dinesh – Profile
Streamora author since Dec 2025. This profile aggregates all their public posts and exam-oriented notes.
Public posts by this author
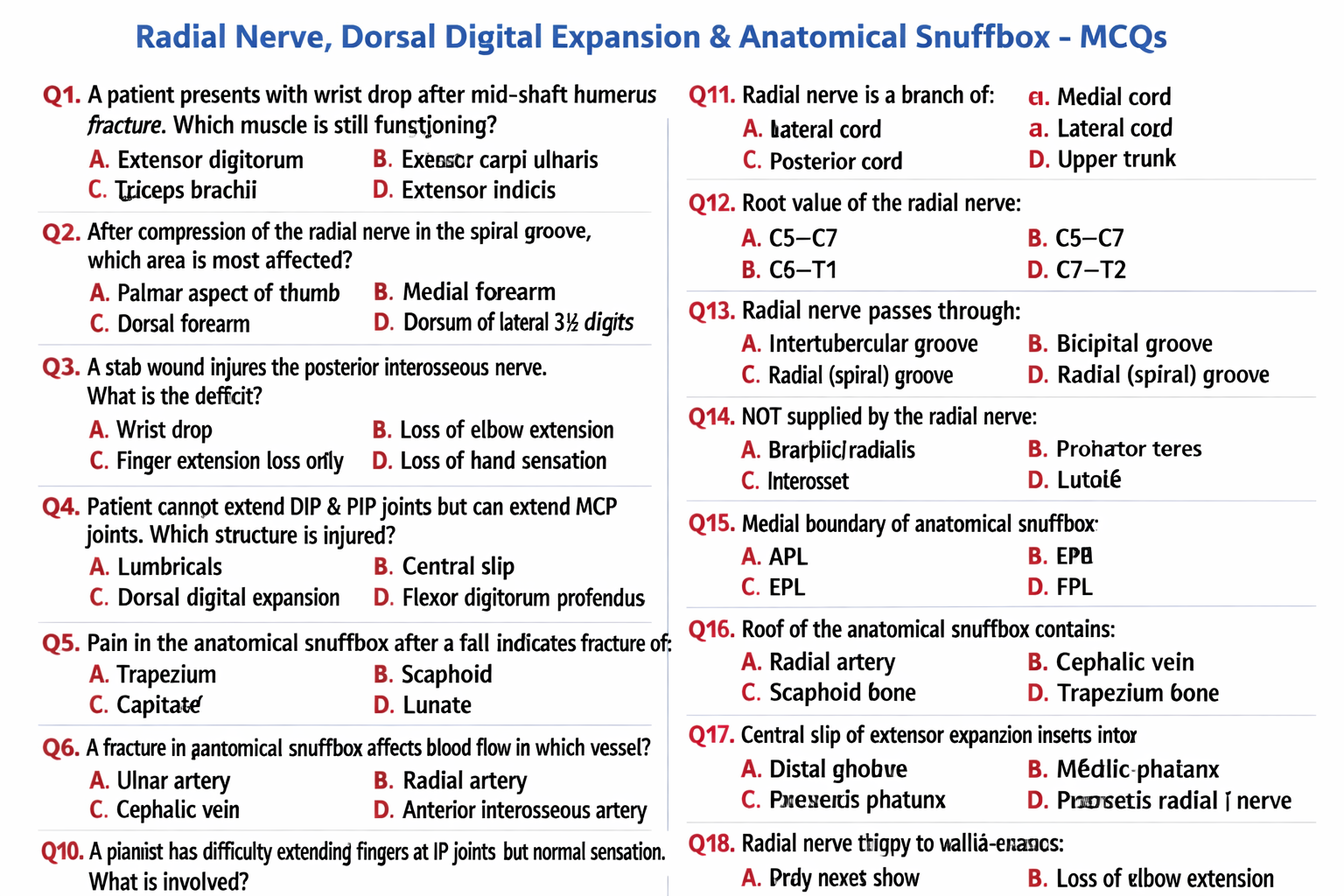
Radial Nerve, Dorsal Digital Expansion and Anatomical Snuffbox Anatomy Explained
Below is a **clear, exam-oriented, complete anatomy note** on **Radial Nerve**, **Dorsal Digital Expansion**, and **Anatomical Snuffbox**. (As requested: **no images**.) --- # **Radial Nerve, Dorsal Digital Expansion, and Anatomical Snuffbox – Complete Anatomy Guide** --- ## **1. Radial Nerve** ### **Definition** The **radial nerve** is the **largest branch of the posterior cord of the brachial plexus**, providing **motor supply to extensor muscles** of the upper limb and **sensory supply to the posterior arm, forearm, and dorsum of the hand**. ### **Root Value** * **C5–T1** --- ### **Origin** * Arises from the **posterior cord of the brachial plexus** --- ### **Course** #### **Axilla** * Lies **posterior to the axillary artery** * Exits the axilla through the **lower triangular space** * Accompanied by the **profunda brachii artery** #### **Arm** * Enters the **radial (spiral) groove** of the humerus * Runs between **medial and lateral heads of triceps** * Supplies **triceps brachii** * Pierces the **lateral intermuscular septum** * Enters the anterior compartment near the lateral epicondyle #### **Cubital Fossa** * Lies **anterior to the lateral epicondyle** * Divides into: * **Superficial branch (sensory)** * **Deep branch (motor → posterior interosseous nerve)** #### **Forearm** * **Deep branch**: * Pierces **supinator** * Continues as **posterior interosseous nerve** * Supplies extensor muscles * **Superficial branch**: * Runs under brachioradialis * Becomes superficial near wrist * Supplies dorsum of hand --- ### **Branches** #### **Motor** * Triceps brachii * Anconeus * Brachioradialis * Extensor carpi radialis longus * All **extensors of wrist and fingers** (via posterior interosseous nerve) #### **Sensory** * Posterior cutaneous nerve of arm * Posterior cutaneous nerve of forearm * Dorsal digital nerves to: * Lateral 3½ digits (proximal parts) --- ### **Applied Anatomy** * **Radial nerve palsy**: * Wrist drop * Loss of finger extension * **Mid-shaft humerus fracture** → injury in radial groove * **Saturday night palsy** → compression in spiral groove --- ## **2. Dorsal