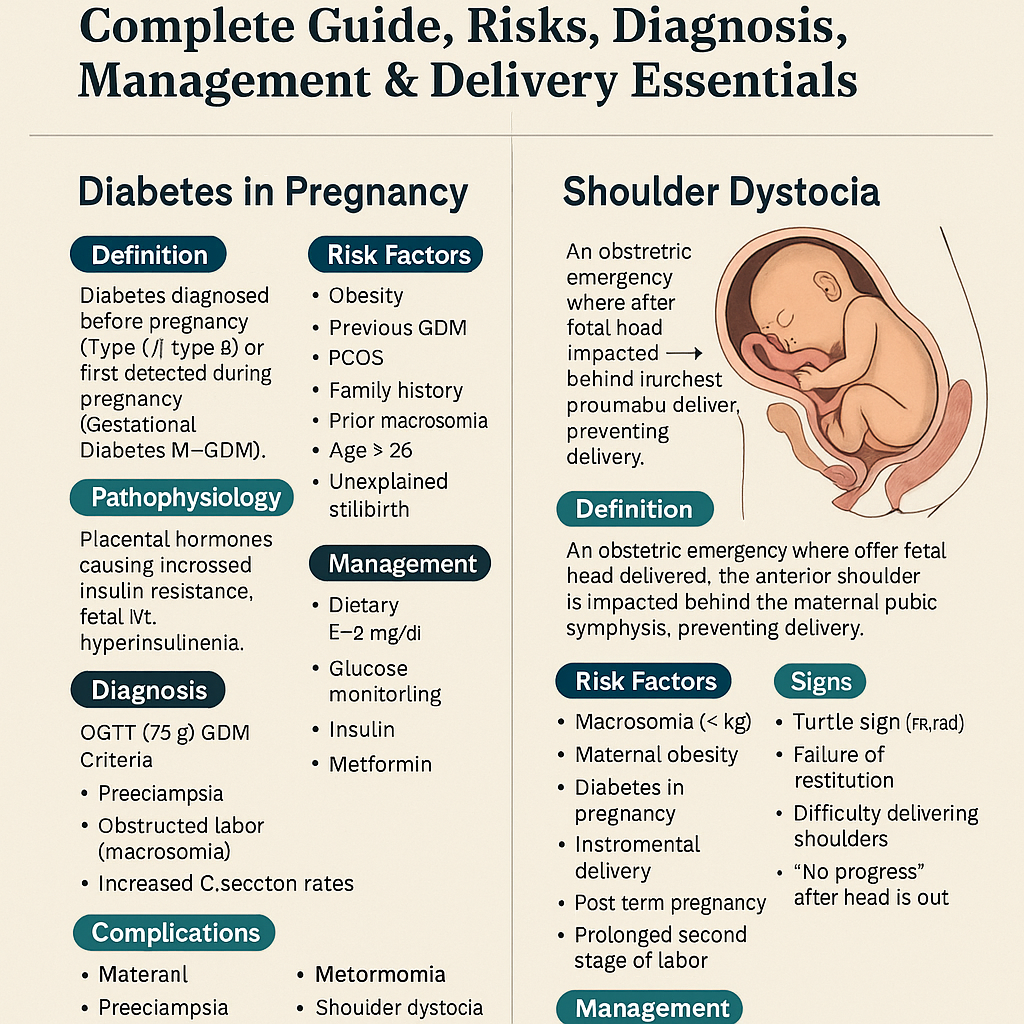
Diabetes in Pregnancy & Shoulder Dystocia – Complete Guide, Risks, Diagnosis, Management & Delivery Essentials
Explore Related Content
- Home Latest medical posts
- Sitelinks Index Complete site map
- Upload Medical Content Share clinical pearls
- More OBSTETRICS AND GYNAECOLOGY Posts Browse related content
- Reviews & Suggestions Community feedback
- Help & FAQ Upload & SEO tips
- More from this Author View all posts
- About Streamora Medical learning hub
Related Posts
Posts with similar category or tags for stronger sitelinks & internal backlinks.
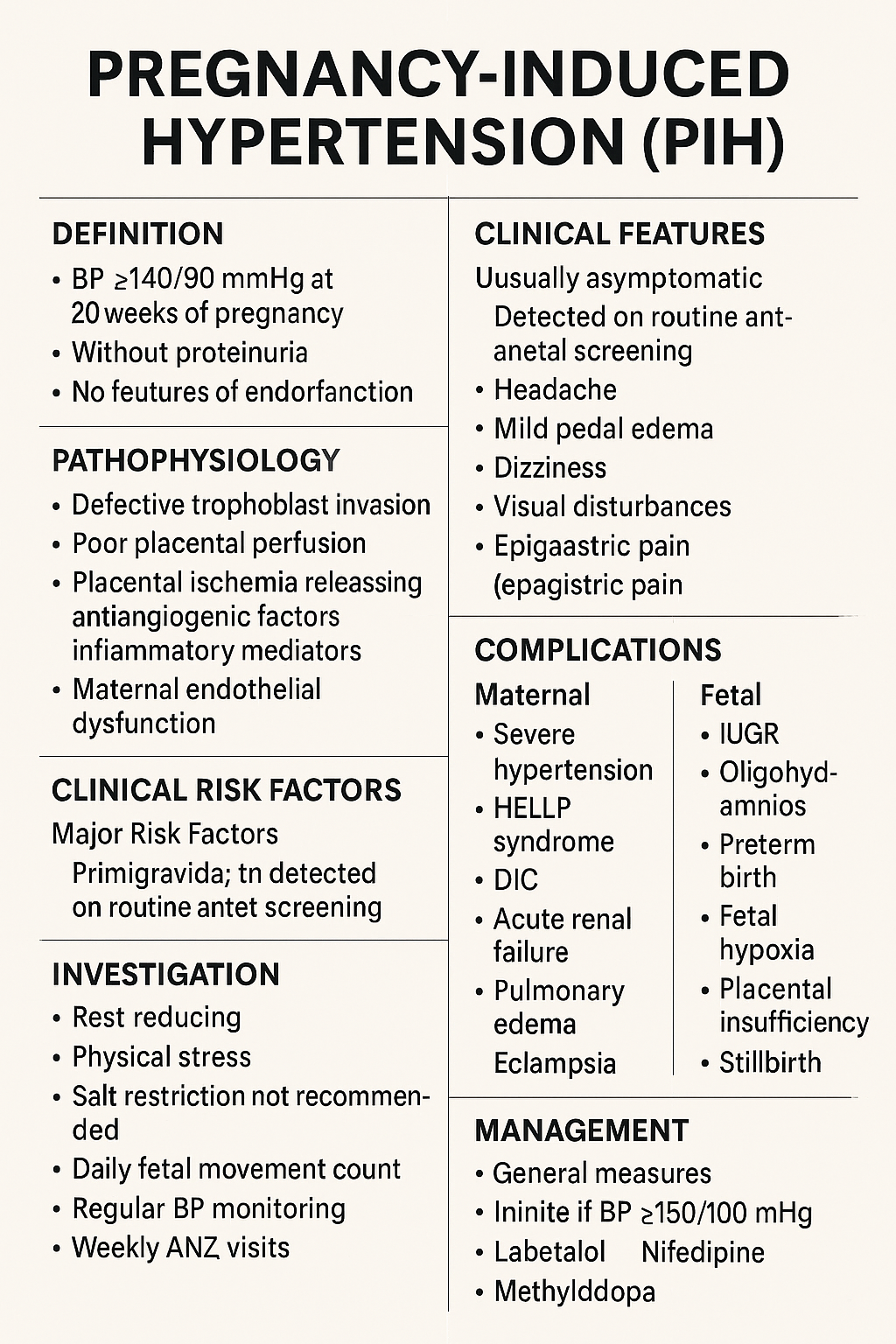
Pregnancy-Induced Hypertension (PIH): Complete Causes, Symptoms, Diagnosis & Treatment Guide
Below is a **complete, concise-but-exhaustive, exam-ready medical reference** on **Pregnancy-Induced Hypertension (PIH)**—also called **gestational hypertension**. Covers: **definition, pathophysiology, etiologies, risk factors, clinical features, investigations, differential diagnosis, complications (maternal & fetal), management (stepwise), drugs with dosing + MOA + AEs + contraindications + monitoring**, delivery timing, prevention, counseling. --- # ⭐ **PREGNANCY-INDUCED HYPERTENSION (PIH) — COMPLETE DETAILS** ! --- # **1️⃣ Definition** **PIH = Gestational Hypertension** * **BP ≥140/90 mmHg** after **20 weeks** of pregnancy * **No proteinuria** * **No features of end-organ dysfunction** * BP becomes normal within **12 weeks postpartum** --- # **2️⃣ Epidemiology** * Occurs in **6–10%** of pregnancies * More common in **primigravida**, **multiple gestation**, **teenage pregnancy**, **advanced maternal age** --- # **3️⃣ Etiology & Risk Factors** ### **Major Risk Factors** * Primigravida * Family history of PIH/Preeclampsia * Personal history of PIH * Multiple pregnancy * Molar pregnancy * Diabetes, Obesity, Chronic hypertension * Autoimmune disease * Renal disease * Thrombophilias * Advanced maternal age (>35 years) --- # **4️⃣ Pathophysiology (Simplified & Complete)**   ### **Normal Pregnancy** * Trophoblast invades → spiral arteries remodel → become wide, low-resistance → good placental perfusion. ### **PIH / Preeclampsia Spectrum** 1. **Defective trophoblastic invasion** → incomplete spiral artery remodeling 2. **Placental ischemia** → oxidative stress 3. **Release of antiangiogenic factors** (sFlt-1, endoglin) and inflammatory mediators 4. **Maternal endothelial dysfunction** → * ↑ vascular resistance * ↑ capillary permeability * Hypercoagulability 🔹 **PIH = mild endotheliopathy without proteinuria or organ dysfunction** 🔹 **Preeclampsia = PIH + proteinuria or organ dysfunction** --- # **5️⃣ Diagnostic Criteria** ### **BP Measurement** * Two readings ≥140/90 mmHg * At least 4 hours apart * After 20 weeks gestation * No proteinuria * No systemic symptoms ### **Proteinuria must be absent** * Dipstick <1+ * Spot urine protein/creatinine ratio <0.3 * 24-hr urinary protein <300 mg --- # **6️⃣ Clinical Features** ### **Usually Asymptomatic** Detected on routine antenatal screening. ### **If symptoms appear** * Headache * Mild pedal edema * Dizziness * Visual disturbances (suggest severe disease progression) * Epigastric pain (danger sign) --- # **7️⃣ Investigations (Complete Panel)** ### **Basic** * BP monitoring * Urinalysis (protein) * CBC * LFTs (AST/ALT) * Renal function test (creatinine, uric acid) ### **For progression to Preeclampsia** * Urine PCR * Peripheral smear (hemolysis) * Coagulation profile * LDH * Fundus examination ### **Fetal Evaluation** * Ultrasound for growth * AFI * Doppler velocimetry * NST / BPP --- # **8️⃣ Differential Diagnosis** * **Chronic hypertension** * **White coat hypertension** * **Preeclampsia** * **Transient hypertension of pregnancy** * **Renal disease** * **Thyroid disorders** * **Drug-induced hypertension** --- # **9️⃣ Maternal Complications** ### **If PIH progresses → Preeclampsia/Eclampsia** * Severe hypertension * HELLP syndrome * DIC * Acute renal failure * Pulmonary edema * Placental abruption * Eclampsia * Stroke / Intracranial hemorrhage --- # **🔟 Fetal Complications** * IUGR * Oligohydramnios * Preterm birth * Fetal hypoxia * Placental insufficiency * Stillbirth --- # **1️⃣1️⃣ Management (Complete Stepwise Protocol)**   --- ## **A. General Measures** * Rest, preferably left lateral * Reduce physical stress * Salt restriction **NOT** recommended severely, only normal diet * Daily fetal movement count * Regular BP monitoring * Weekly ANC visits --- ## **B. Threshold for Treatment** * **Treat if BP ≥150/100 mmHg** * For **140–149/90–99 → Monitor only**, no medication unless comorbidity --- ## **C. First-Line Antihypertensive Drugs in Pregnancy** --- # **🔹1. Labetalol (Drug of Choice)** **MOA:** α-1 & β-blocker → ↓ SVR & BP **Dose:** * Oral: 100–200 mg twice daily → up to 2,400 mg/day * IV (for severe): 20 mg bolus → 40 mg → 80 mg q10min (max 300 mg) **PK:** Hepatic metabolism **Common AEs:** Fatigue, dizziness **Serious AEs:** Bradycardia, hypotension **Contraindications:** Asthma, heart block **Monitoring:** BP, HR **Counselling:** Avoid abrupt stopping --- # **🔹2. Nifedipine (Long-acting)** **MOA:** Calcium channel blocker → vasodilation **Dose:** 30–60 mg sustained-release OD **PK:** Hepatic **Common AEs:** Headache, flushing **Serious AEs:** Hypotension **Contraindications:** Aortic stenosis **Interactions:** Magnesium sulfate ↑ hypotension risk **Monitoring:** BP **Counselling:** Do not chew CR tablets --- # **🔹3. Methyldopa (Safe in pregnancy)** **MOA:** Central α2 agonist **Dose:** 250–500 mg 2–3 times/day **PK:** Renal **Common AEs:** Sedation, depression, dry mouth **Serious AEs:** Liver dysfunction, hemolytic anemia **Monitoring:** LFTs **Counselling:** May cause drowsiness --- # ❌ **Drugs Contraindicated** * ACE inhibitors * ARBs * Atenolol * Diuretics (except pulmonary edema) --- # **1️⃣2️⃣ Management of Severe PIH** * BP ≥160/110 mmHg * Admit * IV labetalol / oral nifedipine * Evaluate for preeclampsia * Magnesium sulfate if criteria for severe features --- # **1️⃣3️⃣ Magnesium Sulfate (for progression to severe/eclampsia)** **MOA:** CNS depressant → prevents