** * Small ASD/VSD * PDA * Mitral valve prolapse * Successfully repaired simple CHD ### **WHO Class II – Moderate Risk** * Unrepaired ASD/VSD * Repaired TOF * Mild LV dysfunction ### **WHO Class III – High Risk** * Mechanical valves * Cyanotic congenital heart disease * Moderate LV dysfunction * Previous peripartum cardiomyopathy with normal EF now ### **WHO Class IV – Extremely High Risk (Pregnancy Contraindicated)** * **Pulmonary hypertension / Eisenmenger syndrome** * **Severe LV dysfunction (EF < 30%)** * **Severe mitral stenosis or aortic stenosis** * **Marfan syndrome with aorta > 45 mm** * **Previous peripartum cardiomyopathy with persistent dysfunction** --- ## **5. Clinical Features** ### **Symptoms** * Dyspnea (especially NYHA III–IV) * Orthopnea / PND * Fatigue * Palpitations * Chest pain * Syncope ### **Warning Features of Cardiac Decompensation** * Dyspnea at rest * Hemoptysis * Cyanosis * Loud P2 / RV heave * Basal crepitations * New arrhythmias --- ## **6. Investigations** ### **Basic** * CBC * ECG * **Echocardiography – Most important** * BNP (optional) ### **Advanced** * Cardiac MRI (safe without gadolinium) * Holter monitoring * Exercise testing (pre-pregnancy only) ### **Avoid** * CT angiography unless life-saving * ACE inhibitors / ARBs history to be checked --- ## **7. Complications** * **Maternal:** Heart failure, arrhythmias, thromboembolism, endocarditis, cardiac arrest * **Fetal:** IUGR, preterm birth, fetal hypoxia, congenital heart disease (3–5% risk) --- # **8. Management of Heart Disease in Pregnancy (Stepwise)**   --- ## **A. Preconception Counselling** * Risk assessment + WHO classification * Optimize cardiac status (e.g., balloon valvotomy for MS) * Stop teratogenic drugs (ACE inhibitors, ARBs, statins, warfarin if possible) --- ## **B. Antenatal Management** ### **1. Lifestyle** * Adequate rest * Left lateral position * Avoid anemia (treat aggressively) * Avoid excessive weight gain * Salt restriction if HF symptoms ### **2. Drugs Used** Below are the major drug classes **with indications, mechanism, dosing, adverse effects, contraindications, interactions, and counselling.** --- ## **i. Diuretics (Furosemide)** **Indication:** Heart failure, pulmonary edema **MOA:** Loop diuretic → inhibits Na-K-2Cl in loop of Henle **Dose:** 20–40 mg PO/IV, repeat as required **PK:** Rapid onset, renal excretion **AEs:** Hypokalemia, dehydration **Contra:** Severe electrolyte imbalance **Interactions:** Digoxin ↑ toxicity if hypokalemia **Counselling:** Monitor weight, urine output, electrolytes --- ## **ii. Beta-blockers (Metoprolol preferred)** **Indication:** Rate control, arrhythmias, ischemic heart disease **MOA:** Blocks β1 receptors → ↓ HR & contractility **Dose:** 25–100 mg/day **AEs:** IUGR (minimal), bradycardia **Contra:** Severe asthma **Interactions:** Calcium channel blockers → heart block risk **Counselling:** Do not stop suddenly --- ## **iii. Anticoagulants** ### **a. LMWH (Enoxaparin) – Preferred** **Indication:** Mechanical valves, AF, thromboembolism **MOA:** Enhances antithrombin III → inhibits Xa **Dose:** 1 mg/kg twice daily **Monitoring:** Anti-Xa levels **AEs:** Bleeding **Contra:** Active bleeding ### **b. Warfarin – Teratogenic (avoid 6–12 weeks)** Used only when valve thrombosis risk is very high. --- ## **iv. Vasodilators (Hydralazine, Nitrates)** **Indication:** HF with hypertension **AEs:** Headache, hypotension --- ## **v. Digoxin** **Indication:** HF with atrial fibrillation **MOA:** Na-K ATPase inhibition → ↑ Ca → ↑ contractility **Dose:** 0.125–0.25 mg daily **AEs:** Toxicity (nausea, vision changes) **Monitor:** Serum levels --- ## **Drugs Contraindicated in Pregnancy** * **ACE inhibitors / ARBs** → renal failure, skull defects * **Amiodarone** → fetal thyroid dysfunction * **Warfarin (first trimester)** unless essential * **Statins** --- ## **C. Follow-up Schedule** * Monthly (WHO I–II) * Fortnightly (WHO III) * Weekly (WHO IV — pregnancy discouraged) --- # **9. Labor and Delivery Management**   ### **Preferred Mode:** **Vaginal delivery with epidural anesthesia** ### **Indications for Caesarean Section** * Severe aortic stenosis * Marfan with aortic root dilation * Eisenmenger * Severe HF * Anticoagulation not stopped ### **Intrapartum Measures** * Continuous ECG + pulse oximetry * Avoid fluid overload * Slow, assisted second stage (forceps/vacuum) ### **Anesthesia** * Epidural preferred * Avoid general anesthesia (↑ cardiac stress) --- # **10. Postpartum Care** * Highest risk of heart failure in **first 24–72 hours** * Gradual mobilization * Restart anticoagulation after 6 hours (if needed) * Contraception counselling * **Avoid estrogen pills** * Prefer: IUCD, progestin-only methods --- # **11. High-Risk Specific Conditions** ## **A. Mitral Stenosis** * Most dangerous RHD lesion in pregnancy * Tachycardia → ↑ LA pressure → pulmonary edema * Management: β-blockers + diuretics * Balloon valvotomy if severe --- ## **B. Eisenmenger Syndrome** * **Pregnancy contraindicated (WHO IV)** * Maternal mortality 30–50% * No effective treatment → counselling for termination --- ## **C. Peripartum Cardiomyopathy** * Heart failure in last month of pregnancy or 5 months postpartum * EF < 45% * Treatment: * Diuretics * Beta-blockers * Bromocriptine (stops prolactin → improves function) * Avoid future pregnancy if EF not normalized --- # **12. Fetal Risks** * Prematurity * Growth restriction * Neonatal asphyxia * Congenital heart disease (if mother has CHD) --- # **13. Key Prevention Strategies** * Early diagnosis * Control anemia * Avoid excessive fluids * Use cardiac medications judiciously * Multidisciplinary care (obstetrician + cardiologist) --- # **Would you like a SEO-optimized title & description for this topic, or a high-ranking blog article version?**
Comments & Discussion
Use this thread like a mini viva: add differentials, staging systems, drug regimens and exam tricks.
Login or register to comment.
No comments yet – start by adding exam-style discussion points.