Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
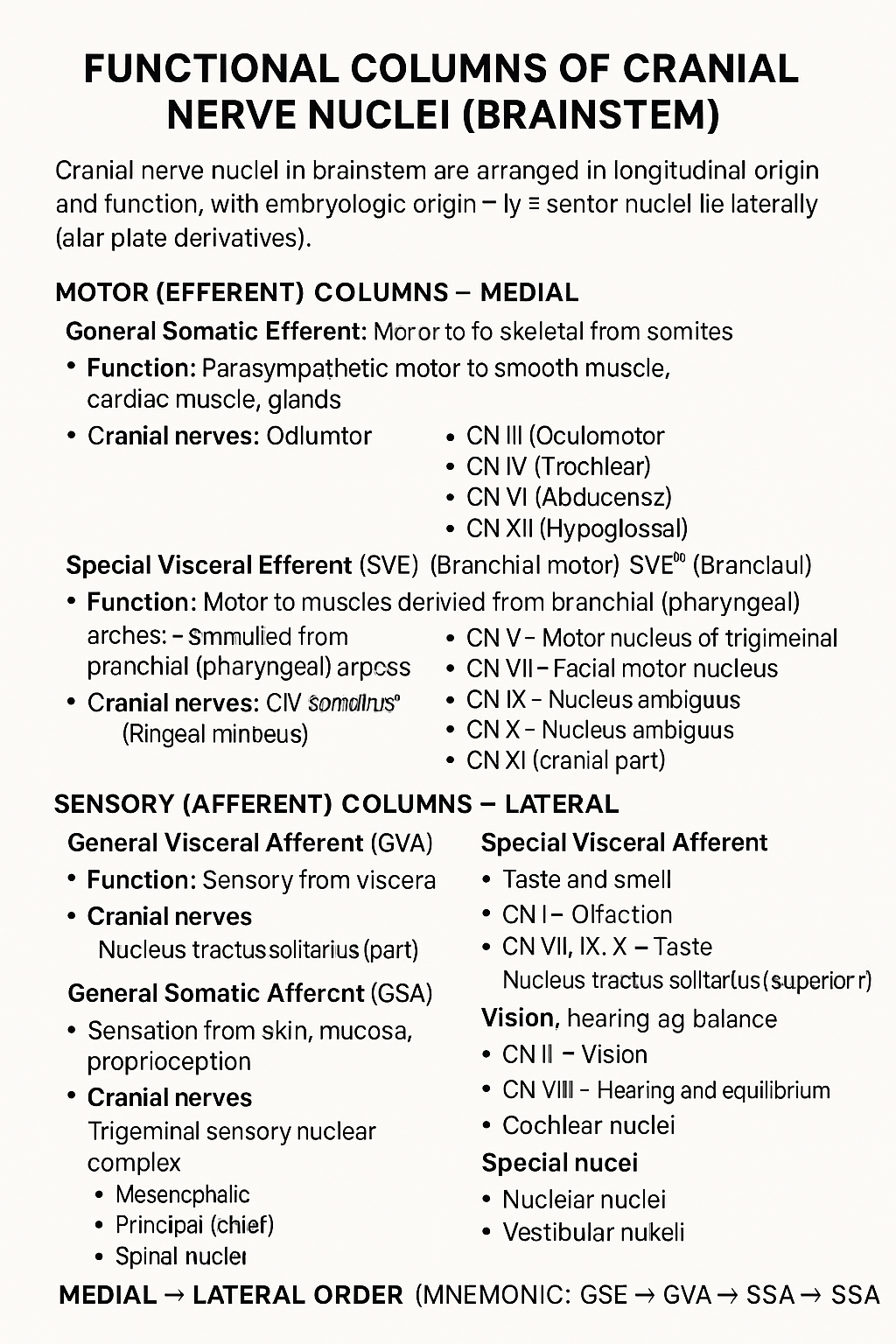
Functional Columns of Cranial Nerve Nuclei in Brainstem
## Functional Columns of Cranial Nerve Nuclei (Brainstem) Cranial nerve nuclei in the brainstem are arranged in **longitudinal functional columns** based on **embryologic origin** and **function**. **Motor nuclei lie medially** (basal plate derivatives) and **sensory nuclei lie laterally** (alar plate derivatives). --- ## MOTOR (EFFERENT) COLUMNS – Medial ### 1. **General Somatic Efferent (GSE)** * **Function:** Motor to skeletal muscles derived from **somites** * **Muscles supplied:** Extraocular muscles, tongue muscles * **Cranial nerves:** * CN III (Oculomotor) * CN IV (Trochlear) * CN VI (Abducens) * CN XII (Hypoglossal) --- ### 2. **General Visceral Efferent (GVE)** * **Function:** **Parasympathetic** motor to smooth muscle, cardiac muscle, glands * **Cranial nerves & nuclei:** * CN III – Edinger–Westphal nucleus * CN VII – Superior salivatory nucleus * CN IX – Inferior salivatory nucleus * CN X – Dorsal motor nucleus of vagus --- ### 3. **Special Visceral Efferent (SVE)** *(Branchial motor)* * **Function:** Motor to muscles derived from **branchial (pharyngeal) arches** * **Muscles supplied:** Muscles of mastication, facial expression, pharynx, larynx * **Cranial nerves:** * CN V – Motor nucleus of trigeminal * CN VII – Facial motor nucleus * CN IX – Nucleus ambiguus * CN X – Nucleus ambiguus * CN XI (cranial part) --- ## SENSORY (AFFERENT) COLUMNS – Lateral ### 4. **General Visceral Afferent (GVA)** * **Function:** Sensory from viscera * **Cranial nerves:** * CN IX * CN X * **Nucleus:** Nucleus tractus solitarius (inferior part) --- ### 5. **Special Visceral Afferent (SVA)** * **Function:** Taste and smell * **Cranial nerves:** * CN I – Olfaction * CN VII, IX, X – Taste * **Nucleus:** Nucleus tractus solitarius (superior part) --- ### 6. **General Somatic Afferent (GSA)** * **Function:** Sensation from skin, mucosa, proprioception * **Cranial nerves:** * CN V (main) * CN VII, IX, X (small contributions) * **Nuclei:** * Trigeminal sensory nuclear complex * Mesencephalic * Principal (chief) * Spinal nucleus --- ### 7. **Special Somatic Afferent (SSA)** * **Function:** Vision, hearing, balance * **Cranial nerves:** * CN II – Vision * CN VIII – Hearing and equilibrium * **Nuclei:** * Cochlear nuclei * Vestibular nuclei --- ## MEDIAL → LATERAL ORDER (Mnemonic) **GSE → GVE → SVE → GVA → SVA → GSA → SSA** --- If you want, I can also provide: * **One-table summary (exam revision)** * **Clinical correlations** * **Simple mnemonics for each column** * **Neat labelled text diagram (ASCII-style)**
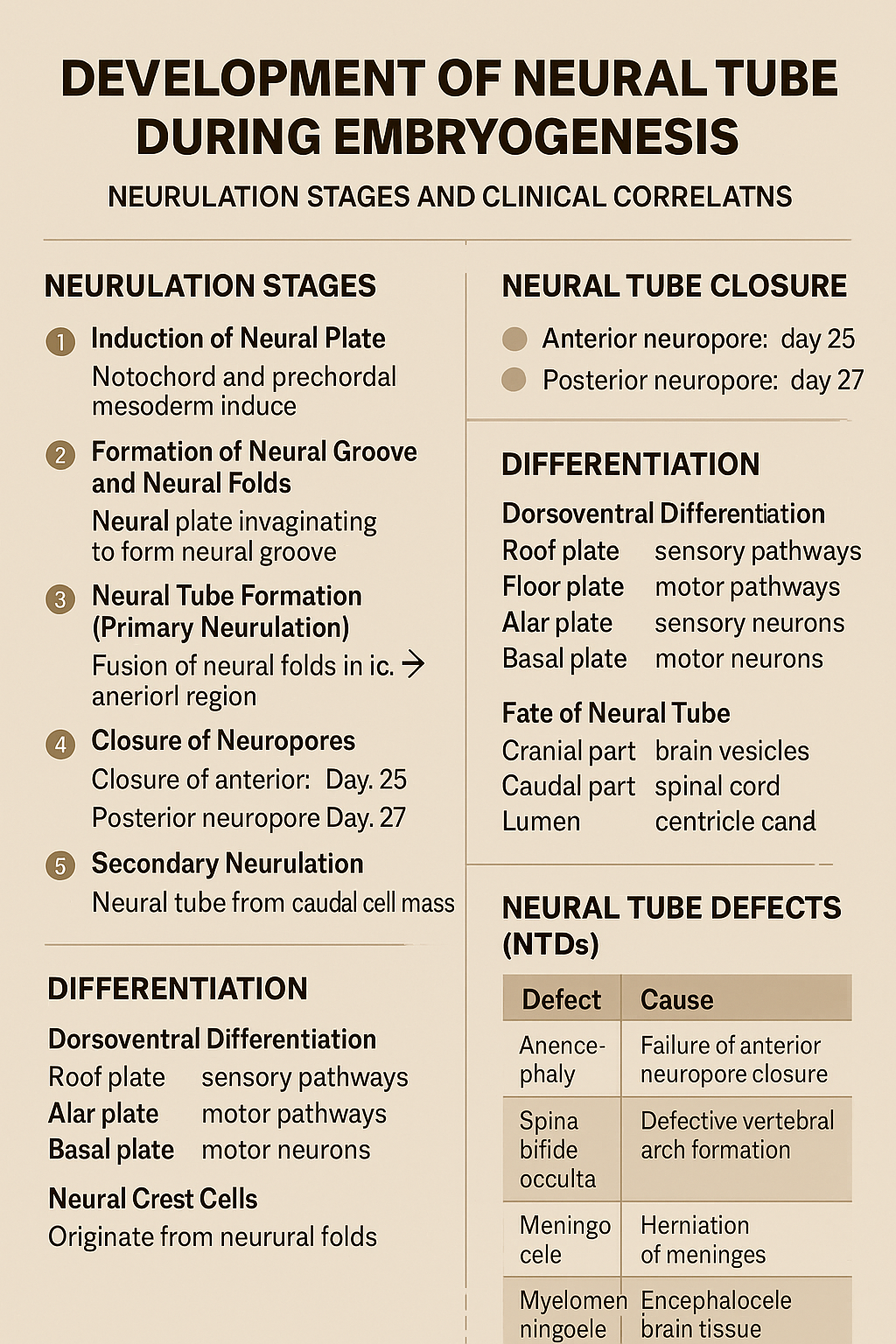
Development of Neural Tube During Embryogenesis Neurulation Stages and Clinical Correlation
## Development of the Neural Tube (Neurulation) ### **Definition** The **neural tube** is the embryonic precursor of the **central nervous system (CNS)**, forming the **brain and spinal cord**. Its development occurs by **neurulation** during the **3rd and 4th weeks of intrauterine life**. --- ## **Timeline** * **Day 18**: Neural plate appears * **Day 20–21**: Neural folds form * **Day 22**: Fusion begins in cervical region * **Day 25**: Closure of anterior (cranial) neuropore * **Day 27**: Closure of posterior (caudal) neuropore --- ## **Phases of Neural Tube Development** ### **1. Induction of Neural Plate** * The **notochord** and **prechordal mesoderm** induce overlying **ectoderm**. * Ectoderm thickens to form the **neural plate**. **Key signaling molecules**: * Sonic hedgehog (Shh) * Noggin * Chordin * Follistatin --- ### **2. Formation of Neural Groove and Neural Folds** * Central neural plate invaginates → **neural groove**. * Lateral edges elevate → **neural folds**. * Neural folds approach each other dorsally. --- ### **3. Neural Tube Formation (Primary Neurulation)** * Neural folds fuse in the **midline**, starting in the **cervical region**. * Fusion proceeds cranially and caudally. * Temporary openings remain: * **Anterior (cranial) neuropore** * **Posterior (caudal) neuropore** --- ### **4. Closure of Neuropores** * **Anterior neuropore closes (Day 25)** → brain development * **Posterior neuropore closes (Day 27)** → spinal cord development Failure of closure leads to **neural tube defects**. --- ### **5. Secondary Neurulation** * Occurs in the **caudal region (below S2)**. * Neural tube forms from **caudal cell mass**. * Important for formation of: * Conus medullaris * Filum terminale --- ## **Differentiation of the Neural Tube** ### **Neural Tube Wall Layers** 1. **Ventricular (ependymal) layer** – neuroepithelial cells 2. **Mantle layer** – gray matter 3. **Marginal layer** – white matter --- ### **Dorsoventral Differentiation** * **Roof plate** → sensory pathways * **Floor plate** → motor pathways * **Alar plate** → sensory neurons * **Basal plate** → motor neurons * **Sulcus limitans** separates alar and basal plates --- ## **Fate of Neural Tube** * **Cranial part** → brain vesicles * Prosencephalon * Mesencephalon * Rhombencephalon * **Caudal part** → spinal cord * **Lumen** → ventricles and central canal --- ## **Neural Crest Cells (Related Event)** * Originate from neural folds * Migrate extensively * Form: * Peripheral nervous system * Melanocytes * Adrenal medulla * Craniofacial cartilage --- ## **Clinical Correlation: Neural Tube Defects (NTDs)** | Defect | Cause | | -------------------- | ------------------------------------- | | Anencephaly | Failure of anterior neuropore closure | | Spina bifida occulta | Defective vertebral arch formation | | Meningocele | Herniation of meninges | | Myelomeningocele | Herniation of spinal cord + meninges | | Encephalocele | Herniation of brain tissue | **Risk factors**: * Folic acid deficiency * Maternal diabetes * Valproate exposure **Prevention**: * Folic acid 400–800 µg/day (preconception) --- ### **One-Line Exam Summary** > The neural tube forms from ectoderm by neurulation during weeks 3–4 and develops into the brain and spinal cord. If you want, I can also provide **exam-oriented MCQs, flowcharts, or comparison tables** for neurulation.