seizures by NMDA blockade **Dose (Pritchard):** * 4 g IV loading + 10 g IM (5 g each buttock) * 5 g IM q4h **Monitoring:** * Respiratory rate * Urine output (>30 ml/hr) * Patellar reflex **Toxicity:** Respiratory depression → treat with **10% calcium gluconate 10 ml IV** --- # **1️⃣4️⃣ Delivery Timing** | Condition | Timing | | ------------------------------------------------ | ------------------------- | | **PIH (controlled)** | **37 weeks** | | **Severe PIH** | 34 weeks (after steroids) | | **Uncontrolled BP, fetal compromise, abruption** | Immediate delivery | --- # **1️⃣5️⃣ Intrapartum Care** * Continuous fetal monitoring * Keep BP <160/110 * Avoid fluid overload * Anesthesia: regional preferred unless contraindicated --- # **1️⃣6️⃣ Postpartum Care** * Continue antihypertensives * Monitor BP for **12 weeks** * If persistent → chronic hypertension --- # **1️⃣7️⃣ Prevention of PIH** * Low-dose **Aspirin 75–150 mg at bedtime** from **12–16 weeks** in high-risk women * Calcium supplementation (1–1.5 g/day) in low-calcium diets * Weight control * Control comorbidities --- # **1️⃣8️⃣ Patient Counseling Points** * Regular BP monitoring * Danger signs: headache, visual symptoms, epigastric pain * Adherence to medications * Fetal kick count * Importance of follow-up * No self-discontinuation of drugs --- # ⭐ If you want, I can also provide: ✅ **Flowchart of PIH diagnosis** ✅ **Flowchart of management** ✅ **HTML/CSS/JS quiz (hard, case-based)** ✅ **SEO title + description + keywords** ✅ **Image generation** Just tell me what you need next!

Post Term Pregnancy and Fetal Macrosomia Causes Risks Diagnosis and Management
Below is a **SEO-friendly, exam-oriented, and clinically complete guide** on **Post-Term Pregnancy and Fetal Macrosomia**, written in clear **H1–H3 structure** and optimized for medical websites. --- ## **SEO Title** **Post Term Pregnancy and Fetal Macrosomia Clinical Guide 2025** --- ## **SEO Meta Description** Comprehensive medical guide on post term pregnancy and fetal macrosomia covering definition, causes, risks, diagnosis, management, induction of labor, complications, and prevention for obstetric practice and exams. --- ## **SEO Keywords** post term pregnancy, postdated pregnancy management, fetal macrosomia, macrosomia causes, post term pregnancy complications, induction of labor post term, macrosomic baby risks, shoulder dystocia, large for gestational age fetus, obstetrics clinical guide --- # **Post Term Pregnancy and Fetal Macrosomia** ## **1. Post Term Pregnancy** ### **Definition** Post term pregnancy is defined as a pregnancy that **extends beyond 42 completed weeks (≥294 days)** from the first day of the last menstrual period. --- ### **Classification** * **Late term:** 41⁰–41⁶ weeks * **Post term:** ≥42⁰ weeks --- ### **Etiology and Risk Factors** * Incorrect dating of pregnancy * Primigravida * Previous post term pregnancy * Male fetus * Maternal obesity * Genetic factors --- ### **Pathophysiology** * Progressive **placental aging and insufficiency** * Reduced uteroplacental perfusion * Oligohydramnios * Increased risk of fetal hypoxia --- ### **Maternal Complications** * Prolonged labor * Increased operative delivery * Perineal trauma * Postpartum hemorrhage * Infection --- ### **Fetal and Neonatal Complications** * Macrosomia * Meconium aspiration syndrome * Shoulder dystocia * Birth asphyxia * Stillbirth * Postmaturity syndrome (dry, peeling skin, decreased fat) --- ### **Diagnosis** * Accurate gestational age assessment (early ultrasound) * Fundal height * Ultrasound for: * Amniotic fluid index (AFI) * Estimated fetal weight * Fetal surveillance: * Non-stress test (NST) * Biophysical profile (BPP) --- ### **Management** * **41 weeks:** Begin antenatal surveillance * **≥41–42 weeks:** Induction of labor * **Cervical ripening:** Prostaglandins or Foley catheter * **Cesarean section:** If failed induction or fetal distress --- ## **2. Fetal Macrosomia** ### **Definition** Fetal macrosomia refers to a fetus with **birth weight ≥4,000 g** (some definitions use ≥4,500 g), irrespective of gestational age. --- ### **Risk Factors** * Maternal diabetes (gestational or pregestational) * Post term pregnancy * Maternal obesity * Excessive gestational weight gain * Multiparity * Previous macrosomic infant * Male fetus --- ### **Pathophysiology** * Maternal hyperglycemia → fetal hyperinsulinemia * Increased fat deposition and organ enlargement * Disproportionate growth of shoulders and trunk --- ### **Maternal Complications** * Prolonged labor * Operative vaginal delivery * Cesarean section * Postpartum hemorrhage * Genital tract injuries --- ### **Fetal and Neonatal Complications** * Shoulder dystocia * Brachial plexus injury * Clavicle fracture * Birth asphyxia * Neonatal hypoglycemia * Childhood obesity and metabolic syndrome --- ### **Diagnosis** * Clinical assessment (fundal height, Leopold maneuvers) * Ultrasound estimated fetal weight (EFW) * Limitations: ±10–15% error in late pregnancy --- ### **Management** * **Antenatal** * Optimize glycemic control * Monitor fetal growth * **Intrapartum** * Trial of labor if EFW <4,500 g (non-diabetic) * Elective cesarean if: * EFW ≥4,500 g (diabetic mother) * EFW ≥5,000 g (non-diabetic) * **Preparedness** * Anticipate shoulder dystocia * Skilled birth attendants --- ## **3. Relationship Between Post Term Pregnancy and Macrosomia** * Prolonged gestation allows continued fetal growth * Increased risk of large for gestational age fetus * Higher rates of operative delivery and birth trauma * Combined risk increases perinatal morbidity --- ## **4. Prevention Strategies** * Accurate pregnancy dating (first-trimester ultrasound) * Timely induction at 41 weeks * Optimal maternal weight and glucose control * Regular antenatal follow-up --- ## **5. Key Clinical Pearls** * Post term pregnancy significantly increases perinatal mortality * Macrosomia cannot be diagnosed with certainty antenatally * Induction at 41 weeks reduces stillbirth risk * Shoulder dystocia is the most feared complication of macrosomia --- If you want, I can next: * **Generate exam-oriented MCQs (HTML CSS JS single file)** * **Create FAQ schema for SEO** * **Generate medical illustrations** * **Convert this into a publish-ready SEO article page**