Digital Expansion (Extensor Expansion / Hood)** ### **Definition** The **dorsal digital expansion** is a **triangular aponeurotic expansion** on the **dorsum of fingers**, formed mainly by **extensor digitorum tendon**, allowing **coordinated finger movements**. --- ### **Formation** Formed by: * Extensor digitorum tendon * Contributions from: * Lumbricals * Interossei --- ### **Structure** * **Central slip**: * Inserts into base of **middle phalanx** * **Two lateral bands**: * Reunite to insert into **distal phalanx** * Covers the **dorsum of MCP, PIP, and DIP joints** --- ### **Functions** * Extension at: * Metacarpophalangeal (MCP) joints * Interphalangeal (IP) joints * Allows **interossei and lumbricals** to: * Flex MCP * Extend IP joints --- ### **Clinical Importance** * **Mallet finger**: rupture of terminal tendon * **Boutonnière deformity**: rupture of central slip * **Claw hand deformity**: imbalance of intrinsic muscles --- ## **3. Anatomical Snuffbox** ### **Definition** The **anatomical snuffbox** is a **triangular depression** seen on the **lateral aspect of the dorsum of the hand** when the thumb is extended. --- ### **Boundaries** #### **Lateral (Anterior) Boundary** * Abductor pollicis longus * Extensor pollicis brevis #### **Medial (Posterior) Boundary** * Extensor pollicis longus #### **Proximal Boundary** * Styloid process of radius --- ### **Floor** * Scaphoid * Trapezium --- ### **Roof** * Skin * Superficial fascia * Superficial branch of radial nerve * Cephalic vein --- ### **Contents** * **Radial artery** (main content) --- ### **Clinical Importance** * **Scaphoid fracture**: * Tenderness in snuffbox * Risk of avascular necrosis * Radial artery palpation site * IV cannulation landmark --- ## **Quick Exam Correlation Table** | Structure | Key Clinical Point | | ------------------------ | ----------------------------- | | Radial nerve | Wrist drop | | Dorsal digital expansion | Finger extension coordination | | Anatomical snuffbox | Scaphoid fracture tenderness | --- ### **If you want next** * High-yield **MCQs** * **Clinical case scenarios** * **Comparison tables** * **OSCE-ready short notes** Just tell me 👍
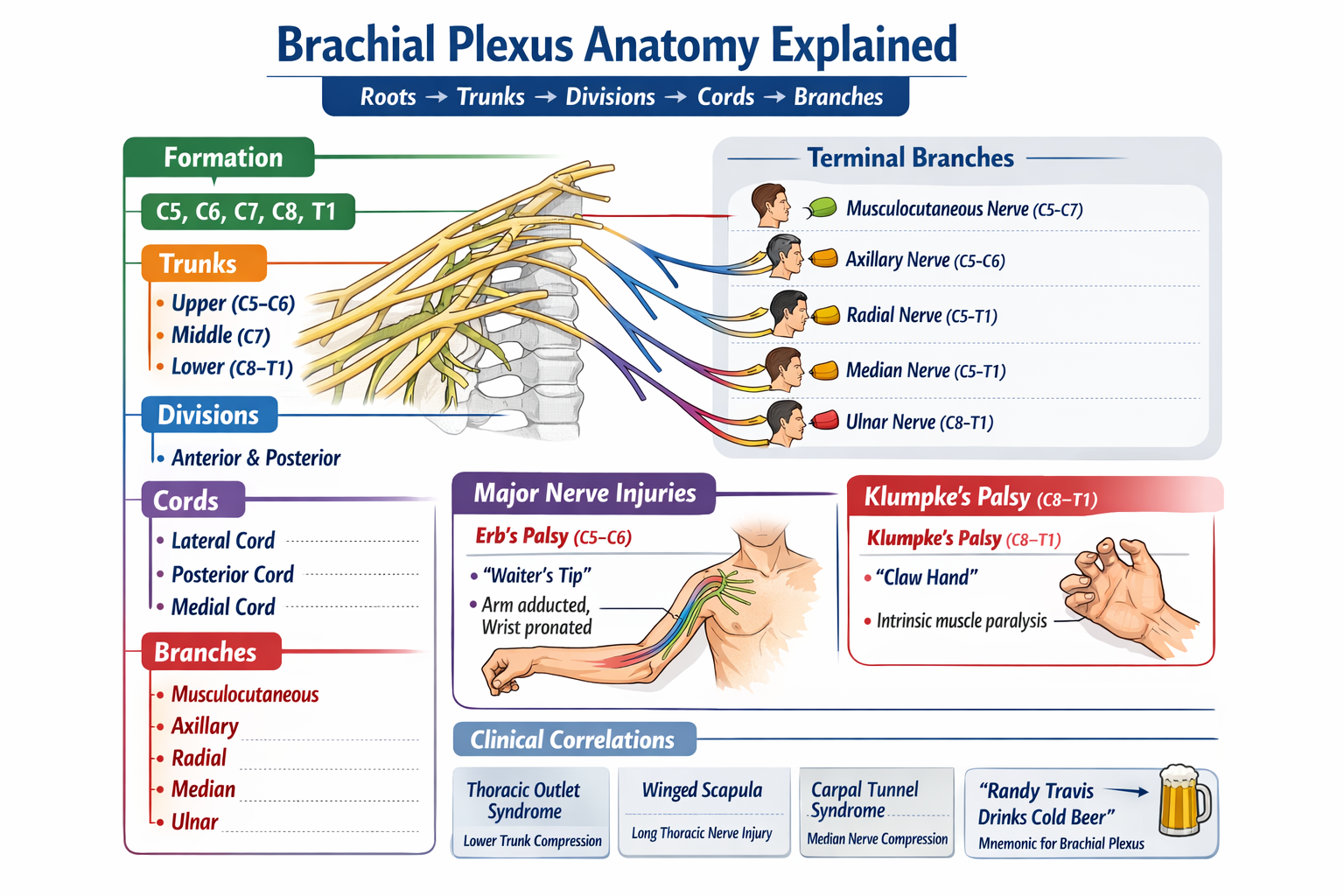
Brachial Plexus Anatomy Explained with Roots Trunks Cords Branches and Clinical Correlations