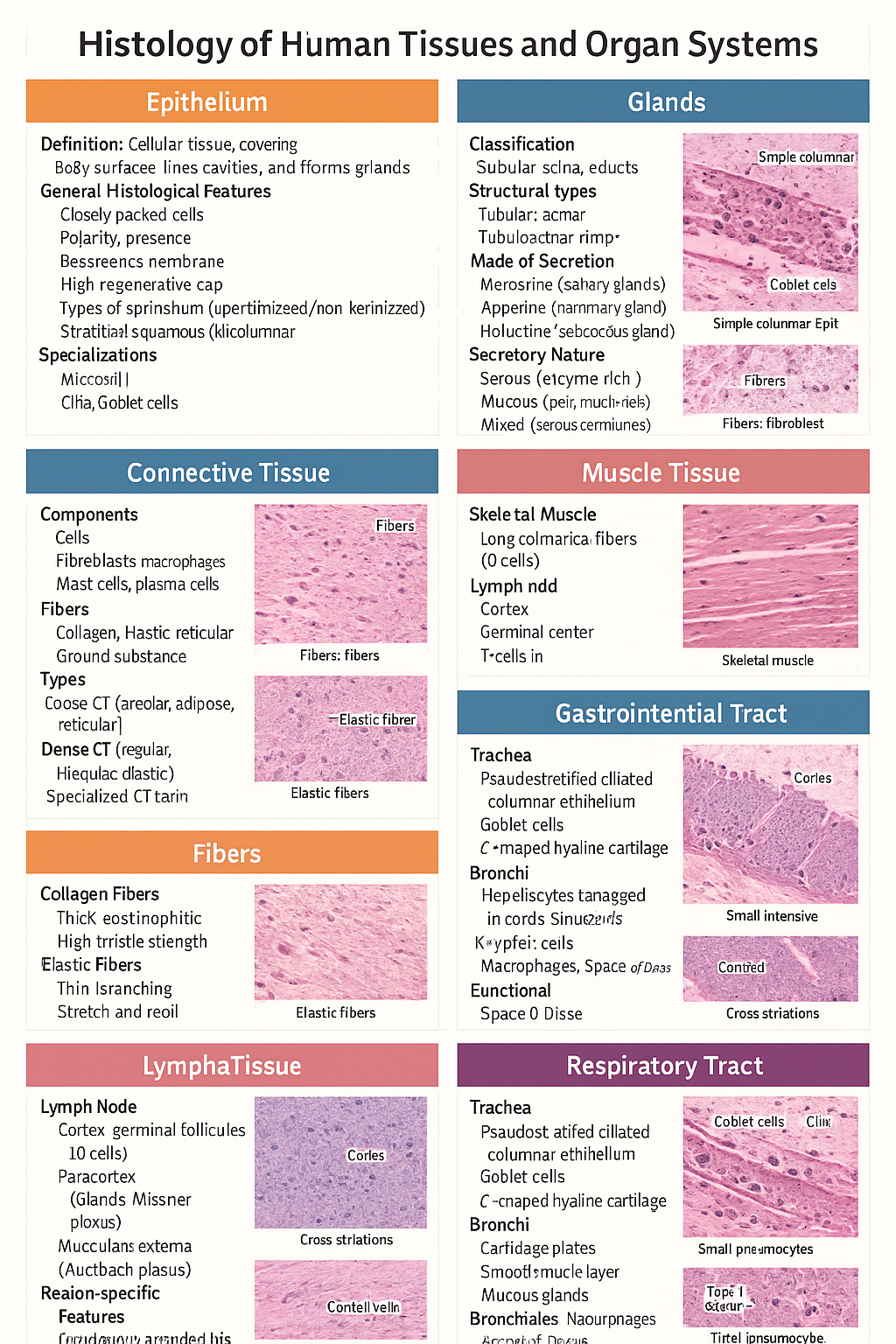
Histology of Epithelium, Connective Tissue, Muscle, Cartilage, Glands, GIT, Liver and Respiratory Tract
Below is a **single-place, SEO-optimized, exam-ready histology guide** covering **epithelium, glands, connective tissue, fibers, cartilage, muscle, lymphatic system, GIT, liver, and respiratory tract**. Structured with **clear H1–H3 headings**, **high-yield features**, and **clinical correlations** for medical students and competitive exams. --- # Histology of Human Tissues and Organ Systems – Complete Guide ## Histology of Epithelium ### Definition Epithelium is a **cellular tissue** that covers body surfaces, lines cavities, and forms glands. ### General Histological Features * Closely packed cells with **minimal extracellular matrix** * **Polarity**: apical, lateral, basal surfaces * **Basement membrane** present * **Avascular**, richly innervated * High **regenerative capacity** ### Types of Epithelium * **Simple squamous**: alveoli, capillaries * **Simple cuboidal**: kidney tubules, glands * **Simple columnar**: stomach, intestine * **Stratified squamous (keratinized/non-keratinized)**: skin / oral cavity * **Pseudostratified ciliated columnar**: trachea * **Transitional epithelium**: urinary bladder ### Specializations * **Microvilli** – absorption * **Cilia** – movement * **Goblet cells** – mucus secretion --- ## Histology of Glands ### Classification * **Exocrine glands** – ducts present * **Endocrine glands** – ductless, secrete into blood ### Structural Types * **Tubular**, **acinar**, **tubuloacinar** * **Simple** or **compound** ### Mode of Secretion * **Merocrine** (salivary glands) * **Apocrine** (mammary gland) * **Holocrine** (sebaceous gland) ### Secretory Nature * **Serous** – enzyme-rich, dark staining * **Mucous** – pale, mucin-rich * **Mixed** – serous demilunes --- ## Histology of Connective Tissue ### Components * **Cells**: fibroblasts, macrophages, mast cells, plasma cells * **Fibers**: collagen, elastic, reticular * **Ground substance**: proteoglycans, GAGs ### Types * **Loose CT**: areolar, adipose, reticular * **Dense CT**: regular, irregular, elastic * **Specialized CT**: cartilage, bone, blood --- ## Histology of Fibers ### Collagen Fibers * Thick, eosinophilic * High tensile strength * Seen in tendons, ligaments ### Elastic Fibers * Thin, branching * Stretch and recoil * Found in lungs, elastic arteries ### Reticular Fibers * Type III collagen * Supportive network * Seen in lymphoid organs --- ## Histology of Cartilage ### General Features * Avascular * Chondrocytes in **lacunae** * Perichondrium present (except articular cartilage) ### Types * **Hyaline cartilage**: trachea, articular surfaces * **Elastic cartilage**: pinna, epiglottis * **Fibrocartilage**: intervertebral discs, pubic symphysis --- ## Histology of Muscle Tissue ### Skeletal Muscle * Long cylindrical fibers * **Multinucleated**, peripheral nuclei * Cross striations present * Voluntary ### Cardiac Muscle * Branching fibers * Single central nucleus * **Intercalated discs** * Involuntary ### Smooth Muscle * Spindle-shaped cells * No striations * Involuntary * Found in viscera, vessels --- ## Histology of Lymphatic System ### Lymph Node * Capsule with trabeculae * **Cortex**: lymphoid follicles (B cells) * **Paracortex**: T cells * **Medulla**: medullary cords and sinuses ### Spleen * **White pulp**: lymphocytes around central artery * **Red pulp**: sinusoids and splenic cords ### Thymus * Cortex and medulla * **Hassall’s corpuscles** * T-cell maturation --- ## Histology of Gastrointestinal Tract (GIT) ### Common Layers 1. **Mucosa** – epithelium, lamina propria, muscularis mucosa 2. **Submucosa** – glands, Meissner plexus 3. **Muscularis externa** – Auerbach plexus 4. **Serosa/adventitia** ### Region-Specific Features * **Esophagus**: stratified squamous epithelium * **Stomach**: simple columnar epithelium, gastric glands * **Small intestine**: villi, plicae circulares, Peyer’s patches (ileum) * **Colon**: no villi, abundant goblet cells --- ## Histology of Liver ### Structural Unit * **Classical hepatic lobule** * Central vein * Portal triad: hepatic artery, portal vein, bile duct ### Cellular Features * Hepatocytes arranged in cords * **Sinusoids** lined by fenestrated endothelium * **Kupffer cells** – macrophages * **Space of Disse** ### Functional Significance * Metabolism * Detoxification * Bile production --- ## Histology of Respiratory Tract ### Trachea * Pseudostratified ciliated columnar epithelium * Goblet cells * C-shaped hyaline cartilage ### Bronchi * Cartilage plates * Smooth muscle layer * Mucous glands ### Bronchioles * No cartilage or glands * Simple ciliated columnar → cuboidal epithelium ### Alveoli * **Type I pneumocytes** – gas exchange * **Type II pneumocytes** – surfactant * Alveolar macrophages --- ## High-Yield Exam Pearls * Transitional epithelium is **unique to urinary tract** * Fibrocartilage **lacks perichondrium** * Peyer’s patches are characteristic of **ileum** * Kupffer cells are **liver macrophages** * Type II pneumocytes produce **surfactant** --- If you want, I can next: * ✅ Convert this into **HTML-CSS-JS single-file notes** * ✅ Add **labeled histology images** * ✅ Generate **25 image-based MCQs** * ✅ Create **printable PDF or exam charts** Just tell me 👍

Post Term Pregnancy and Fetal Macrosomia Causes Risks Diagnosis and Management
Below is a **SEO-friendly, exam-oriented, and clinically complete guide** on **Post-Term Pregnancy and Fetal Macrosomia**, written in clear **H1–H3 structure** and optimized for medical websites. --- ## **SEO Title** **Post Term Pregnancy and Fetal Macrosomia Clinical Guide 2025** --- ## **SEO Meta Description** Comprehensive medical guide on post term pregnancy and fetal macrosomia covering definition, causes, risks, diagnosis, management, induction of labor, complications, and prevention for obstetric practice and exams. --- ## **SEO Keywords** post term pregnancy, postdated pregnancy management, fetal macrosomia, macrosomia causes, post term pregnancy complications, induction of labor post term, macrosomic baby risks, shoulder dystocia, large for gestational age fetus, obstetrics clinical guide --- # **Post Term Pregnancy and Fetal Macrosomia** ## **1. Post Term Pregnancy** ### **Definition** Post term pregnancy is defined as a pregnancy that **extends beyond 42 completed weeks (≥294 days)** from the first day of the last menstrual period. --- ### **Classification** * **Late term:** 41⁰–41⁶ weeks * **Post term:** ≥42⁰ weeks --- ### **Etiology and Risk Factors** * Incorrect dating of pregnancy * Primigravida * Previous post term pregnancy * Male fetus * Maternal obesity * Genetic factors --- ### **Pathophysiology** * Progressive **placental aging and insufficiency** * Reduced uteroplacental perfusion * Oligohydramnios * Increased risk of fetal hypoxia --- ### **Maternal Complications** * Prolonged labor * Increased operative delivery * Perineal trauma * Postpartum hemorrhage * Infection --- ### **Fetal and Neonatal Complications** * Macrosomia * Meconium aspiration syndrome * Shoulder dystocia * Birth asphyxia * Stillbirth * Postmaturity syndrome (dry, peeling skin, decreased fat) --- ### **Diagnosis** * Accurate gestational age assessment (early ultrasound) * Fundal height * Ultrasound for: * Amniotic fluid index (AFI) * Estimated fetal weight * Fetal surveillance: * Non-stress test (NST) * Biophysical profile (BPP) --- ### **Management** * **41 weeks:** Begin antenatal surveillance * **≥41–42 weeks:** Induction of labor * **Cervical ripening:** Prostaglandins or Foley catheter * **Cesarean section:** If failed induction or fetal distress --- ## **2. Fetal Macrosomia** ### **Definition** Fetal macrosomia refers to a fetus with **birth weight ≥4,000 g** (some definitions use ≥4,500 g), irrespective of gestational age. --- ### **Risk Factors** * Maternal diabetes (gestational or pregestational) * Post term pregnancy * Maternal obesity * Excessive gestational weight gain * Multiparity * Previous macrosomic infant * Male fetus --- ### **Pathophysiology** * Maternal