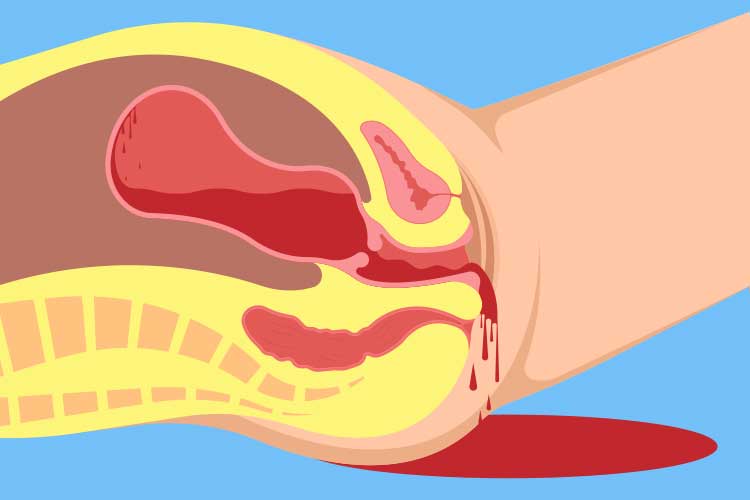
Postpartum Hemorrhage Causes Diagnosis and Management
## **Postpartum Hemorrhage Clinical Guide Causes Diagnosis and Management** ### **Definition** **Postpartum hemorrhage (PPH)** is excessive bleeding after childbirth. * **Primary (early) PPH:** ≥500 mL after vaginal delivery or ≥1000 mL after cesarean section within **24 hours** * **Secondary (late) PPH:** Excessive bleeding from **24 hours to 6 weeks** postpartum --- ## **Epidemiology and Importance** * Leading cause of **maternal mortality worldwide** * Rapid onset and progression require **early recognition and protocol-based management** --- ## **Pathophysiology** Normal hemostasis after delivery depends on **uterine contraction** compressing spiral arteries. Failure of contraction or disruption of clotting leads to uncontrolled bleeding. --- ## **Causes – “4 Ts” Framework** 1. **Tone (most common – uterine atony)** * Overdistended uterus (multiple pregnancy, polyhydramnios, macrosomia) * Prolonged or precipitous labor * Chorioamnionitis 2. **Trauma** * Cervical, vaginal, perineal tears * Uterine rupture * Hematomas 3. **Tissue** * Retained placental tissue * Placenta accreta spectrum 4. **Thrombin** * Coagulopathies (DIC, severe preeclampsia, HELLP, anticoagulant use) --- ## **Risk Factors** * Previous PPH * Operative delivery * Induction or augmentation of labor * Anemia * Placenta previa or accreta --- ## **Clinical Features** * Excessive vaginal bleeding * Boggy or enlarged uterus * Signs of hypovolemia: tachycardia, hypotension, pallor, altered sensorium * Reduced urine output --- ## **Initial Assessment and Diagnosis** **Diagnosis is clinical and urgent** * Quantify blood loss (visual + weighing) * Assess uterine tone * Inspect birth canal * Evaluate placenta completeness ### **Investigations (do not delay treatment)** * CBC (Hb, platelets) * Blood group and cross-match * Coagulation profile (PT, aPTT, fibrinogen) * ABG if severe shock --- ## **Management – Stepwise Approach** ### **Immediate Resuscitation** * Call for help * Airway and oxygen * Two wide-bore IV lines * Crystalloids followed by blood products (1:1:1 PRBC:plasma:platelets if massive) --- ## **Uterotonic Drugs (Cornerstone of Treatment)** ### **1. Oxytocin** * **Indication:** First-line for uterine atony * **Mechanism:** Stimulates uterine smooth muscle contraction * **Dose:** * IV infusion: 10–40 IU in 1 L NS/RL * IM: 10 IU * **Adverse effects:** Hypotension (rapid IV), water intoxication * **Contraindications:** None significant in PPH * **Monitoring:** Uterine tone, vitals * **Counselling:** First-line and safe --- ### **2. Methylergometrine** * **Mechanism:** Sustained uterine contraction via alpha-adrenergic stimulation * **Dose:** 0.2 mg IM (may repeat) * **Adverse effects:** Hypertension, nausea * **Contraindications:** Hypertension, preeclampsia, cardiac disease * **Monitoring:** Blood pressure --- ### **3. Carboprost (15-methyl PGF2α)** * **Mechanism:** Prostaglandin-induced myometrial contraction * **Dose:** 250 µg IM every 15–90 min (max 8 doses) * **Adverse effects:** Bronchospasm, diarrhea, fever * **Contraindications:** Asthma * **Monitoring:** Respiratory status --- ### **4. Misoprostol** * **Mechanism:** Prostaglandin E1 analog * **Dose:** 800–1000 µg rectal or sublingual * **Adverse effects:** Fever, shivering * **Use:** Low-resource settings --- ### **5. Tranexamic Acid** * **Indication:** All PPH within 3 hours of onset * **Mechanism:** Inhibits fibrinolysis * **Dose:** 1 g IV over 10 min (repeat once if bleeding continues) * **Adverse effects:** Rare thrombosis * **Contraindications:** Active thromboembolic disease * **Monitoring:** Renal function if repeated * **Counselling:** Reduces mortality when given early --- ## **Mechanical and Surgical Measures** ### **Mechanical** * Bimanual uterine massage * Uterine balloon tamponade (Bakri balloon) * Uterine packing ### **Surgical** * Uterine compression sutures (B-Lynch) * Uterine artery ligation * Internal iliac artery ligation * **Hysterectomy** (life-saving last resort) --- ## **Management by Cause** * **Atony:** Uterotonics → balloon → surgery * **Trauma:** Immediate repair of tears * **Tissue:** Manual removal, curettage * **Thrombin:** Correct coagulopathy with blood products --- ## **Secondary Postpartum Hemorrhage** **Causes** * Retained products * Subinvolution of uterus * Endometritis **Management** * Antibiotics * Uterotonics * Ultrasound-guided evacuation if indicated --- ## **Complications** * Hypovolemic shock * Acute kidney injury * DIC * Sheehan syndrome * Maternal death --- ## **Prevention** * Active management of third stage of labor * Antenatal anemia correction * Risk stratification and preparedness --- ## **Prognosis** Excellent with early recognition and protocol-driven care; delays increase morbidity and mortality. --- ## **SEO Meta Data** **SEO Title:** Postpartum Hemorrhage Causes Diagnosis and Management **Meta Description:** Comprehensive clinical guide on postpartum hemorrhage covering causes, diagnosis, stepwise management, uterotonic drugs, surgical options, prevention, and complications. **SEO Keywords (comma separated):** postpartum hemorrhage, PPH management, uterine atony, causes of PPH, tranexamic acid PPH, obstetric emergency, maternal hemorrhage, third stage labor complications --- ## **Frequently Asked Questions** **What is the most common cause of postpartum hemorrhage?** Uterine atony. **When should tranexamic acid be given in PPH?** Within 3 hours of onset of bleeding. **What is the first-line drug for PPH?** Oxytocin. **When is hysterectomy indicated in PPH?** When bleeding is uncontrollable and life-threatening despite conservative measures. **Can PPH occur after 24 hours?** Yes, it is termed secondary postpartum hemorrhage. --- If you want, I can **convert this into a CMS-ready HTML or PHP page**, **add FAQ schema and Article schema**, or **create MCQs and case-based questions** for your medical knowledge platform.