hyperglycemia → fetal hyperinsulinemia * Increased fat deposition and organ enlargement * Disproportionate growth of shoulders and trunk --- ### **Maternal Complications** * Prolonged labor * Operative vaginal delivery * Cesarean section * Postpartum hemorrhage * Genital tract injuries --- ### **Fetal and Neonatal Complications** * Shoulder dystocia * Brachial plexus injury * Clavicle fracture * Birth asphyxia * Neonatal hypoglycemia * Childhood obesity and metabolic syndrome --- ### **Diagnosis** * Clinical assessment (fundal height, Leopold maneuvers) * Ultrasound estimated fetal weight (EFW) * Limitations: ±10–15% error in late pregnancy --- ### **Management** * **Antenatal** * Optimize glycemic control * Monitor fetal growth * **Intrapartum** * Trial of labor if EFW <4,500 g (non-diabetic) * Elective cesarean if: * EFW ≥4,500 g (diabetic mother) * EFW ≥5,000 g (non-diabetic) * **Preparedness** * Anticipate shoulder dystocia * Skilled birth attendants --- ## **3. Relationship Between Post Term Pregnancy and Macrosomia** * Prolonged gestation allows continued fetal growth * Increased risk of large for gestational age fetus * Higher rates of operative delivery and birth trauma * Combined risk increases perinatal morbidity --- ## **4. Prevention Strategies** * Accurate pregnancy dating (first-trimester ultrasound) * Timely induction at 41 weeks * Optimal maternal weight and glucose control * Regular antenatal follow-up --- ## **5. Key Clinical Pearls** * Post term pregnancy significantly increases perinatal mortality * Macrosomia cannot be diagnosed with certainty antenatally * Induction at 41 weeks reduces stillbirth risk * Shoulder dystocia is the most feared complication of macrosomia --- If you want, I can next: * **Generate exam-oriented MCQs (HTML CSS JS single file)** * **Create FAQ schema for SEO** * **Generate medical illustrations** * **Convert this into a publish-ready SEO article page**
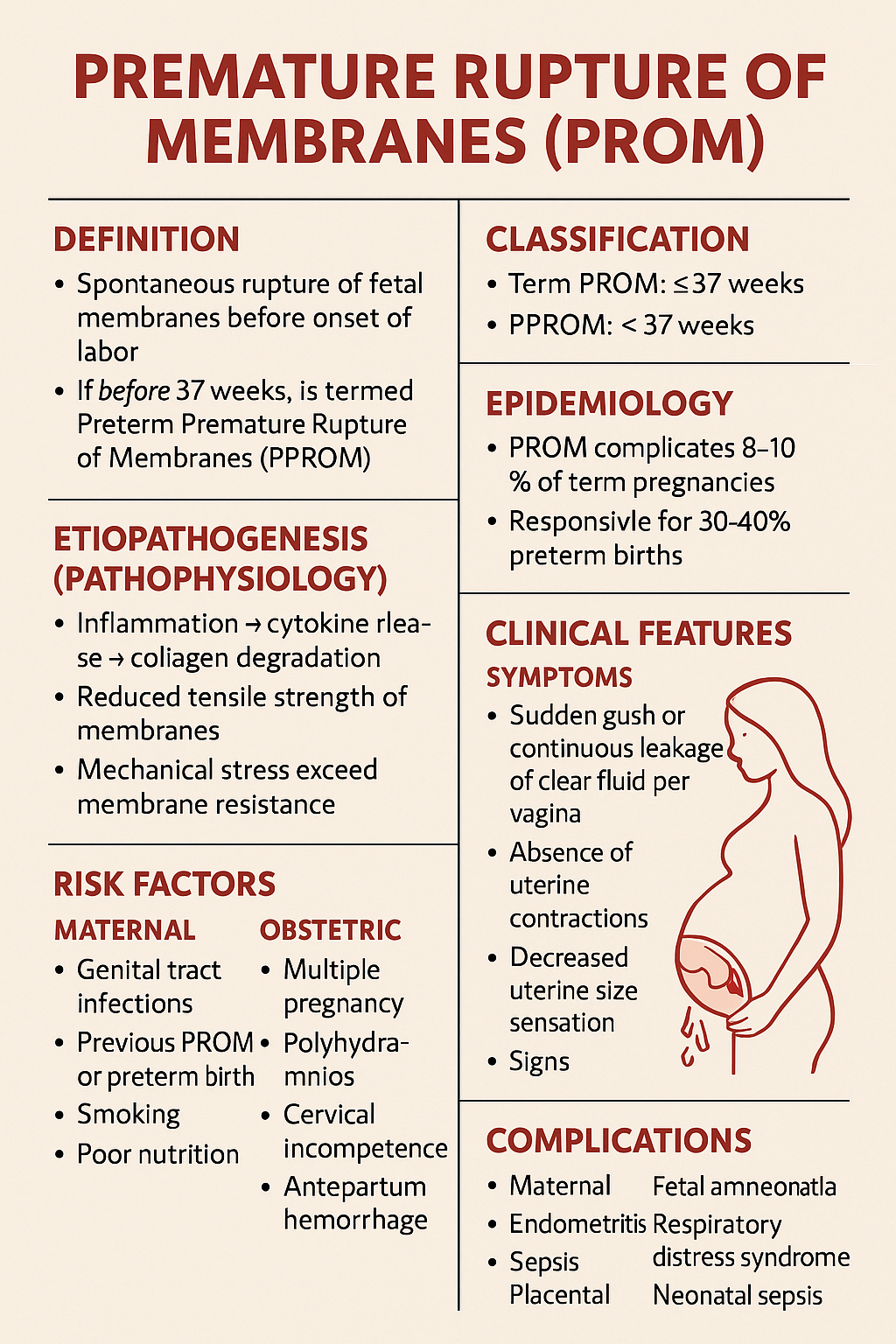
Premature Rupture of Membranes PROM – Causes Diagnosis Management and Complications
Below is a **complete, SEO-friendly, exam-oriented, single-place medical reference** on **Premature Rupture of Membranes (PROM)**, structured with clear **H1–H4 headings**, rich keywords, and clinically accurate content suitable for **medical students, clinicians, and health websites**. --- # **Premature Rupture of Membranes (PROM)** ## **Definition** **Premature Rupture of Membranes (PROM)** is defined as **spontaneous rupture of the fetal membranes before the onset of labor**, irrespective of gestational age. * If it occurs **before 37 completed weeks**, it is termed **Preterm Premature Rupture of Membranes (PPROM)**. --- ## **Classification** ### **1. Based on Gestational Age** * **Term PROM**: ≥ 37 weeks * **PPROM**: < 37 weeks ### **2. Based on Duration** * **Recent PROM**: < 18 hours * **Prolonged PROM**: ≥ 18 hours (↑ risk of infection) --- ## **Epidemiology** * PROM complicates **8–10% of term pregnancies** * PPROM accounts for **2–3% of all pregnancies** * Responsible for **30–40% of preterm births** --- ## **Etiopathogenesis (Pathophysiology)** ### **Normal Membrane Integrity** * Maintained by **collagen, elastin, and extracellular matrix** * Balance between **matrix synthesis and degradation** ### **Mechanisms Leading to PROM** * **Inflammation → cytokine release → collagen degradation** * **Reduced tensile strength of membranes** * **Mechanical stress exceeding membrane resistance** --- ## **Risk Factors** ### **Maternal Factors** * Genital tract infections (BV, UTI, STIs) * Previous PROM or preterm birth * Smoking * Poor nutrition * Low socioeconomic status ### **Obstetric Factors** * Multiple pregnancy * Polyhydramnios * Cervical incompetence * Antepartum hemorrhage ### **Iatrogenic Factors** * Amniocentesis * Cervical procedures --- ## **Clinical Features** ### **Symptoms** * Sudden **gush or continuous leakage of clear fluid per vagina** * Absence of uterine contractions initially * Decreased uterine size sensation ### **Signs** * Pooling of liquor in posterior fornix * Wet perineum * Reduced amniotic fluid volume --- ## **Diagnosis** ### **History** * Timing, amount, color, and odor of fluid * Associated fever, pain, reduced fetal movements ### **Physical Examination** * **Sterile speculum examination (preferred)** * Avoid digital vaginal examination unless in labor --- ### **Confirmatory Tests** #### **1. Bedside Tests** * **Nitrazine test**: Alkaline pH (false positives possible) * **Fern test**: Crystallization pattern on microscopy #### **2. Biochemical Tests** * PAMG-1 (AmniSure) * IGFBP-1 (Actim PROM) #### **3. Ultrasound** * Reduced Amniotic Fluid Index (AFI) * Assessment of fetal growth and presentation --- ## **Differential Diagnosis** * Urinary incontinence * Physiological vaginal discharge * Seminal fluid * Vaginal infections --- ## **Complications** ### **Maternal** * Chorioamnionitis * Endometritis * Sepsis * Placental abruption ### **Fetal and Neonatal** * Prematurity * Respiratory distress syndrome * Neonatal sepsis * Umbilical cord prolapse * Pulmonary hypoplasia (early PPROM) --- ## **Management of PROM** Management depends on **gestational age**, **infection status**, and **fetal condition**. --- ## **Management at Term PROM (≥ 37 Weeks)** ### **Principles** * Aim for **delivery** * Reduce infection risk ### **Management** * Induction of labor within **12–24 hours** * Oxytocin preferred * Prophylactic antibiotics if GBS positive --- ## **Management of PPROM (< 37 Weeks)** ### **General Principles** * Balance between **prematurity risks** and **infection risks** * Expectant management if stable --- ### **Stepwise Management** #### **1. Hospitalization and Monitoring** * Maternal vitals, fetal heart rate * Signs of infection #### **2. Antibiotic Therapy** **Indication**: Prolong latency, reduce infection **Standard Regimen** * Ampicillin IV → Amoxicillin oral * Erythromycin / Azithromycin **Benefits** * ↓ Chorioamnionitis * ↓ Neonatal sepsis * ↑ Latency period --- #### **3. Corticosteroids** **Indication**: 24–34 weeks **Drugs** * Betamethasone 12 mg IM × 2 doses (24 hours apart) **Benefits** * ↓ RDS * ↓ IVH * ↓ NEC --- #### **4. Tocolysis** * **Not routinely recommended** * Short-term use only to complete steroid course --- #### **5. Magnesium Sulfate** **Indication**: < 32 weeks **Purpose**: Fetal neuroprotection --- ### **Indications for Immediate Delivery** * Clinical chorioamnionitis * Non-reassuring fetal status * Placental abruption * Advanced labor * Severe oligohydramnios with distress --- ## **Prevention** * Screening and treatment of genital infections * Smoking cessation * Cervical cerclage in indicated cases * Adequate antenatal care --- ## **Prognosis** * **Term PROM**: Excellent with timely delivery * **PPROM**: Depends on gestational age and infection * Neonatal outcome improves significantly after **32–34 weeks** --- ## **Key Exam Points** * Avoid digital vaginal examination in PROM * Antibiotics increase latency in PPROM * Corticosteroids between 24–34 weeks * Infection = indication for delivery at any gestation --- ## **SEO Keywords (Comma-Separated)** premature rupture of membranes, prom pregnancy, pprom obstetrics, prom diagnosis management, preterm premature rupture membranes, prom complications, amniotic fluid leakage pregnancy, chorioamnionitis prom, prom treatment guidelines, pprom antibiotics steroids --- If you want, I can next: * Generate **SEO-optimized title and meta description** * Create **25 hard case-based MCQs (HTML CSS JS in one file)** * Generate **FAQ schema for SEO** * Provide **image prompts or medical diagrams**
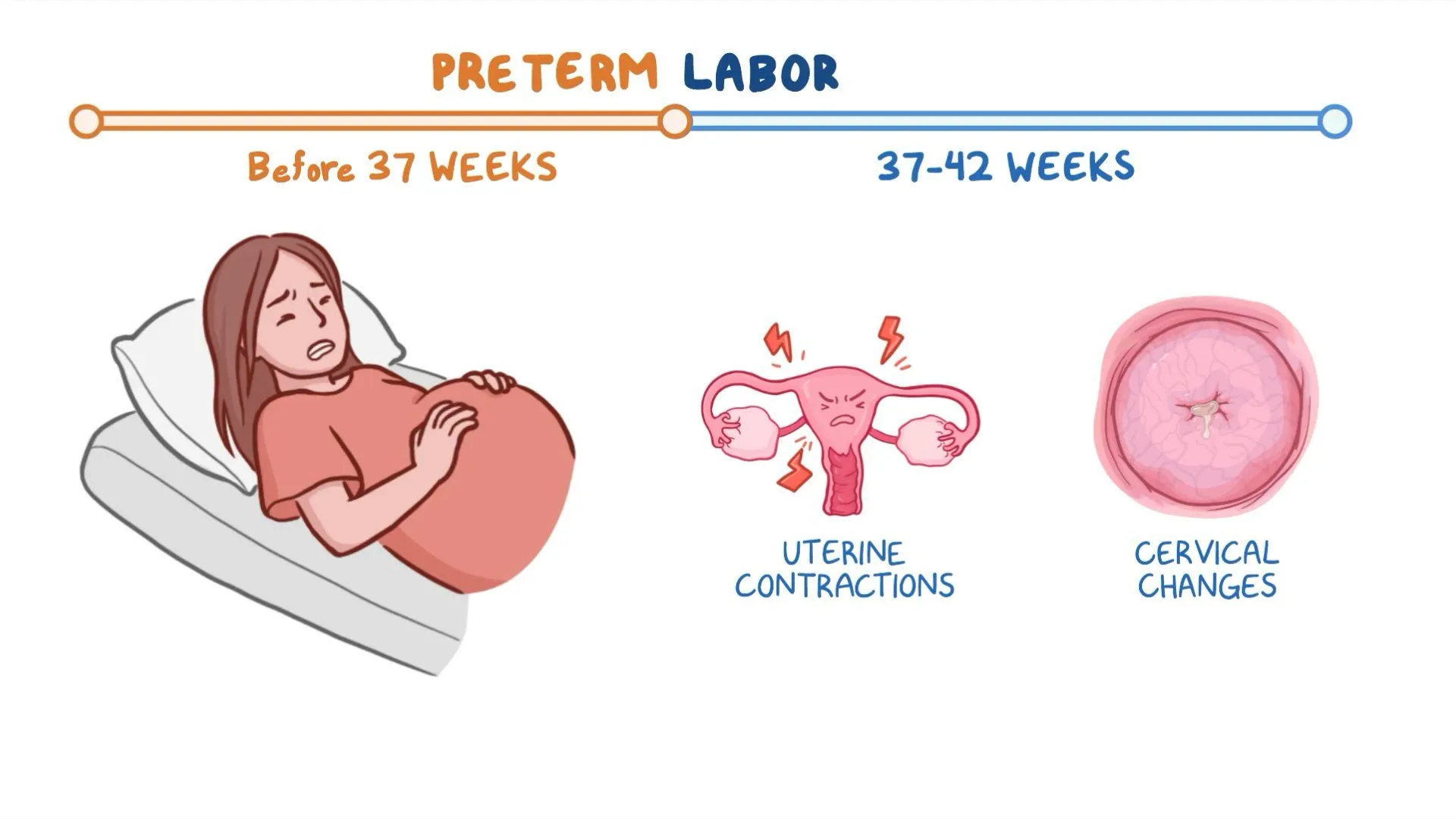
Preterm Labor: Causes, Diagnosis, Prevention and Management
Below is a **single-place, SEO-optimized, exam-ready and clinically complete reference** on **Preterm Labor**, written with clear **H1–H4 structure**, high-value keywords, and authoritative medical depth. --- # **Preterm Labor: Causes, Diagnosis, Prevention and Management** ## **Definition of Preterm Labor** Preterm labor is defined as **regular uterine contractions associated with cervical changes occurring between 20 weeks and before 37 completed weeks of gestation**, leading to preterm birth if not arrested. --- ## **Epidemiology and Importance** * Accounts for **10–12% of all pregnancies globally** * Major cause of **neonatal morbidity and mortality** * Responsible for complications such as **respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, sepsis, and long-term neurodevelopmental disability** --- ## **Pathophysiology of Preterm Labor** Preterm labor results from **premature activation of the normal labor pathway**, involving: ### **1. Uterine Activation** * Increased **oxytocin receptors** * Enhanced **prostaglandin synthesis** ### **2. Cervical Ripening** * Collagen degradation * Increased inflammatory mediators ### **3. Decidual and Membrane Activation** * Infection or inflammation leads to cytokine release * Prostaglandins stimulate uterine contractions --- ## **Etiology and Risk Factors** ### **Maternal Factors** * Previous preterm birth * Short interpregnancy interval * Extremes of maternal age * Smoking, substance abuse * Poor antenatal care * Low socioeconomic status ### **Obstetric Factors** * Multiple pregnancy * Polyhydramnios * Placental abruption * Placenta previa * Uterine anomalies ### **Infective Causes** * Urinary tract infection * Bacterial vaginosis * Chorioamnionitis ### **Fetal Factors** * Congenital anomalies * Fetal distress --- ## **Clinical Features of Preterm Labor** ### **Symptoms** * Regular uterine contractions (≥4 in 20 minutes or ≥8 in 60 minutes) * Lower abdominal or back pain * Pelvic pressure * Increased vaginal discharge * Vaginal spotting or bleeding ### **Signs** * Cervical dilation ≥1 cm * Cervical effacement ≥80% * Shortened cervical length on ultrasound --- ## **Diagnosis of Preterm Labor** ### **Clinical Assessment** * History of contractions and risk factors * Sterile speculum examination ### **Investigations** #### **1. Transvaginal Ultrasound** * Cervical length <25 mm before 24 weeks suggests high risk #### **2. Fetal Fibronectin Test** * Positive test indicates increased risk of preterm birth within 7–14 days #### **3. Laboratory Tests** * Urine analysis and culture * High vaginal swab if infection suspected * Complete blood count and CRP when indicated --- ## **Differential Diagnosis** * Braxton Hicks contractions * Urinary tract infection * Abruptio placentae * Placenta previa * Gastrointestinal causes --- ## **Management of Preterm Labor** ### **General Principles** * Confirm diagnosis * Exclude contraindications to tocolysis * Assess gestational age and fetal wellbeing --- ### **Tocolytic Therapy** Used to **delay delivery for 48 hours** to allow steroid administration. #### **1. Nifedipine (First Line)** * **Indication:** Suppression of uterine contractions * **Mechanism:** Calcium channel blockade * **Dose:** 20–30 mg orally loading, then 10–20 mg every 6–8 hours * **Adverse Effects:** Hypotension, headache, flushing * **Contraindications:** Hypotension, cardiac disease * **Monitoring:** Blood pressure, pulse * **Counselling:** Avoid sudden posture changes #### **2. Atosiban** * Oxytocin receptor antagonist * Preferred in cardiac disease #### **3. Indomethacin** * Used before 32 weeks * Risk of premature ductus arteriosus closure --- ### **Antenatal Corticosteroids** Enhance fetal lung maturity. #### **Betamethasone** * **Dose:** 12 mg IM, two doses 24 hours apart * **Benefits:** Reduces RDS, IVH, NEC, neonatal mortality * **Monitoring:** Blood glucose in diabetics --- ### **Magnesium Sulfate for Neuroprotection** * **Indication:** <32 weeks gestation * **Benefit:** Reduces cerebral palsy risk * **Adverse Effects:** Flushing, respiratory depression * **Monitoring:** Reflexes, urine output, respiratory rate --- ### **Antibiotics** * Not routinely indicated * Used when infection is confirmed or suspected --- ## **Contraindications to Tocolysis** * Intrauterine fetal demise * Lethal fetal anomalies * Severe preeclampsia or eclampsia * Chorioamnionitis * Significant vaginal bleeding --- ## **Prevention of Preterm Labor** ### **Primary Prevention** * Smoking cessation * Treatment of genital and urinary infections * Adequate antenatal care ### **Secondary Prevention** #### **Progesterone Therapy** * **Indication:** Previous preterm birth or short cervix * **Dose:** Vaginal progesterone 200 mg daily * **Mechanism:** Maintains uterine quiescence #### **Cervical Cerclage** * Indicated in cervical insufficiency * Performed between 12–14 weeks in selected cases --- ## **Complications** ### **Maternal** * Operative delivery * Infection * Postpartum hemorrhage ### **Neonatal** * Respiratory distress syndrome * Sepsis * Long-term neurodevelopmental impairment --- ## **Prognosis** * Depends on **gestational age at delivery** * Survival improves significantly after **32–34 weeks** * Early recognition and management improve outcomes --- ## **Key Clinical Pearls** * Cervical length is the **best predictor** of preterm birth * Tocolytics delay labor but **do not prevent preterm birth** * Corticosteroids are the **most effective intervention** for neonatal outcomes * Magnesium sulfate provides **neuroprotection**, not tocolysis --- ## **SEO Keywords (Comma Separated)** preterm labor, premature labor, causes of preterm labor, diagnosis of preterm labor, management of preterm labor, tocolytic therapy, antenatal corticosteroids, magnesium sulfate neuroprotection, cervical length ultrasound, fetal fibronectin test, prevention of preterm birth, progesterone therapy pregnancy --- If you want, I can **next provide**: * **25 hard case-based MCQs using HTML CSS JS (single file)** * **FAQs for SEO rich results** * **Schema-ready medical content** * **Exam-oriented summary tables** Just tell me 👍
Twin Pregnancy Complete Guide 2025 Causes Types Diagnosis Risks and Management
Below is a **complete, detailed, SEO-friendly medical article on Twin Pregnancy**, written **without images**, structured with clear **H1–H3 headings**, and optimized for **search engines and medical learning**. --- ## **SEO Title** Twin Pregnancy Complete Guide 2025 Causes Types Diagnosis Risks and Management --- ## **Meta Description** Comprehensive medical guide on twin pregnancy covering types, causes, diagnosis, antenatal care, complications, fetal surveillance, delivery planning, and prognosis for mother and babies. --- ## **SEO Keywords** twin pregnancy, multiple pregnancy twins, dichorionic twins, monochorionic twins, twin pregnancy diagnosis, twin pregnancy complications, twin pregnancy antenatal care, twin pregnancy delivery, twin pregnancy risks, twin pregnancy management, twin gestation obstetrics --- # **Twin Pregnancy** ## **1. Definition** Twin pregnancy is a type of **multiple gestation** in which **two fetuses develop simultaneously in the uterus**. It carries **higher maternal and fetal risks** compared to singleton pregnancy and requires **specialized antenatal monitoring and delivery planning**. --- ## **2. Epidemiology** * Incidence: **1 in 80–90 pregnancies** * Higher incidence with: * Assisted reproductive techniques * Advanced maternal age * Family history of twins * Multiparity --- ## **3. Classification of Twin Pregnancy** ### **3.1 Based on Zygosity** * **Dizygotic (Fraternal) Twins** * Fertilization of two separate ova * Always dichorionic and diamniotic * Most common type * **Monozygotic (Identical) Twins** * Division of a single fertilized ovum * Chorionicity depends on timing of division --- ### **3.2 Based on Chorionicity and Amnionicity** #### **3.2.1 Dichorionic Diamniotic Twins (DCDA)** * Two placentas, two amniotic sacs * Lowest complication rate * May have fused placentas #### **3.2.2 Monochorionic Diamniotic Twins (MCDA)** * One placenta, two amniotic sacs * Risk of twin-to-twin transfusion syndrome #### **3.2.3 Monochorionic Monoamniotic Twins (MCMA)** * One placenta, one amniotic sac * Highest risk * Cord entanglement common --- ## **4. Etiology and Risk Factors** * Assisted reproductive technology * Ovulation induction * Maternal age above 30 years * African ethnicity * Tall stature and high BMI * Family history of twins --- ## **5. Diagnosis of Twin Pregnancy** ### **5.1 Clinical Features** * Excessive uterine enlargement * Severe nausea and vomiting * Early perception of fetal movements * Palpation of multiple fetal parts ### **5.2 Ultrasonography** * Gold standard for diagnosis * Confirms: * Number of fetuses * Chorionicity and amnionicity * Gestational age * Placental location ### **5.3 Doppler Studies** * Used for fetal surveillance * Essential in monochorionic twins --- ## **6. Antenatal Care in Twin Pregnancy** ### **6.1 General Principles** * More frequent antenatal visits * Early booking * Multidisciplinary approach ### **6.2 Nutritional Requirements** * Increased calorie intake * Iron supplementation * Folic acid * Calcium and protein supplementation ### **6.3 Fetal Surveillance** * Serial growth scans every 2–4 weeks * Amniotic fluid assessment * Doppler velocimetry --- ## **7. Maternal Complications** * Anemia * Gestational hypertension * Preeclampsia * Gestational diabetes * Antepartum hemorrhage * Polyhydramnios * Increased operative delivery * Postpartum hemorrhage --- ## **8. Fetal Complications** * Preterm birth * Low birth weight * Intrauterine growth restriction * Congenital anomalies * Twin-to-twin transfusion syndrome * Cord accidents * Perinatal mortality --- ## **9. Special Complications in Monochorionic Twins** ### **9.1 Twin-to-Twin Transfusion Syndrome** * Unequal placental blood flow * Donor twin: growth restriction, oligohydramnios * Recipient twin: polyhydramnios, cardiac overload ### **9.2 Twin Anemia Polycythemia Sequence** * Chronic intertwin blood transfusion * Diagnosed by Doppler MCA PSV --- ## **10. Management of Twin Pregnancy** ### **10.1 Antenatal Management** * Strict blood pressure monitoring * Early detection of complications * Corticosteroids for lung maturity if preterm risk ### **10.2 Timing of Delivery** * DCDA twins: 37–38 weeks * MCDA twins: 36–37 weeks * MCMA twins: 32–34 weeks by planned cesarean ### **10.3 Mode of Delivery** * Vaginal delivery if: * First twin cephalic * No obstetric contraindications * Cesarean section if: * First twin non-cephalic * Monoamniotic twins * Obstetric complications --- ## **11. Intrapartum Care** * Continuous fetal monitoring * Availability of neonatal intensive care * Skilled obstetric and anesthetic support --- ## **12. Postpartum Care** * Active management of third stage * Monitoring for postpartum hemorrhage * Lactation support * Neonatal care for prematurity --- ## **13. Prognosis** * Improved outcomes with early diagnosis * Chorionicity is the strongest predictor * Higher neonatal morbidity compared to singleton pregnancy --- ## **14. Key Clinical Pearls** * Early determination of chorionicity is critical * Monochorionic twins require closer surveillance * Preterm birth is the most common complication * Delivery planning should be individualized --- If you want, I can next provide: **25 hard case-based MCQs (HTML CSS JS single file)**, **FAQs for SEO**, or **exam-oriented short notes** for twin pregnancy.

Placenta Accreta Spectrum: Definition, Risk Factors, Diagnosis and Management
Below is a **fully SEO-optimized, image-free, exam-ready and clinically complete** article on **Placenta Accreta Spectrum**, structured exactly in the **H1 → H2 → H3** format that search engines and medical readers prefer. --- ## **SEO Title** **Placenta Accreta Spectrum: Definition, Risk Factors, Diagnosis and Management** --- ## **SEO Meta Description** Comprehensive clinical guide on Placenta Accreta Spectrum covering definition, types, pathophysiology, risk factors, diagnosis, imaging criteria, antenatal planning, surgical management, complications, and maternal outcomes. --- ## **SEO Keywords** placenta accreta spectrum, placenta accreta, placenta increta, placenta percreta, morbidly adherent placenta, placenta accreta diagnosis, placenta accreta ultrasound signs, placenta accreta MRI, placenta accreta management, cesarean hysterectomy accreta, postpartum hemorrhage accreta --- # **Placenta Accreta Spectrum** ## **1. Definition** Placenta Accreta Spectrum (PAS) refers to a group of abnormal placental attachment disorders characterized by **pathological adherence of the placenta to the myometrium due to partial or complete absence of decidua basalis**, resulting in failure of normal placental separation after delivery. --- ## **2. Classification of Placenta Accreta Spectrum** ### **2.1 Placenta Accreta** * Chorionic villi attach **directly to the myometrium** * Most common and least severe form ### **2.2 Placenta Increta** * Chorionic villi **invade into the myometrium** ### **2.3 Placenta Percreta** * Chorionic villi **penetrate through the myometrium and serosa** * May invade adjacent organs (bladder most commonly) --- ## **3. Epidemiology** * Incidence: ~1 in 300–500 pregnancies * Rapidly increasing due to rising cesarean section rates * Major cause of **severe obstetric hemorrhage and maternal morbidity** --- ## **4. Etiopathogenesis and Pathophysiology** ### **4.1 Underlying Mechanism** * Defective or absent decidua basalis * Inadequate Nitabuch’s layer * Direct trophoblastic invasion into myometrium ### **4.2 Contributing Factors** * Prior uterine surgery leads to **endometrial scarring** * Implantation over scar tissue promotes abnormal placental adherence --- ## **5. Risk Factors** ### **5.1 Major Risk Factors** * Previous cesarean delivery (risk increases with number) * Placenta previa with prior cesarean section ### **5.2 Additional Risk Factors** * Previous myomectomy * Dilatation and curettage * Asherman syndrome * Advanced maternal age * Multiparity * Assisted reproductive techniques --- ## **6. Clinical Features** ### **6.1 Antenatal Period** * Often asymptomatic * Frequently associated with placenta previa * May present with painless antepartum bleeding ### **6.2 Intrapartum and Postpartum** * Failure of placental separation * Massive postpartum hemorrhage * Hypovolemic shock * Disseminated intravascular coagulation --- ## **7. Diagnosis** ### **7.1 Antenatal Diagnosis** Early diagnosis is critical for reducing morbidity. #### **Ultrasound (First Line)** Key grayscale and Doppler findings: * Loss of retroplacental clear zone * Thinning of myometrium (<1 mm) * Placental lacunae (“Swiss cheese” appearance) * Turbulent lacunar blood flow * Bridging vessels to bladder #### **MRI (Adjunct Tool)** Indications: * Posterior placenta * Suspected placenta percreta * Inconclusive ultrasound MRI Findings: * Dark intraplacental bands on T2 * Myometrial thinning * Uterine bulging * Direct invasion of adjacent organs --- ## **8. Differential Diagnosis** * Retained placenta * Uterine atony * Placenta previa without invasion * Uterine inversion --- ## **9. Antenatal Management and Planning** ### **9.1 Multidisciplinary Approach** * Obstetrician * Anesthesiologist * Interventional radiologist * Urologist * Blood bank support ### **9.2 Timing of Delivery** * Planned delivery at **34–36 weeks** * After corticosteroids for fetal lung maturity ### **9.3 Place of Delivery** * Tertiary care center with massive transfusion capability --- ## **10. Intrapartum Management** ### **10.1 Preferred Surgical Approach** * **Planned cesarean hysterectomy without attempting placental removal** * Placenta left in situ to prevent catastrophic hemorrhage ### **10.2 Surgical Principles** * Vertical uterine incision away from placenta * Avoid placental manipulation * Early hysterectomy following fetal delivery --- ## **11. Conservative Management Options** Reserved for highly selected cases desiring fertility. ### **11.1 Methods** * Placenta left in situ * Uterine artery embolization * Methotrexate use (controversial) ### **11.2 Risks** * Severe infection * Delayed hemorrhage * Secondary hysterectomy --- ## **12. Complications** ### **12.1 Maternal Complications** * Massive hemorrhage * Blood transfusion reactions * Bladder or ureteric injury * Sepsis * Thromboembolism * Maternal mortality ### **12.2 Fetal Complications** * Prematurity * Low birth weight * NICU admission --- ## **13. Prognosis** * Prognosis improves significantly with **antenatal diagnosis** * Planned surgery reduces maternal mortality * Future fertility usually lost with definitive surgery --- ## **14. Prevention** * Rational use of cesarean sections * Avoid unnecessary uterine curettage * Early risk stratification in placenta previa cases --- ## **15. Key Exam and Clinical Pearls** * Placenta previa with previous cesarean = **PAS until proven otherwise** * Never attempt manual placental removal if accreta suspected * Cesarean hysterectomy is the gold standard management * MRI complements ultrasound, not a replacement --- If you want, I can next provide: * **Case-based MCQs (HTML CSS JS single file)** * **PAS vs Placenta Previa comparison table** * **FAQ section for SEO** * **Schema-ready JSON-LD medical article** Just tell me 👍