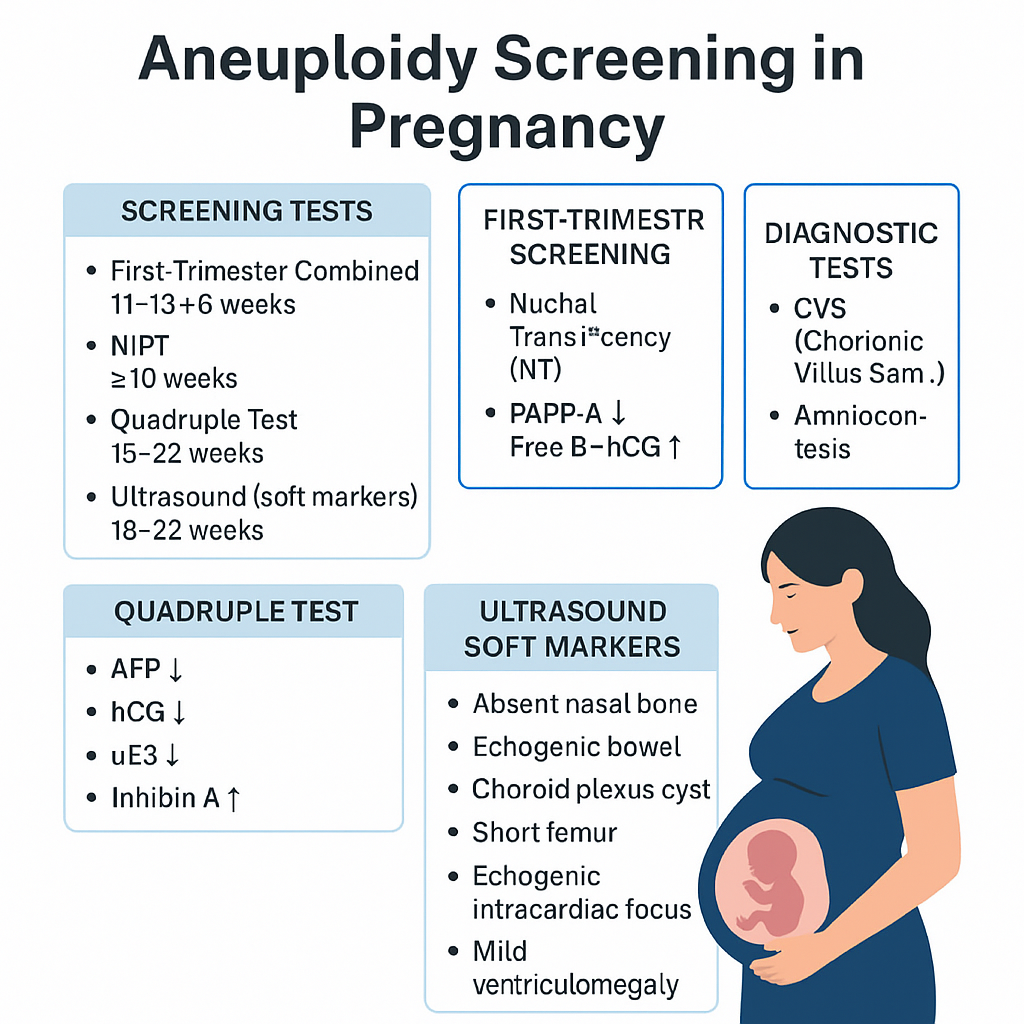
Aneuploidy Screening in Pregnancy: First Trimester, Quadruple Test, NIPT & Soft Markers | Complete Guide 2025
--- # ⭐ **Aneuploidy Screening in Pregnancy — Complete Obstetric Guide** Aneuploidy = **abnormal number of chromosomes** (most clinically relevant: **Trisomy 21, 18, 13**, Turner syndrome). Goal of screening = **identify pregnancies at increased risk** early enough to offer **diagnostic testing**. --- # **1. Why Aneuploidy Occurs (Basic Pathophysiology)** * **Meiotic nondisjunction** → failure of homologous chromosomes/sister chromatids to separate. * **Common in maternal meiosis I** (age-related). * **Trisomy 21 risk increases exponentially with maternal age**. * Mosaicism occurs if nondisjunction happens post-zygotically. --- # **2. High-Risk Factors** * Advanced maternal age (≥35 yrs). * Previous pregnancy with aneuploidy. * Parental balanced translocation (esp. Robertsonian). * Abnormal ultrasound markers (NT ↑, absent nasal bone, echogenic bowel, cardiac defects). * Abnormal biochemical screening results. --- # **3. Overview of Screening Timeline** | Gestation | Test | | ------------------- | ------------------------------------------------------------- | | **11–13+6 weeks** | First-trimester combined screening (NT + PAPP-A + free β-hCG) | | **10 weeks onward** | NIPT / cfDNA (highest accuracy) | | **15–22 weeks** | Second-trimester quadruple test | | **18–22 weeks** | Targeted anomaly scan (soft markers) | **Screening ≠ diagnosis.** Diagnostic tests = **CVS (10–13 wks)**, **Amniocentesis (≥15 wks)**, **FISH/karyotype/microarray**. --- # **4. First-Trimester Screening (11–13+6 Weeks)** ## **Components** 1. **Nuchal translucency (NT):** * Measured at CRL 45–84 mm * **NT >3.5 mm = major risk marker** * Increased NT → Trisomy 21/18/13, cardiac defects, Noonan syndrome, skeletal dysplasias 2. **Biochemical markers:** * **PAPP-A ↓**: Trisomy 21/18, placental insufficiency * **Free β-hCG ↑**: Trisomy 21 * **Free β-hCG ↓**: Trisomy 18/13 ## **Detection rate:** ~85–90% for T21 when combined. --- # **5. NIPT / cfDNA (Non-Invasive Prenatal Testing)** * Can be done **from 10 weeks onward**. * Analyzes **cell-free fetal DNA** in maternal blood. * **Most accurate screening test**. ## **Detects** * **Trisomy 21, 18, 13** * **Sex chromosome aneuploidies** (Turner, Klinefelter) * Microdeletions (low PPV, not recommended routinely) ## **Not diagnostic**, but: * **Sensitivity**: * T21 ≈ 99% * T18 ≈ 97–98% * T13 ≈ 92% ## **Causes of false results** * Confined placental mosaicism * Vanishing twin * Maternal malignancy * Low fetal fraction (<4%) --- # **6. Second-Trimester Quadruple Test (15–22 Weeks)** Markers: * **AFP** * **hCG** * **uE3 (unconjugated estriol)** * **Inhibin-A** ## **Patterns** ### **Trisomy 21** * **AFP ↓** * **uE3 ↓** * **hCG ↑** * **Inhibin-A ↑** ### **Trisomy 18** * **AFP ↓** * **uE3 ↓** * **hCG ↓** * **Inhibin-A normal** ### **Open neural tube defects** * **AFP ↑↑** Detection rate: * **~75% for T21** --- # **7. Ultrasound Soft Markers (18–22 Weeks)** ### **Major structural markers** * Cardiac defects (AV canal) → T21 * Holoprosencephaly → T13 * Omphalocele → T18 * Diaphragmatic hernia * Renal anomalies ### **Soft markers (non-structural)** | Marker | Association | | -------------------------------------- | --------------- | | **Absent nasal bone** | T21 | | **Echogenic intracardiac focus (EIF)** | Mild ↑ T21 risk | | **Echogenic bowel** | T21, CMV, CF | | **Short femur/humerus** | T21 | | **Choroid plexus cyst** | T18 | | **Single umbilical artery** | T18, T13 | | **Mild ventriculomegaly** | Aneuploidy risk | Soft markers **modify risk**, not diagnostic. --- # **8. Integrated & Sequential Screening** ### **Integrated test** * Combines first-trimester + second-trimester results * Highest combined detection before NIPT * Detection: **~94–95%**, but results available only in 2nd trimester ### **Sequential screening** * If first-trimester is high-risk → offer NIPT/CVS * If low-risk → continue with second trimester screening * More practical than integrated approach --- # **9. Diagnostic Tests (When Screening Is Positive)** ## **Chorionic Villus Sampling (CVS)** * **10–13+6 weeks** * Transcervical or transabdominal * Results: karyotype, microarray * Miscarriage risk: **~0.2–0.3%** ## **Amniocentesis** * **≥15 weeks** * Lower miscarriage risk: **0.1–0.2%** ## **Rapid tests** * **FISH** (24–48 hrs): detects T21, T18, T13 * **Microarray**: detects microdeletions/duplications --- # **10. Combined Detection Performance** | Test | Detection rate for T21 | | ------------------------ | ---------------------- | | First trimester combined | 85–90% | | Quadruple test | 75% | | Integrated screening | 94–95% | | **NIPT** | **>99%** | NIPT is **preferred**, especially for high-risk pregnancies. --- # **11. When to Offer NIPT (Indications)** * Maternal age ≥35 yrs * Previous trisomy pregnancy * Abnormal ultrasound markers * Positive biochemical screen * IVF pregnancies (optional but recommended) * Parental chromosomal rearrangement (screening may be inadequate → offer diagnostic test) --- # **12. Management Algorithm (Simplified)** ### **STEP 1: First antenatal visit** * Counsel regarding available screening methods * Offer **NIPT** to all (optimal) ### **STEP 2: If NT scan & biochemistry done** * **High-risk → NIPT or CVS** * **Intermediate risk → NIPT** * **Low risk → routine care** ### **STEP 3: Anomaly scan** * If any major structural abnormality → **Diagnostic test (CVS/Amniocentesis)** irrespective of NIPT result ### **STEP 4: If NIPT positive** * **Never terminate pregnancy based on NIPT alone** * Perform **confirmatory CVS/Amniocentesis** --- # **13. Counseling Points** * Screening ≠ diagnosis * Explain detection rates and false positives * Invasive diagnostic tests carry small miscarriage risks * A normal screen reduces but **does not eliminate** risk * Final decision is patient-centered --- # **14. Key Exam High-Yield Points** * **Most sensitive screening test:** NIPT * **Earliest diagnostic test:** CVS * **Best time for NT scan:** 11–13+6 weeks * **AFP ↑:** NTD, abdominal wall defects, incorrect dating * **AFP ↓ + hCG ↑ + uE3 ↓:** Trisomy 21 * **Choroid plexus cyst:** Trisomy 18 marker * **Absent nasal bone:** Down syndrome strongest soft marker * **Echogenic bowel:** Trisomy 21, CMV, CF ---
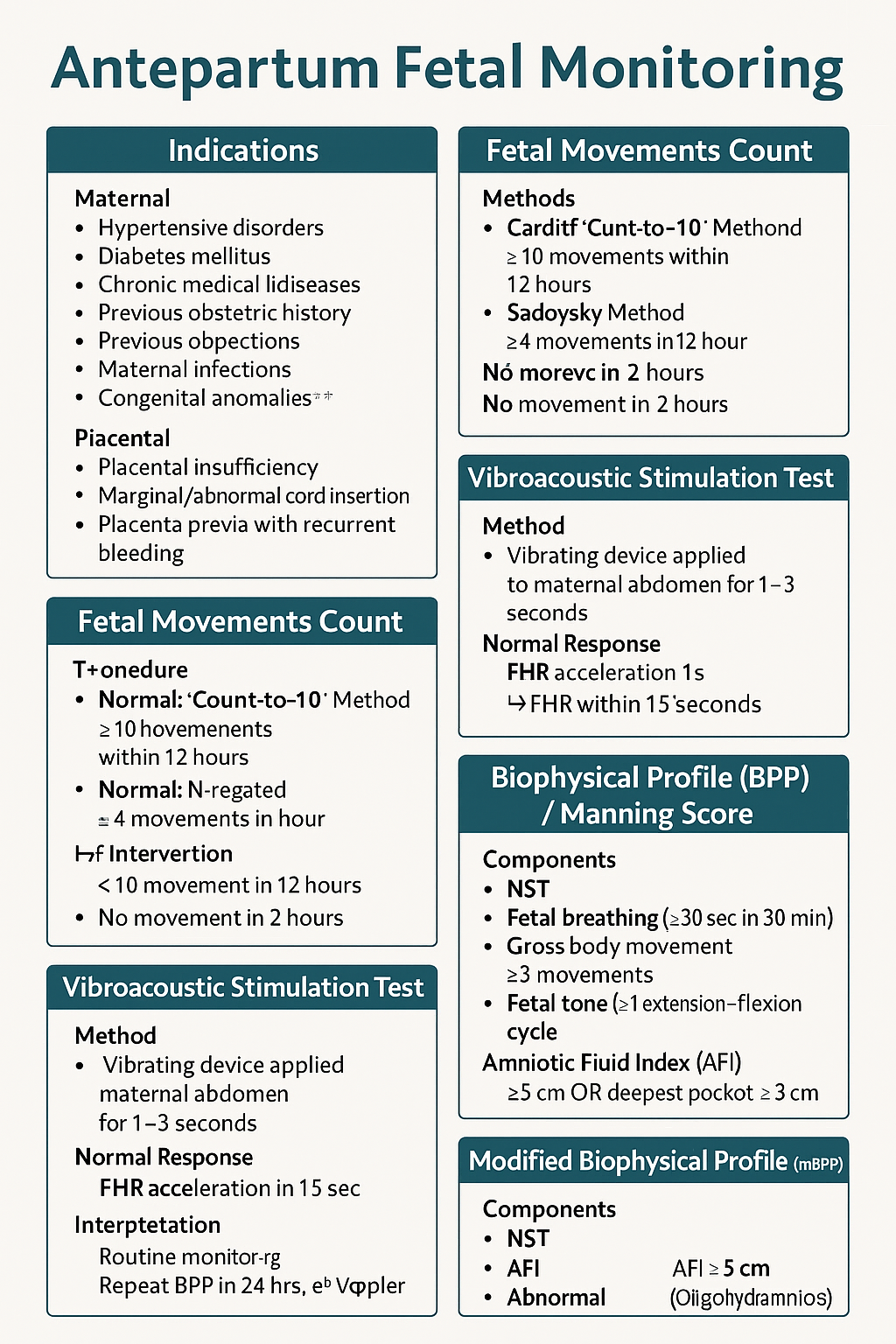
Antepartum Fetal Monitoring: Indications, NST, Biophysical Profile, Modified BPP & Vibroacoustic Test | Complete Obstetrics Guide 2025
--- # ⭐ **ANTEPARTUM FETAL MONITORING — COMPLETE HIGH-YIELD REFERENCE (NEET PG / INI-CET)** Antepartum fetal surveillance aims to detect **early fetal hypoxia** to prevent stillbirth, reduce perinatal morbidity, and guide timing of delivery. It assesses **placental function**, **oxygenation**, **neurological integrity**, and **fetal compensatory mechanisms**. --- # **1️⃣ Indications for Antepartum Fetal Monitoring** ### **A. Maternal Indications** * **Hypertensive disorders:** Gestational HTN, preeclampsia, eclampsia * **Diabetes mellitus:** GDM requiring insulin/OADs, pre-gestational DM * **Chronic medical diseases:** * Chronic hypertension * Renal disease * Autoimmune disease (SLE, APLA syndrome) * Cardiac disease * Thyroid disease with complications * **Previous obstetric history:** * Previous stillbirth * Previous IUGR baby * Previous neonatal death * Isoimmunization/Rh alloimmunization * **Maternal infections:** TORCH with fetal involvement * **Advanced maternal age (>35)** * **Post-dated pregnancy (>40 weeks)** ### **B. Fetal Indications** * **Decreased fetal movements** * **IUGR (Symmetric/Asymmetric)** * **Oligohydramnios / Polyhydramnios** * **Multiple pregnancy with complications** * **Fetal anemia / hydrops** * **Congenital anomalies** ### **C. Placental Indications** * Placental insufficiency * Marginal/Abnormal cord insertion * Placenta previa with recurrent bleeding --- # **2️⃣ Fetal Movement Count (FMC / Kick Count)** Fetal movements reflect fetal well-being (neurological + metabolic status). ### **Methods** ### **A. Cardiff Count-to-10 Method** * Mother records movements daily. * **Normal:** 10 movements within 12 hours. ### **B. Sadovsky Method** * Count movements for 1 hour after meals. * **Normal:** ≥4 movements/hour. ### **When to worry?** * **<10 movements in 12 hours** * **<4 movements in 1 hour** * **No movement in 2 hours** → urgent evaluation (NST/BPP) ### **Management of Decreased Fetal Movements** 1. Immediate **NST** 2. If NST non-reactive → **BPP** 3. If BPP equivocal → **Doppler studies** 4. If evidence of fetal compromise → **Delivery based on GA** --- # **3️⃣ Non-Stress Test (NST)** NST measures **fetal heart rate accelerations** in response to fetal movements via cardiotocography. ### **Procedure** * Done after **28–32 weeks** (mature autonomic nervous system). * Duration: **20 minutes** (extend to 40 minutes if needed). --- ## **Interpretation (Reactive vs Non-Reactive)** ### ✔ **Reactive NST (Normal)** * **≥2 accelerations** in 20 minutes * Acceleration criteria: * **≥15 bpm for ≥15 sec** (≥32 weeks) * **≥10 bpm for ≥10 sec** (<32 weeks) ### ✔ **Non-Reactive NST** * <2 accelerations in 40 minutes * Suggests fetal sleep cycle, hypoxia, CNS depression. ### **Causes of Non-Reactive NST** * Fetal sleep * Maternal drug intake (MgSO₄, opioids, sedatives) * Hypoxia * Prematurity * Congenital anomalies ### **Next Steps in Non-Reactive NST** * Vibroacoustic stimulation test * BPP * Contraction stress test (rarely used today) * Doppler studies --- # **4️⃣ Vibroacoustic Stimulation Test (VAST)** Used to differentiate fetal sleep from hypoxia in non-reactive NST. ### **Method** * A vibrating device (artificial larynx) applied to maternal abdomen for **1–3 seconds**. ### **Normal Response** * FHR acceleration within **15 seconds** * Converts non-reactive NST → **reactive** ### **Significance** * High negative predictive value * Reduces need for BPP --- # **5️⃣ Biophysical Profile (BPP) / Manning Score** Combines **NST + ultrasound parameters** assessing fetal CNS integrity + oxygenation. ### **Components (Total 10 points)** Each gets **2 = normal**, **0 = abnormal** | Component | Normal Criteria (2 points) | | ------------------------------ | --------------------------------- | | **NST** | Reactive | | **Fetal breathing** | ≥30 sec in 30 min | | **Gross body movement** | ≥3 movements | | **Fetal tone** | ≥1 extension–flexion cycle | | **Amniotic Fluid Index (AFI)** | AFI ≥5 cm OR deepest pocket ≥2 cm | --- ## **Scoring & Interpretation** | Score | Interpretation | Management | | -------- | -------------- | ------------------------------------------- | | **8–10** | Normal | Routine monitoring | | **6** | Equivocal | Repeat BPP in 24 hrs; evaluate Doppler | | **4** | Abnormal | Risk of fetal hypoxia → Delivery if ≥34 wks | | **0–2** | Severe hypoxia | Immediate delivery | --- # **6️⃣ Modified Biophysical Profile (mBPP)** Simplified & widely used. ### **Components** 1. **NST** 2. **AFI (Amniotic Fluid Index)** ### **Interpretation** * **Normal:** Reactive NST + AFI ≥5 cm * **Abnormal:** * Non-reactive NST * AFI <5 cm (Oligohydramnios) → placental insufficiency ### **Management** * If abnormal mBPP → full BPP or Doppler; consider delivery based on GA. --- # **7️⃣ Contraction Stress Test (OBSOLETE mostly)** Assesses fetal response to **uterine contractions** → risk of late decelerations. Rarely done due to risk + availability of Doppler and BPP. --- # **8️⃣ Putting It All Together — Management Algorithm** ### **Decreased fetal movements →** 1. **NST** 2. If reactive → reassure 3. If non-reactive → repeat + VAST 4. If still non-reactive → BPP 5. * **BPP ≤4** → Delivery * **BPP 6** → Repeat in 24 hrs * **BPP 8–10** → Continue routine follow-ups 6. Assess **AFI, Doppler, maternal condition** --- # **9️⃣ Important Clinical Correlations** ### **NST becomes abnormal earliest in fetal hypoxia** CNS activity reduces → loss of accelerations. ### **BPP components lost in sequence during hypoxia (Late → Early loss)** 1. **NST** 2. **Fetal breathing** 3. **Gross movement** 4. **Fetal tone** (last to disappear) 5. **AFI reduced** from chronic utero-placental insufficiency ### **AFI is chronic marker**; NST is acute marker. --- # ⭐ **HIGH-YIELD VALUES (MUST REVISE)** * Reactive NST: **≥2 accelerations** (15 × 15) * Tone: 1 flexion–extension * Breathing: ≥1 episode ≥30 sec * Movement: ≥3 body movements * AFI: Normal ≥5 cm * Modified BPP = NST + AFI * Sleep cycle: **20–40 min** → extend NST to 40 min --- --- # ⭐ **25 CASE SCENARIOS WITH DETAILED MANAGEMENT** *(Antepartum Fetal Surveillance: FMC, NST, BPP, VAST, mBPP)* --- # **1️⃣ Case Scenario – Decreased Fetal Movements at 34 Weeks** A 28-year-old G2P1 at 34 weeks reports **no fetal movements for 8 hours**. ### **Management** 1. Immediate **NST** 2. If **reactive** → reassure, daily kick count 3. If **non-reactive** → extend to 40 min 4. If still non-reactive → **VAST** 5. If remains non-reactive → **BPP** 6. * **BPP ≥8** → Follow-up * **BPP ≤4** → Deliver based on GA --- # **2️⃣ Case Scenario – Non-Reactive NST in a Diabetic Mother** GDM on insulin at 36 weeks undergoes NST → **non-reactive** after 40 minutes. ### **Management** 1. Perform **VAST** 2. If reactive → repeat NST in 1 week 3. If still non-reactive → **Full BPP** 4. If BPP score **≤4** → Plan delivery 5. Assess **AFI & Doppler** for placental insufficiency --- # **3️⃣ Case Scenario – Oligohydramnios with IUGR** 30-year-old at 32 weeks with **AFI = 4 cm**, EFW <10th percentile. ### **Management** 1. Start **modified BPP (NST + AFI)** 2. Daily NST 3. Doppler: **Umbilical artery S/D ratio** 4. If AEDF/REDF → **Immediate delivery** 5. If NST non-reactive → full BPP 6. Steroids if <34 weeks --- # **4️⃣ Case – Post-Dated Pregnancy (41 Weeks)** Patient at 41+2 weeks shows decreased fetal movement. ### **Management** 1. **NST + AFI** 2. If NST reactive & AFI normal → induce labour within 24–48 hrs 3. If NST non-reactive → BPP 4. BPP ≤6 → Deliver 5. Continuous intrapartum monitoring --- # **5️⃣ Case – Preeclampsia with Severe Features** 32 weeks, BP 160/110, proteinuria +++, fetus active. ### **Management** 1. Daily **NST** 2. Twice-weekly **BPP** 3. Doppler (UA + MCA) weekly 4. Magnesium sulfate for seizure prophylaxis 5. Deliver at 34 weeks or earlier if fetal compromise --- # **6️⃣ Case – Chronic Hypertension with Reduced Movements** 35-year-old with chronic HTN reports <4 kicks in 1 hr. ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. If AFI <5 → suspect placental insufficiency 4. Admit, daily surveillance 5. Deliver if BPP ≤4 or Doppler abnormal --- # **7️⃣ Case – IUGR with Normal NST** 29 weeks, IUGR but **reactive NST**. ### **Management** 1. Continue **twice-weekly NST** 2. Weekly Doppler (UA/ MCA/ CPR ratio) 3. Growth scan every 2 weeks 4. Deliver if Doppler deteriorates or NST becomes abnormal --- # **8️⃣ Case – Polyhydramnios with GDM** 30-year-old with polyhydramnios, NST reactive. ### **Management** 1. Twice-weekly NST 2. AFI monitoring 3. Doppler weekly 4. Induce at 38–39 weeks 5. Prepare for shoulder dystocia risk --- # **9️⃣ Case – Decreased Fetal Movement in Obese Mother** NST shows **baseline variability minimal**. ### **Management** 1. Rule out maternal meds, sleep cycle 2. Extend NST + VAST 3. If still abnormal → BPP 4. Deliver if BPP ≤4 --- # **🔟 Case – Rh-Isoimmunization** 28 weeks, MCA PSV >1.5 MOM (fetal anemia suspected). ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. Plan **intrauterine transfusion** 4. After IUT: Daily NST --- # **1️⃣1️⃣ Case – Twin Pregnancy with Growth Discordance** NST non-reactive for smaller twin. ### **Management** 1. VAST 2. If still non-reactive → BPP for each twin 3. Doppler UA/MCA/ Ductus venosus 4. Deliver if evidence of compromise --- # **1️⃣2️⃣ Case – Maternal Hypoglycemia Before NST** NST shows no accelerations. ### **Management** 1. Give oral glucose 2. Repeat NST 3. If becomes reactive → normal 4. If persistently non-reactive → VAST → BPP --- # **1️⃣3️⃣ Case – Placental Abruption Suspicion** Pain + bleeding + reduced movements. ### **Management** 1. **Immediate NST** 2. If late decelerations / bradycardia → **Immediate delivery** 3. Stabilize mother --- # **1️⃣4️⃣ Case – COVID Positive Mother with Decreased Movements** NST non-reactive. ### **Management** 1. Rule out maternal fever, hypoxia 2. Oxygen + hydration 3. VAST 4. If still non-reactive → BPP 5. Deliver if fetal compromise --- # **1️⃣5️⃣ Case – Smoking Mother with IUGR** NST shows decreased variability. ### **Management** 1. VAST 2. BPP 3. Doppler UA 4. Nicotine cessation + fetal surveillance every 2–3 days --- # **1️⃣6️⃣ Case – Absent Fetal Breathing on BPP** BPP = 6/10 (breathing absent). ### **Management** 1. Repeat BPP in 24 hrs 2. If repeat BPP ≤6 → Deliver 3. Continuous NST monitoring --- # **1️⃣7️⃣ Case – Low AFI but Reactive NST** AFI = 4 cm at 37 weeks. ### **Management** 1. Diagnose **oligohydramnios** 2. Admit, hydration 3. Modified BPP daily 4. Deliver at 37–38 weeks --- # **1️⃣8️⃣ Case – Maternal Seizure on MgSO₄** NST shows minimal variability (drug effect). ### **Management** 1. Continue monitoring 2. Do not interpret variability during MgSO₄ therapy 3. Use **BPP** instead of NST --- # **1️⃣9️⃣ Case – Poorly Controlled Diabetes** 36 weeks, polyhydramnios + macrosomia. ### **Management** 1. NST every 2–3 days 2. Weekly BPP 3. Deliver at 38 weeks 4. Prepare for shoulder dystocia --- # **2️⃣0️⃣ Case – Maternal Dehydration** NST non-reactive. ### **Management** 1. Give IV fluids 2. Repeat NST 3. If reactive → dehydration cause 4. If persists → BPP --- # **2️⃣1️⃣ Case – Postpartum Hemorrhage Risk Mother** Placenta previa major. ### **Management** 1. Weekly NST 2. BPP if NST abnormal 3. Plan elective C-section at 36–37 weeks --- # **2️⃣2️⃣ Case – Fetal Tachycardia** FHR 170 bpm in NST. ### **Management** 1. Exclude maternal fever, dehydration, drugs 2. Treat maternal cause 3. If persists → BPP + Doppler 4. Consider delivery if fetal compromise --- # **2️⃣3️⃣ Case – Mother on Sedatives** NST non-reactive. ### **Management** 1. Document medication effect 2. Perform BPP instead of repeating NST 3. Reassure if BPP normal --- # **2️⃣4️⃣ Case – Sudden IUD Suspicion** No FHR detected in NST. ### **Management** 1. Confirm with ultrasound 2. Evaluate cause (abruption, cord accident) 3. Manage according to GA and maternal stability --- # **2️⃣5️⃣ Case – Preterm (<32 Weeks) Non-Reactive NST** At 30 weeks, NST non-reactive. ### **Management** 1. Extend NST to 40 min 2. Apply VAST 3. If still non-reactive → BPP 4. If BPP ≤4 → Deliver after steroid cover 5. If BPP normal → prematurity likely cause ---
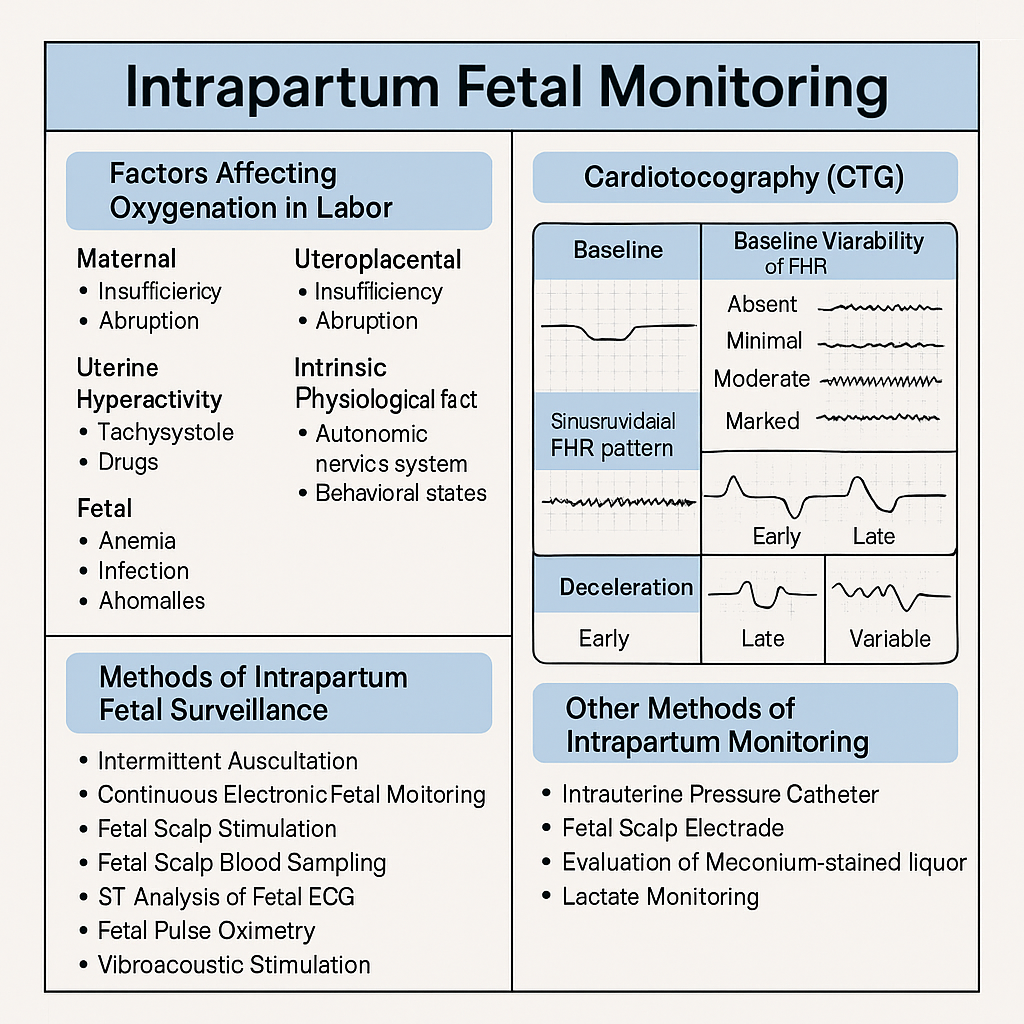
Intrapartum Fetal Monitoring: CTG Interpretation, Decelerations, Sinusoidal Pattern & Complete Management Guide 2025
Below are **30 detailed intrapartum fetal monitoring case scenarios with complete management**, written in **NEET PG / INI-CET exam style**. Each scenario includes **clinical context → CTG finding → diagnosis → step-wise management**. --- # ✅ **30 CASE SCENARIOS WITH DETAILED MANAGEMENT (Intrapartum Fetal Monitoring)** --- ## **1️⃣ Case — Late Decelerations in a Preeclamptic Mother** A 25-year-old primigravida, 4 cm dilated, on oxytocin. CTG shows **recurrent late decelerations**, baseline 150, variability <5 bpm. ### **Diagnosis** Uteroplacental insufficiency from **preeclampsia + hyperstimulation**. ### **Management** 1. Stop oxytocin 2. Left lateral position 3. IV fluids 4. If contraction frequency >5/10 min → **tocolysis (terbutaline 0.25 mg SC)** 5. If no improvement → **FBS** 6. If pH <7.20 or tracing deteriorates → **Emergency LSCS** --- ## **2️⃣ Case — Variable Decelerations with Oligohydramnios** G2P1, term labor, CTG shows **variable decelerations with shoulders**, adequate variability. ### **Diagnosis** Cord compression due to oligohydramnios. ### **Management** 1. Maternal repositioning 2. Amnioinfusion 3. Continue labor if variability normal 4. If severe recurrent variables + loss of variability → expedite delivery --- ## **3️⃣ Case — Sinusoidal Pattern** Rh-negative woman, fetus 38 weeks. CTG: **true sinusoidal pattern**. ### **Diagnosis** Severe fetal anemia. ### **Management** 1. Immediate evaluation (Kleihauer test, ultrasound MCA Doppler if time permits) 2. **Emergency LSCS** 3. Prepare NICU for transfusion --- ## **4️⃣ Case — Prolonged Deceleration from Cord Prolapse** During vaginal exam, a loop of cord felt. CTG shows **bradycardia at 80 bpm** for 4 minutes. ### **Management** 1. Lift presenting part manually 2. Knee–chest position 3. Call for emergency LSCS 4. Warm