Antepartum Hemorrhage (APH): Causes, Symptoms, Diagnosis, Management & Complications
--- # **Antepartum Hemorrhage (APH): Causes, Symptoms, Diagnosis, Management and Complications** --- ## **What Is Antepartum Hemorrhage?** ### **Definition of Antepartum Hemorrhage** Antepartum hemorrhage (APH) is defined as **bleeding from or into the genital tract occurring after 20 weeks of gestation and before the delivery of the fetus**. ### **Meaning of APH in Pregnancy** APH is a **major obstetric emergency** associated with significant **maternal morbidity, fetal hypoxia, preterm birth, and perinatal mortality**. --- ## **Epidemiology of Antepartum Hemorrhage** ### **Incidence of APH** * Occurs in **3–5% of all pregnancies** * Accounts for a large proportion of **emergency obstetric admissions** ### **Maternal and Perinatal Impact** * Major cause of: * Maternal anemia * Hemorrhagic shock * Stillbirth * Neonatal intensive care admission --- ## **Classification of Antepartum Hemorrhage** ### **Placental Causes of Antepartum Hemorrhage** Placental causes account for **approximately 70% of APH cases**. #### **Placenta Previa** Placenta implanted in the **lower uterine segment**, partially or completely covering the internal cervical os. #### **Placental Abruption (Abruptio Placentae)** Premature separation of a **normally situated placenta** after 20 weeks of gestation. #### **Vasa Previa** Fetal blood vessels traverse the membranes over the cervical os, unprotected by placenta or Wharton’s jelly. --- ### **Non-Placental Causes of Antepartum Hemorrhage** #### **Cervical Causes** * Cervical ectropion * Cervicitis * Cervical polyps * Cervical carcinoma #### **Vaginal Causes** * Trauma * Infection * Varicosities --- ### **Unexplained Antepartum Hemorrhage** * No identifiable cause * Occurs in **10–15%** of cases * Still associated with adverse fetal outcomes --- ## **Risk Factors for Antepartum Hemorrhage** ### **Risk Factors for Placenta Previa** * Previous cesarean section * Previous placenta previa * Multiparity * Advanced maternal age * Smoking ### **Risk Factors for Placental Abruption** * Hypertension and preeclampsia * Abdominal trauma * Smoking and cocaine use * Polyhydramnios * Sudden uterine decompression --- ## **Pathophysiology of Antepartum Hemorrhage** ### **Pathophysiology of Placenta Previa** * Placenta in lower uterine segment * Stretching and thinning cause **placental separation** * Results in **painless bleeding** ### **Pathophysiology of Placental Abruption** * Rupture of maternal vessels in decidua basalis * Formation of retroplacental hematoma * Leads to **uterine hypertonicity and fetal hypoxia** ### **Pathophysiology of Vasa Previa** * Rupture of fetal vessels * Rapid fetal blood loss * Can cause **acute fetal demise** --- ## **Clinical Features of Antepartum Hemorrhage** ### **General Symptoms of APH** * Vaginal bleeding * Reduced fetal movements * Abdominal pain (may or may not be present) --- ### **Clinical Features of Placenta Previa** * **Painless**, bright red bleeding * Recurrent episodes * Soft, non-tender uterus * Malpresentation common * Fetal heart sounds usually normal --- ### **Clinical Features of Placental Abruption** * **Painful bleeding** * Dark blood * Tense, tender uterus * Maternal shock may be disproportionate * Fetal distress or absent heart sounds --- ### **Clinical Features of Vasa Previa** * Sudden bleeding after rupture of membranes * Fetal bradycardia * Maternal condition relatively stable --- ## **Initial Assessment of Antepartum Hemorrhage** ### **Primary Survey (ABC Approach)** * Airway, Breathing, Circulation * Oxygen supplementation * Two large-bore IV cannulae * Monitor vitals and urine output ### **Important Clinical Rule** ⚠️ **Digital vaginal examination is contraindicated until placenta previa is excluded** --- ## **Investigations in Antepartum Hemorrhage** ### **Laboratory Investigations** * Complete blood count * Blood group and Rh typing * Cross-match blood * Coagulation profile (especially in abruption) * Renal function tests --- ### **Imaging in Antepartum Hemorrhage** * **Ultrasound** for placental localization * Doppler ultrasound for suspected vasa previa * Continuous CTG for fetal monitoring --- ## **Differential Diagnosis of Antepartum Hemorrhage** * Placenta previa * Placental abruption * Vasa previa * Preterm labor with show * Cervical malignancy * Uterine rupture (rare) --- ## **Management of Antepartum Hemorrhage** ### **General Management Principles** * Hospital admission * Bed rest * IV fluids * Blood transfusion if required * Anti-D immunoglobulin for Rh-negative mothers * Corticosteroids if gestation <34 weeks --- ## **Management of Placenta Previa** ### **Expectant Management** Indicated when: * Bleeding is mild * Gestation is preterm * Mother and fetus stable Includes: * Close monitoring * Avoid vaginal exams * Steroids for fetal lung maturity --- ### **Definitive Management** * **Cesarean section** is the mode of delivery for: * Major placenta previa * Heavy or recurrent bleeding * Fetal distress * Term pregnancy --- ## **Management of Placental Abruption** ### **Mild Abruption** * Conservative management * Close maternal and fetal monitoring ### **Severe Abruption** * Immediate delivery * Blood products * Correction of coagulopathy ### **Mode of Delivery** * Vaginal if fetus dead and labor progressing * Cesarean if fetus alive with distress --- ## **Management of Vasa Previa** * Emergency cesarean section * Neonatal resuscitation readiness * Planned elective cesarean if diagnosed antenatally --- ## **Complications of Antepartum Hemorrhage** ### **Maternal Complications** * Hemorrhagic shock * Disseminated intravascular coagulation (DIC) * Postpartum hemorrhage * Acute kidney injury * Maternal death --- ### **Fetal Complications** * Prematurity * Intrauterine growth restriction * Fetal hypoxia * Stillbirth * Neonatal anemia --- ## **Prevention of Antepartum Hemorrhage** ### **Preventive Strategies** * Routine antenatal ultrasound * Control of hypertension * Avoid smoking and substance abuse * Planned delivery in high-risk pregnancies --- ## **Prognosis of Antepartum Hemorrhage** ### **Maternal Prognosis** * Good with early diagnosis and prompt management ### **Fetal Prognosis** * Depends on: * Cause of APH * Gestational age * Speed of intervention --- ## **Exam-Oriented Key Points** * **Painless bleeding → Placenta previa** * **Painful bleeding + tender uterus → Abruption** * **Shock out of proportion → Concealed abruption** * **Never perform PV exam before ruling out placenta previa** --- ## **Frequently Asked Questions (SEO Boost)** ### **Is antepartum hemorrhage dangerous?** Yes. APH is a **medical emergency** that can threaten both maternal and fetal life. ### **What is the most common cause of APH?** **Placenta previa** is the most common cause. ### **Can APH be prevented?** Some causes can be reduced with proper antenatal care and risk factor control. ---
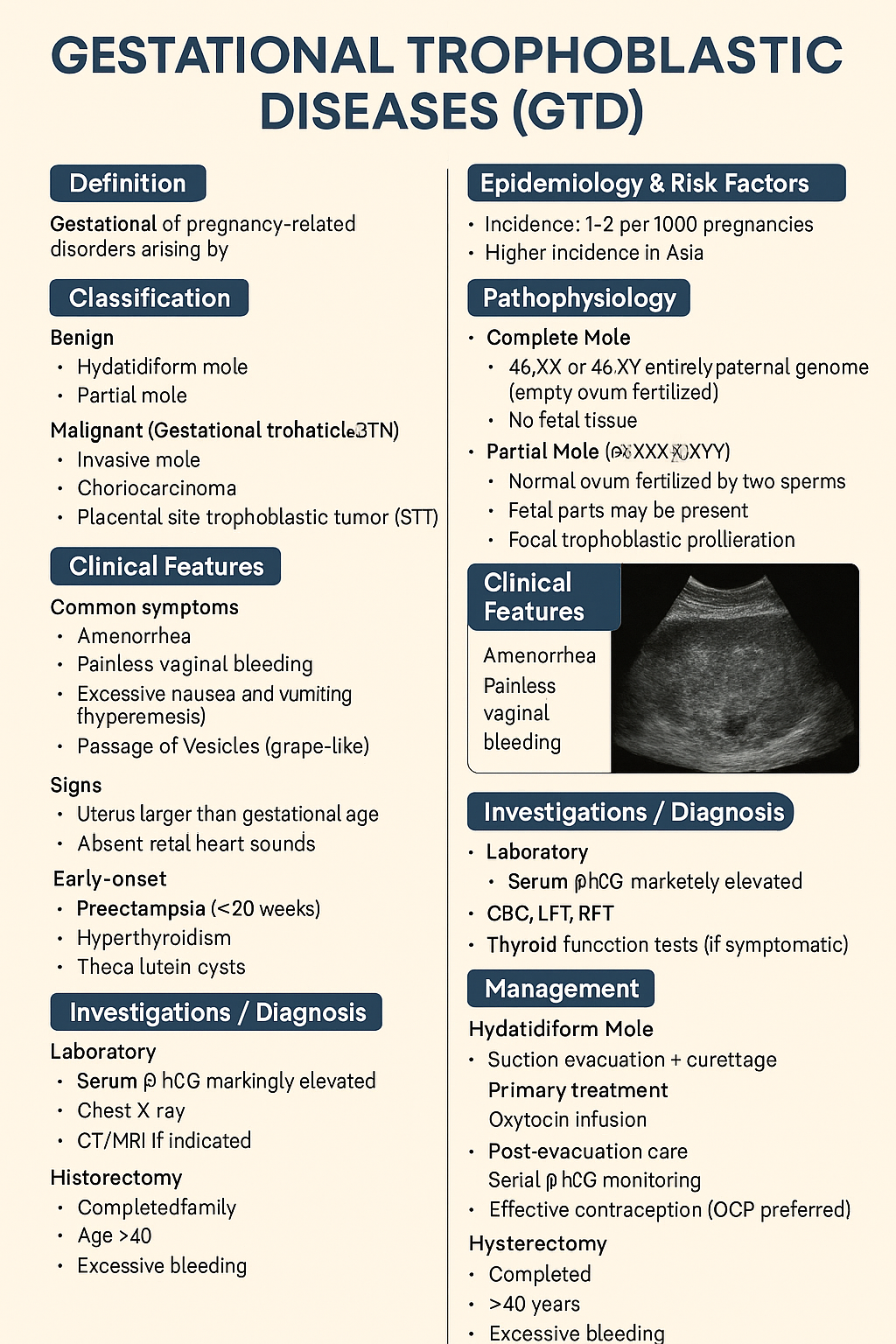
Gestational Trophoblastic Diseases (GTD): Types, Diagnosis, Management & Prognosis – Complete Medical Guide 2025