sterile saline-soaked gauze to prevent vasospasm 5. Deliver within **<30 minutes** --- ## **5️⃣ Case — Tachysystole-Induced Late Decelerations** Oxytocin infusion running, contractions 6/10 min. CTG: recurrent late decels. ### **Management** 1. Stop oxytocin immediately 2. Terbutaline 0.25 mg SC 3. Lateral position 4. Reassess 5. If persists → expedite delivery --- ## **6️⃣ Case — Minimal Variability for 50 Minutes** Primigravida in active labor. CTG: baseline 140, variability <5 bpm for 50 min, no decels. ### **Diagnosis** Non-reassuring CTG, possibly fetal sleep or medication effect. ### **Management** 1. Scalp stimulation 2. If acceleration present → reassuring 3. If absent → FBS or continuous monitoring 4. Continue labor if other parameters normal --- ## **7️⃣ Case — Meconium-Stained Liquor with Abnormal CTG** Thick meconium + variable decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. Amnioinfusion (if available) 3. Prepare for operative delivery 4. NICU standby for Meconium Aspiration Syndrome --- ## **8️⃣ Case — Prolonged Deceleration After Epidural** Immediately after epidural, FHR drops to 90 bpm for 3 minutes. ### **Diagnosis** Maternal hypotension causing decreased uteroplacental flow. ### **Management** 1. Left lateral position 2. IV fluid bolus 3. Vasopressor (phenylephrine preferred) 4. If persists beyond 5 minutes → consider LSCS --- ## **9️⃣ Case — Fetal Tachycardia with Maternal Fever** CTG shows FHR 180 bpm, moderate variability; maternal temp 101°F. ### **Diagnosis** Chorioamnionitis. ### **Management** 1. Broad-spectrum antibiotics 2. Acetaminophen 3. Expedite delivery (not LSCS solely for fever) 4. Avoid prolonged labor --- ## **🔟 Case — Arrest of Descent + Late Decelerations** Second stage, fully dilated, prolonged pushing, late decels appear. ### **Management** 1. Check for instrumental eligibility 2. **Forceps or vacuum** if head low 3. If not eligible → emergency LSCS --- ## **1️⃣1️⃣ Case — Recurrent Severe Variable Decelerations** CTG: variable decels dropping to 70 bpm for 60–90 sec. ### **Management** 1. Lateral positioning 2. Amnioinfusion 3. Reduce contractions if tachysystole 4. If persistent → operative delivery --- ## **1️⃣2️⃣ Case — Fetal Scalp pH Borderline** FBS pH = 7.22. ### **Management** 1. Correct reversible causes 2. Repeat FBS in 30 min 3. If worsens → expedite delivery --- ## **1️⃣3️⃣ Case — Loss of Variability with Bradycardia** Baseline 90 bpm, absent variability. ### **Diagnosis** Advanced fetal hypoxia. ### **Management** 1. Immediate decision for LSCS 2. No role of waiting or FBS --- ## **1️⃣4️⃣ Case — CTG Unable to Trace Due to Obesity** During labor, external CTG poor quality. ### **Management** 1. Switch to **fetal scalp electrode (FSE)** 2. Use IUPC for contraction monitoring 3. Continue labor normally if FHR normal --- ## **1️⃣5️⃣ Case — Category III CTG in Trial of Labor After Cesarean (TOLAC)** Late decels + minimal variability + scar tenderness. ### **Diagnosis** Scar rupture suspected. ### **Management** 1. Immediate emergency LSCS 2. Do NOT attempt instrumental delivery --- ## **1️⃣6️⃣ Case — Hyperstimulation Causing Decelerations** Misoprostol induction; CTG shows tachysystole + decels. ### **Management** 1. Stop prostaglandin 2. Tocolysis 3. Continuous monitoring 4. If fetal distress → emergency delivery --- ## **1️⃣7️⃣ Case — True Sinusoidal Pattern from Fetomaternal Hemorrhage** CTG sinusoidal; Kleihauer test positive. ### **Management** 1. Emergency delivery 2. Neonatal transfusion preparation --- ## **1️⃣8️⃣ Case — Prolonged Decel During Second Stage** Mother pushing vigorously; CTG shows bradycardia. ### **Management** 1. Stop pushing 2. Reassess for instrument delivery 3. If head + station → vacuum/forceps 4. Otherwise → LSCS --- ## **1️⃣9️⃣ Case — Mild Variable Decelerations with Normal Variability** Intermittent variables, contraction-associated. ### **Management** 1. Reassurance 2. Continue monitoring No intervention required. --- ## **2️⃣0️⃣ Case — Shoulder Dystocia + Bradycardia** Delivery nearly complete, FHR falls to 70 bpm. ### **Management** 1. McRoberts + suprapubic pressure 2. Deliver shoulders quickly 3. Neonatal resuscitation readiness --- ## **2️⃣1️⃣ Case — Cord Around Neck Detected on Ultrasound Before Labor** During labor → variable decels appear. ### **Management** 1. Continue monitoring 2. If severe or persistent → expedite delivery 3. Do not intervene solely for nuchal cord --- ## **2️⃣2️⃣ Case — Prolapsed Cord in Breech** CTG severe bradycardia. ### **Management** 1. Knee–chest position 2. Manual elevation of presenting part 3. Emergency LSCS --- ## **2️⃣3️⃣ Case — Minimal Variability from Opioid Analgesia** Given pethidine 15 min ago; variability <5. ### **Management** 1. Observe for 30–60 min 2. If variability recovers → continue 3. If not → evaluate for fetal hypoxia --- ## **2️⃣4️⃣ Case — Reassuring CTG in Low-Risk Labor** Baseline 140, variability 10, accelerations present. ### **Management** Continue routine monitoring. --- ## **2️⃣5️⃣ Case — Excessive Maternal Dehydration** CTG shows fetal tachycardia 170 bpm. ### **Management** 1. IV fluid bolus 2. Assess maternal vitals 3. Continue monitoring --- ## **2️⃣6️⃣ Case — Placental Abruption Suspected** Pain + bleeding + fetal tachycardia → later bradycardia. ### **Management** 1. Stabilize mother 2. Immediate LSCS if fetus alive 3. Vaginal delivery only if imminent --- ## **2️⃣7️⃣ Case — IUGR Baby with Recurrent Late Decelerations** CTG: late decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. No role for prolonged labor 3. **Expedite delivery** --- ## **2️⃣8️⃣ Case — Maternal Seizure (Eclampsia)** CTG: prolonged decel. ### **Management** 1. Stabilize mother (MgSO₄, airway) 2. Left lateral position 3. If fetal recovery absent → LSCS --- ## **2️⃣9️⃣ Case — Vaginal Birth After Multiple Variables** CTG mostly reassuring except mild variables. ### **Management** 1. Continue monitoring 2. Check for cord issues 3. No intervention unless severe --- ## **3️⃣0️⃣ Case — Failure of Fetal Response to Scalp Stimulation** Minimal variability, no acceleration after stimulation. ### **Diagnosis** Hypoxia suspected. ### **Management** 1. FBS if available 2. If pH abnormal → immediate delivery 3. If not available → treat as pathological CTG → expedite delivery --- If you want, I can also produce: ✅ **HTML + CSS + JS EXAM MODE MCQs (25/30/50)** ✅ **SEO title/description/keywords** ✅ **A medical diagram image for intrapartum fetal monitoring** Just say **“generate MCQs”**, **“generate image”**, or **“give SEO”**. Below is your **complete, concise-but-exhaustive master reference** on **Intrapartum Fetal Monitoring** — fully aligned with NEET PG / INI-CET high-yield requirements. --- # ⭐ **INTRAPARTUM FETAL MONITORING — COMPLETE DETAILED NOTES (2025)** --- ## **1️⃣ Factors Affecting Fetal Oxygenation During Labor** Fetal oxygenation depends on uninterrupted flow across **four levels**: ### **A. Maternal Factors** * **Maternal oxygenation:** Hypoxia, severe anemia, pulmonary disease. * **Uterine perfusion:** Hypotension (epidural, hemorrhage), dehydration, aortocaval compression. * **Uterine hyperactivity:** Tachysystole (>5 contractions/10 min), hypertonus ↓ intervillous blood flow. * **Drugs:** β-agonists ↑ fetal tachycardia; opioids ↓ variability. ### **B. Uteroplacental Factors** * Placental insufficiency (hypertension, preeclampsia, post-maturity). * Placental abruption, infarction, previa, accreta spectrum. * Umbilical cord compression (oligohydramnios, cord prolapse, tight nuchal cord). ### **C. Fetal Factors** * Fetal anemia, infections, acidosis. * Congenital anomalies (especially CNS, cardiac). * Prematurity → reduced variability. ### **D. Intrinsic Physiological Factors** * Autonomic nervous system balance (sympathetic/parasympathetic). * Fetal behavioral states (quiet sleep cycles ↓ variability). --- ## **2️⃣ Methods of Intrapartum Fetal Surveillance** ### **A. Intermittent Auscultation (IA)** * Using **Pinard stethoscope** or **Doppler**. * Low-risk pregnancies. * Frequency: * **1st stage:** every 30 min * **2nd stage:** every 5 min * Look for: baseline, accelerations, decelerations. ### **B. Continuous Electronic Fetal Monitoring (EFM / CTG)** * External US transducer + tocodynamometer. * Internal scaling: scalp electrode + IUPC (intrauterine pressure catheter) when needed. ### **C. Fetal Scalp Stimulation** * Acceleration after stimulation → reassuring (pH > 7.2). ### **D. Fetal Scalp Blood Sampling (FBS)** → Direct measure of fetal acid-base status. * **Normal pH ≥ 7.25** * **Borderline 7.21–7.24** * **Abnormal < 7.20** → urgent delivery. ### **E. ST-Analysis of Fetal ECG (STAN)** * Detects myocardial hypoxia (ST changes). * Used with CTG. ### **F. Fetal Pulse Oximetry (rare)** * Reassurance if SpO₂ > 30%. ### **G. Vibroacoustic Stimulation** * Sound stimulus → acceleration = good oxygenation. --- ## **3️⃣ Cardiotocography (CTG) – Complete Interpretation** CTG has **5 components**: **Baseline, Variability, Accelerations, Decelerations, Contractions.** --- ## **3.1 Baseline Fetal Heart Rate** Normal: **110–160 bpm** ### **Tachycardia (>160 bpm) causes:** * Maternal fever (chorioamnionitis) * Fetal hypoxia early * Fetal anemia * Drugs: β-agonists, atropine ### **Bradycardia (<110 bpm) causes:** * Vagal stimulation (head compression) * Cord compression * Prolonged deceleration → late sign of hypoxia --- ## **3.2 Baseline Variability (BV)** Reflects fetal autonomic integrity. | **Type** | **Range** | **Significance** | | --------------------- | ------------ | ------------------------------------------ | | Absent | 0 bpm | Severe hypoxia, acidosis, drugs | | Minimal | <5 bpm | Sleep cycle, opioids, prematurity, hypoxia | | **Moderate (Normal)** | **6–25 bpm** | Good oxygenation | | Marked | >25 bpm | Early hypoxia, cord compression | --- ## **3.3 Accelerations** * Abrupt ↑ in FHR by ≥15 bpm for ≥15 sec. * **Reassuring sign** → fetal well-being. --- ## **3.4 Decelerations — Types & Complete Interpretation** ### **A. Early Decelerations** * Mirror contractions. * Due to **head compression**. * **Benign, no treatment.** ### **B. Late Decelerations** * Begin after the contraction peak → return after contraction ends. * Due to **uteroplacental insufficiency**. * **Always concerning**, esp. with absent variability. ### **C. Variable Decelerations** * Abrupt fall in FHR, variable shape. * Due to **cord compression**. * May have "shoulders" (pre- & post-acceleration). * Severe if >60 bpm drop lasting >60 sec. ### **D. Prolonged Deceleration** * FHR drop ≥15 bpm lasting **2–10 min**. * > 10 min = change in baseline. ### **E. Sinusoidal Pattern (MOST IMPORTANT)** **True Sinusoidal Pattern** * Smooth, regular, sine-wave oscillation (3–5 cycles/min) * Amplitude 5–15 bpm * No variability, no accelerations * **Causes:** * Severe fetal anemia (Rh isoimmunization, fetomaternal hemorrhage) * Twin-to-twin transfusion * Hypoxia late stage * **Immediate delivery required** **Pseudo-sinusoidal:** * Seen with opioids — benign. --- ## **4️⃣ NICE 2024 Categories of CTG Interpretation** | Category | Findings | Action | | ------------------------------- | -------------------------------------------------------- | ------------------------------------------------ | | **Normal (Category I)** | Baseline 110–160, Variability 6–25, No repetitive decels | Continue | | **Suspicious (Category II)** | One non-reassuring feature | Correct reversible causes, close monitoring | | **Pathological (Category III)** | ≥1 abnormal feature OR ≥2 non-reassuring | Immediate evaluation, FBS, or expedited delivery | ### **Features** **Reassuring:** * Baseline 110–160 * Variability 6–25 * No decelerations / early decels * Accelerations present **Non-reassuring:** * Baseline 100–109 or 161–180 * Variability <5 for 40–90 min * Variable decels with features * Single prolonged decel <3 min **Abnormal:** * Baseline <100 or >180 * Variability <5 for >90 min * Late decels / prolonged decels >3 min * Sinusoidal pattern --- ## **5️⃣ Management of Abnormal CTG** ### **A. Correct Reversible Causes** * Left lateral position * IV fluids → treat maternal hypotension * Stop oxytocin (if tachysystole) * Tocolysis if uterine hyperstimulation (Terbutaline 0.25 mg SC) * Oxygen (only if maternal hypoxia) ### **B. Fetal Assessment** * Fetal scalp stimulation * FBS (pH or lactate) ### **C. Delivery** * If pH <7.20 OR pathological CTG persists * Emergency LSCS or instrumental delivery depending on stage --- ## **6️⃣ Other Methods of Intrapartum Monitoring** ### **A. Intrauterine Pressure Catheter (IUPC)** * Measures **Montevideo units** * Adequate labor: **>200 MVU** ### **B. Fetal Scalp Electrode (FSE)** * Accurate beat-to-beat FHR * Used when external CTG is poor. ### **C. Meconium-stained liquor evaluation** * Thick meconium + abnormal CTG → intrapartum hypoxia risk. ### **D. Lactate Monitoring** * Fetal scalp lactate <4.8 mmol/L reassuring. --- ## **7️⃣ Quick High-Yield Revision Table** | Topic | Key Points | | ------------------------------- | ------------------------------- | | Best indicator of fetal hypoxia | **Reduced variability** | | Worst CTG sign | **Sinusoidal pattern** | | Earliest sign of hypoxia | **Tachycardia** | | Most common deceleration | **Variable (cord compression)** | --- If you want, I can also generate: ✅ SEO title, description & keywords ✅ 25 hard case-based MCQs (HTML + CSS + JS EXAM MODE) ✅ 25 case scenarios with management ✅ Medical diagram image (via image generator) Just tell me **“continue”** with what you need.
Comments & Discussion
Use this thread like a mini viva: add differentials, staging systems, drug regimens and exam tricks.
Login or register to comment.
No comments yet – start by adding exam-style discussion points.