Below is a **single-place, exam-ready, clinically complete reference** on **Gestational Trophoblastic Diseases (GTD)**, structured exactly for **medical learning, exams, and clinical use**. --- # **Gestational Trophoblastic Diseases (GTD)** ## **1. Definition** Gestational trophoblastic diseases are a **spectrum of pregnancy-related disorders** arising from **abnormal proliferation of trophoblastic tissue** following conception. They range from **benign molar pregnancy** to **malignant gestational trophoblastic neoplasia (GTN)**. --- ## **2. Classification** ### **A. Benign** 1. **Hydatidiform mole** * Complete mole * Partial mole ### **B. Malignant (Gestational Trophoblastic Neoplasia – GTN)** 1. **Invasive mole** 2. **Choriocarcinoma** 3. **Placental site trophoblastic tumor (PSTT)** 4. **Epithelioid trophoblastic tumor (ETT)** --- ## **3. Epidemiology & Risk Factors** * Incidence: **1–2 per 1000 pregnancies** * Higher incidence in **Asia** * Risk factors: * Extremes of maternal age (<20, >35 years) * Previous molar pregnancy * Nutritional deficiency (low carotene, folate) * History of miscarriage --- ## **4. Pathophysiology** ### **Complete Mole** * **46,XX or 46,XY** * Entirely paternal genome (empty ovum fertilized) * No fetal tissue * Diffuse trophoblastic hyperplasia ### **Partial Mole** * **Triploid (69,XXX/XXY/XYY)** * Normal ovum fertilized by two sperms * Fetal parts may be present * Focal trophoblastic proliferation --- ## **5. Clinical Features** ### **Common Symptoms** * Amenorrhea * **Painless vaginal bleeding** * Excessive nausea and vomiting (hyperemesis) * Passage of vesicles (grape-like) ### **Signs** * Uterus larger than gestational age (complete mole) * Absent fetal heart sounds * Early-onset: * Preeclampsia (<20 weeks) * Hyperthyroidism * Theca lutein cysts --- ## **6. Investigations / Diagnosis** ### **Laboratory** * **Serum β-hCG**: markedly elevated * CBC, LFT, RFT * Thyroid function tests (if symptomatic) ### **Imaging** * **Ultrasound** * Complete mole: *“Snowstorm / cluster of grapes”* * Partial mole: gestational sac + abnormal fetus ### **Histopathology** * Confirms diagnosis after evacuation ### **Baseline Metastatic Work-up (GTN)** * Chest X-ray * CT/MRI if indicated --- ## **7. Differential Diagnosis** * Missed abortion * Ectopic pregnancy * Placenta accreta * Degenerating fibroid --- ## **8. Management** ### **A. Hydatidiform Mole** #### **Primary Treatment** * **Suction evacuation + curettage** (treatment of choice) * Oxytocin infusion after evacuation #### **Post-Evacuation Care** * Serial β-hCG monitoring * Effective contraception (OCP preferred) #### **Hysterectomy** * Completed family * Age >40 years * Excessive bleeding --- ### **B. Gestational Trophoblastic Neoplasia (GTN)** #### **Diagnosis of GTN (FIGO criteria)** * Plateauing β-hCG * Rising β-hCG * Persistent β-hCG >6 months * Histologic choriocarcinoma #### **Risk Stratification (WHO Score)** * Low risk: ≤6 * High risk: ≥7 --- ## **9. Chemotherapy** ### **Low-Risk GTN** #### **Methotrexate** * **Mechanism**: Folate antagonist → inhibits DNA synthesis * **Dose**: * 50 mg IM weekly OR * 1 mg/kg on days 1,3,5,7 + folinic acid * **Adverse effects**: * Stomatitis * Hepatotoxicity * Bone marrow suppression * **Monitoring**: * CBC * LFTs * β-hCG weekly * **Contraindications**: * Liver disease * Renal failure #### **Actinomycin-D (Alternative)** * **Mechanism**: DNA intercalation * **Dose**: 1.25 mg/m² IV every 2 weeks * **Adverse effects**: * Alopecia * Myelosuppression --- ### **High-Risk GTN** #### **EMA-CO Regimen** * **Etoposide** * **Methotrexate** * **Actinomycin-D** * **Cyclophosphamide** * **Vincristine** **Indication**: WHO score ≥7 or metastatic disease --- ## **10. Special Types** ### **Choriocarcinoma** * Highly malignant * Early hematogenous spread (lungs, brain) * Very high β-hCG * Responds excellently to chemotherapy ### **PSTT & ETT** * Low β-hCG * Less chemosensitive * **Primary treatment: hysterectomy** --- ## **11. Follow-Up** * β-hCG: * Weekly until negative ×3 * Monthly for 6–12 months * Contraception mandatory during follow-up * Next pregnancy allowed after surveillance completion --- ## **12. Prognosis** * Cure rate: * **>98% in low-risk GTN** * **>85–90% in high-risk GTN** * Future fertility usually preserved --- ## **13. Key Exam Pearls** * Early preeclampsia → think **molar pregnancy** * β-hCG is the **tumor marker** * Choriocarcinoma follows **any pregnancy** * PSTT → **hysterectomy**, not chemo * OCPs are **safe** during follow-up --- If you want next: * **SEO title + keywords** * **25 hard case-based MCQs (HTML/CSS/JS – single file)** * **Flowcharts / tables only** * **Separate GTN chemotherapy comparison** * **Image-free exam revision notes** Just tell me what you want next.
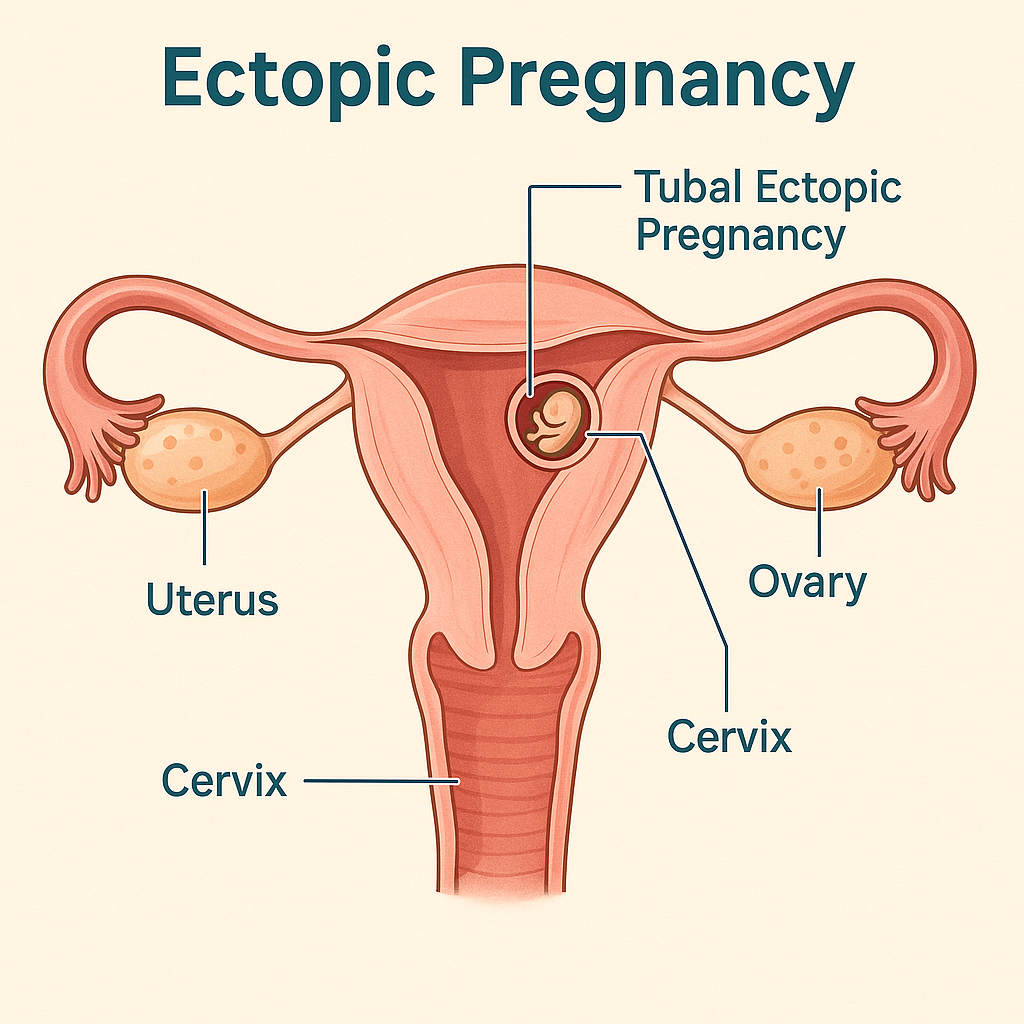
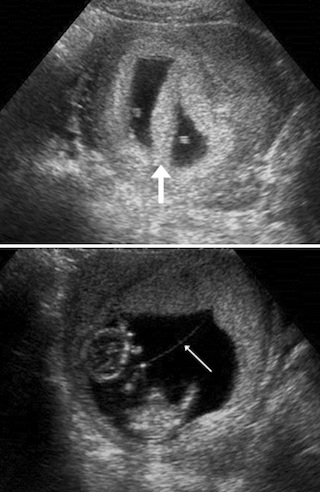
Ectopic Pregnancy: Causes, Symptoms, Diagnosis, Treatment Options & Management Guidelines (2025 Complete Guide)
Below is a **single-place, exam-ready + clinical-practice detailed reference** on **Ectopic Pregnancy**, written in the **structured pattern you prefer** and suitable for your medical hub. ✔️ **No images included** ✔️ **Includes authoritative external links** --- # **Ectopic Pregnancy – Complete Clinical & Management Guide (2025)** --- ## **1. Definition** **Ectopic pregnancy** is implantation of a fertilized ovum **outside the endometrial cavity**. > > 95% occur in the **fallopian tube**. It is a **life-threatening obstetric emergency** if ruptured. --- ## **2. Epidemiology** * Incidence: **1–2% of all pregnancies** * Leading cause of **maternal mortality in first trimester** * Rising incidence due to: * Assisted reproductive techniques (ART) * Pelvic inflammatory disease (PID) --- ## **3. Common Sites of Ectopic Pregnancy** | Site | Approx. % | | ---------------------- | ---------- | | Ampullary tube | 70% | | Isthmic tube | 12% | | Fimbrial | 11% | | Interstitial (cornual) | 2–4% | | Ovarian | <1% | | Cervical | <1% | | Caesarean scar | Increasing | --- ## **4. Pathophysiology** Normal embryo transport is impaired due to: * **Tubal damage** * **Altered tubal motility** * **Delayed ovum transport** → Implantation occurs before reaching uterus → Trophoblastic invasion erodes vessels → **Tubal rupture → hemorrhage** --- ## **5. Risk Factors** ### High-risk * Previous ectopic pregnancy * Tubal surgery / sterilization * PID (especially *Chlamydia*) * Assisted reproduction (IVF) ### Moderate risk * IUCD in situ * Smoking * Endometriosis ### No identifiable risk factor in ~50% --- ## **6. Clinical Features** ### Classical Triad (only ~50%) 1. **Amenorrhea** 2. **Lower abdominal pain** 3. **Vaginal bleeding** ### Other symptoms * Shoulder tip pain (diaphragmatic irritation) * Syncope * Dizziness ### Signs of Rupture * Hypotension * Tachycardia * Pallor * Abdominal guarding * Cervical motion tenderness * Full, tender pouch of Douglas --- ## **7. Investigations / Diagnosis** ### 1. Urine Pregnancy Test * Positive ### 2. Serum β-hCG (Quantitative) * **Discriminatory zone**: ~1500–2000 IU/L * If no intrauterine gestational sac → suspect ectopic * Plateauing or suboptimal rise (<66% in 48 hrs) ### 3. Transvaginal Ultrasound (TVS) **Suggestive findings** * Empty uterus * Adnexal mass * Tubal ring sign * Free fluid in pelvis ### 4. Culdocentesis (obsolete) ### 5. Diagnostic Laparoscopy (gold standard if uncertain) --- ## **8. Differential Diagnosis** * Threatened / incomplete abortion * Corpus luteum cyst * Acute PID * Ovarian torsion * Appendicitis * Renal colic --- ## **9. Management (Stepwise)** ### A. Expectant Management **Criteria** * Asymptomatic * β-hCG <200 IU/L and declining * No adnexal mass * Reliable follow-up --- ### B. Medical Management – **Methotrexate** #### Indications * Hemodynamically stable * Unruptured ectopic * β-hCG ≤5000 IU/L * No fetal cardiac activity #### Contraindications * Hemodynamic instability * Liver, renal disease * Breastfeeding * Blood dyscrasias #### Regimens **Single-dose** * Methotrexate **50 mg/m² IM** * Check β-hCG on day 4 & 7 **Multi-dose** * MTX 1 mg/kg on days 1,3,5,7 * Leucovorin rescue --- ### C. Surgical Management #### Indications * Ruptured ectopic * Hemodynamic instability * Failed medical treatment * Contraindications to methotrexate #### Procedures * **Salpingectomy** (preferred if tube severely damaged) * **Salpingostomy** (fertility preservation) * Laparoscopy preferred over laparotomy (if stable) --- ## **10. Special Types** ### Interstitial (Cornual) * Late rupture * Massive hemorrhage * Managed surgically ± MTX ### Cervical Ectopic * Painless bleeding * Managed with MTX, uterine artery embolization ### Caesarean Scar Pregnancy * Increasing incidence * High risk of placenta accreta * Early MTX or surgical excision --- ## **11. Complications** * Hemorrhagic shock * Infertility * Recurrent ectopic pregnancy * Maternal death (if delayed) --- ## **12. Prognosis** * Future fertility preserved in many * Recurrence risk: **10–25%** * Early diagnosis improves outcomes --- ## **13. Counselling & Follow-Up** * Avoid pregnancy for **3 months after MTX** * Early ultrasound in next pregnancy * Discuss recurrence risk * Rh-negative women → **Anti-D immunoglobulin** --- ## **14. Prevention** * Prompt treatment of PID * Smoking cessation * Safe reproductive practices * Early antenatal booking --- ## **15. Authoritative External Links** * **WHO – Ectopic Pregnancy Overview** [https://www.who.int](https://www.who.int) * **ACOG Practice Bulletin: Tubal Ectopic Pregnancy** [https://www.acog.org](https://www.acog.org) * **RCOG Green-top Guideline No. 21** [https://www.rcog.org.uk](https://www.rcog.org.uk) * **UpToDate – Ectopic Pregnancy (Clinician Reference)** [https://www.uptodate.com](https://www.uptodate.com) * **NICE Guideline: Ectopic pregnancy and miscarriage** [https://www.nice.org.uk](https://www.nice.org.uk) --- If you want, I can next: * Create **SEO title, meta description & keywords** * Convert this into **HTML (single-file)** for your site * Generate **case-based MCQs** * Add **internal links** to abortion, PID, β-hCG interpretation, or early pregnancy bleeding Just tell me 👍
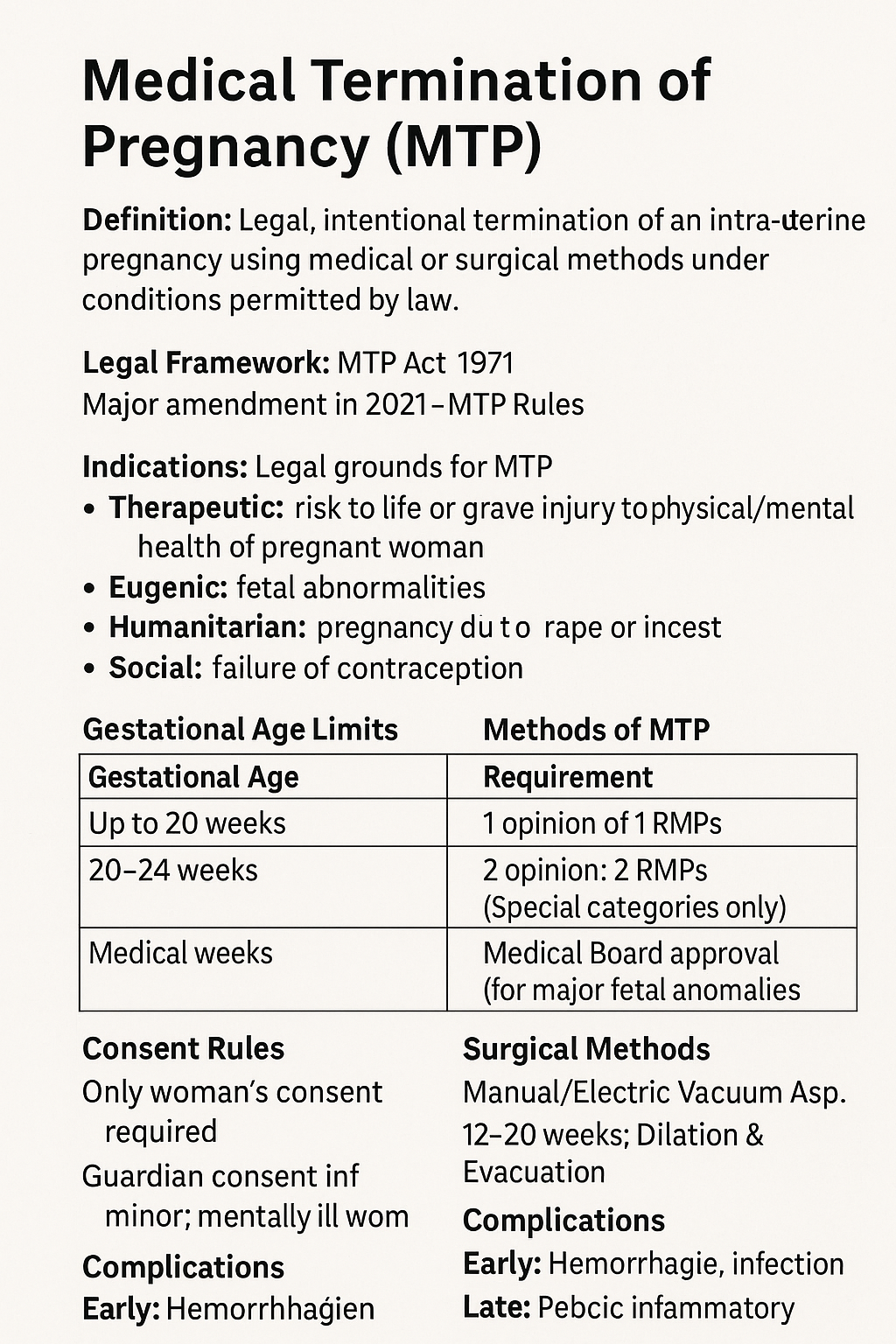
Medical Termination of Pregnancy (MTP): MTP Act, Indications, Methods, Gestational Limits & Complete Guide 2025
Below is a **complete, exam-ready, clinically exhaustive detail note on MTP (Medical Termination of Pregnancy)** with **reliable external reference links**. *(Text only, no images — as you prefer.)* --- # **Medical Termination of Pregnancy (MTP): Complete Detailed Note (India-Focused, 2025)** --- ## **1. Definition** **Medical Termination of Pregnancy (MTP)** is the **legal, intentional termination of an intra-uterine pregnancy** using **medical or surgical methods**, performed **under conditions permitted by law** to safeguard the woman’s physical, mental, and social well-being. --- ## **2. Legal Framework in India** ### **MTP Act** * **MTP Act, 1971** * **Amended in 2002** * **Major Amendment in 2021** * **MTP Rules & Regulations, 2003 & 2021** ### **Key Objectives** * Reduce **unsafe abortions** * Protect **reproductive rights** * Reduce **maternal mortality** --- ## **3. Indications for MTP (Legal Grounds)** ### **A. Therapeutic** * Risk to **life of the pregnant woman** * Grave injury to **physical or mental health** ### **B. Eugenic** * Substantial risk of **serious fetal abnormalities** * Includes **lethal anomalies, chromosomal disorders** ### **C. Humanitarian** * Pregnancy due to **rape or incest** ### **D. Social** * **Failure of contraception** (Applicable to **married & unmarried women** after 2021 amendment) --- ## **4. Gestational Age Limits & Medical Opinion** | Gestational Age | Requirement | | --------------- | ------------------------------------------------------ | | **≤ 20 weeks** | Opinion of **1 Registered Medical Practitioner (RMP)** | | **20–24 weeks** | Opinion of **2 RMPs** (Special categories only) | | **> 24 weeks** | **Medical Board approval** (for major fetal anomalies) | ### **Special Categories (20–24 weeks)** * Survivors of rape/incest * Minors * Differently-abled women * Mentally ill women * Disaster/emergency situations --- ## **5. Who Can Perform MTP?** Only a **Registered Medical Practitioner (RMP)** with: * Recognized qualification * Training in **obstetrics & gynecology** * Performed at **approved facilities only** --- ## **6. Approved Places for MTP** * Government hospitals * Approved private hospitals/clinics * Facilities meeting **MTP Rules infrastructure criteria** --- ## **7. Methods of MTP** --- ### **A. Medical Abortion** **Used up to 9 weeks (63 days)** #### **Drugs & Regimen** 1. **Mifepristone 200 mg orally** 2. After 24–48 hrs → **Misoprostol 800 mcg** * Oral / Buccal / Vaginal #### **Mechanism** * Mifepristone: Progesterone antagonist → decidual breakdown * Misoprostol: Prostaglandin → uterine contractions #### **Contraindications** * Ectopic pregnancy * Chronic adrenal failure * Long-term steroid therapy * Bleeding disorders --- ### **B. Surgical Methods** #### **Up to 12 weeks** * **Manual Vacuum Aspiration (MVA)** * **Electric Vacuum Aspiration (EVA)** #### **12–20 weeks** * **Dilation & Evacuation (D&E)** #### **>20 weeks (selected cases)** * Medical induction using **misoprostol ± mifepristone** * Rarely hysterotomy --- ## **8. Pre-Procedure Evaluation** * Confirm **intrauterine pregnancy** * Gestational age (USG) * Hb, blood group & Rh * Rule out **ectopic pregnancy** * Informed **written consent** * **Guardian consent** for minors/mentally ill women --- ## **9. Consent Rules** * **Only woman’s consent required** * **Husband’s consent NOT required** * Guardian consent mandatory for: * Minor (<18 years) * Mentally ill woman --- ## **10. Confidentiality** * Identity of woman **must not be disclosed** * Breach punishable under law --- ## **11. Post-Abortion Care** * Monitor bleeding, infection * **Anti-D immunoglobulin** for Rh-negative women * Pain management * Antibiotics if indicated * **Contraceptive counselling before discharge** --- ## **12. Complications of MTP** ### **Early** * Hemorrhage * Infection * Incomplete abortion * Uterine perforation (surgical) ### **Late** * Pelvic inflammatory disease * Asherman syndrome (rare) * Psychological distress --- ## **13. Failure of MTP** * Ongoing pregnancy * Incomplete evacuation * Requires repeat evacuation or surgery --- ## **14. MTP vs Illegal Abortion** | Legal MTP | Unsafe Abortion | | -------------- | ----------------------- | | Done by RMP | Untrained person | | Approved place | Unsafe location | | Sterile | Septic | | Low mortality | High maternal mortality | --- ## **15. Ethical & Social Aspects** * Women’s **reproductive autonomy** * Balancing fetal rights & maternal health * Public health importance --- ## **16. Important Exam & Clinical Pearls** * MTP **≠ abortion on demand** * 2021 Act includes **unmarried women** * Husband consent **not required** * Medical Board mandatory **>24 weeks** --- ## **17. Reliable External Reference Links** * **Ministry of Health & Family Welfare (India)** [https://www.mohfw.gov.in](https://www.mohfw.gov.in) * **MTP Act 1971 (Bare Act)** [https://legislative.gov.in/actsofparliamentfromtheyear/medical-termination-pregnancy-act-1971](https://legislative.gov.in/actsofparliamentfromtheyear/medical-termination-pregnancy-act-1971) * **MTP Amendment Act 2021** [https://prsindia.org/billtrack/medical-termination-of-pregnancy-amendment-bill-2020](https://prsindia.org/billtrack/medical-termination-of-pregnancy-amendment-bill-2020) * **WHO – Abortion Care Guideline** [https://www.who.int/publications/i/item/9789240039483](https://www.who.int/publications/i/item/9789240039483) * **ACOG – Induced Abortion** [https://www.acog.org/clinical/clinical-guidance/practice-bulletin](https://www.acog.org/clinical/clinical-guidance/practice-bulletin) * **FIGO Safe Abortion Guidelines** [https://www.figo.org/resources/safe-abortion](https://www.figo.org/resources/safe-abortion) --- If you want, I can next: * Add **SEO title + meta description + keywords** * Convert this into **HTML medical hub format** * Create **case-based MCQs** * Add **Indian court case highlights (landmark judgments)**
Browse by Medical Category
Explore content organized by medical specialties and systems