## **Brachial Plexus – Complete Detailed Anatomy** ### **Definition** The **brachial plexus** is a network of **ventral rami of spinal nerves C5–T1** that provides **motor, sensory, and sympathetic innervation** to the upper limb. --- ## **Formation (Roots → Trunks → Divisions → Cords → Branches)** ### **1. Roots** * **C5, C6, C7, C8, T1** (ventral rami) * Pass between **anterior and middle scalene muscles** in the neck * **Branches from roots:** * **Dorsal scapular nerve (C5)** → Rhomboids, levator scapulae * **Long thoracic nerve (C5–C7)** → Serratus anterior (winged scapula if injured) --- ### **2. Trunks** Formed in the **posterior triangle of the neck** * **Upper trunk:** C5–C6 * **Middle trunk:** C7 * **Lower trunk:** C8–T1 **Branches from trunks:** * **Suprascapular nerve (C5–C6)** → Supraspinatus, infraspinatus * **Nerve to subclavius (C5–C6)** --- ### **3. Divisions** Located **behind the clavicle** * Each trunk divides into: * **Anterior division** → Flexor compartments * **Posterior division** → Extensor compartments * **No branches** arise here --- ### **4. Cords** Named according to relation to the **axillary artery** (in axilla) | Cord | Formation | | ------------------ | ------------------------------------------- | | **Lateral cord** | Anterior divisions of upper + middle trunks | | **Medial cord** | Anterior division of lower trunk | | **Posterior cord** | All posterior divisions | --- ### **5. Terminal Branches** #### **From Lateral Cord** * **Musculocutaneous nerve (C5–C7)** * **Lateral root of median nerve** #### **From Medial Cord** * **Ulnar nerve (C8–T1)** * **Medial root of median nerve** * **Medial cutaneous nerve of arm** * **Medial cutaneous nerve of forearm** #### **From Posterior Cord** * **Axillary nerve (C5–C6)** * **Radial nerve (C5–T1)** --- ## **Major Peripheral Nerves – Functions & Lesions** ### **Musculocutaneous Nerve (C5–C7)** * **Motor:** Biceps, brachialis, coracobrachialis * **Sensory:** Lateral forearm * **Injury:** Weak elbow flexion & supination --- ### **Axillary Nerve (C5–C6)** * **Motor:** Deltoid, teres minor * **Sensory:** Regimental badge area * **Injury:** Surgical neck fracture → loss of shoulder abduction (15–90°) --- ### **Radial Nerve (C5–T1)** * **Motor:** All extensors of arm & forearm * **Sensory:** Posterior arm, forearm, dorsal hand * **Injury:** Wrist drop --- ### **Median Nerve (C5–T1)** * **Motor:** Forearm flexors, thenar muscles * **Sensory:** Lateral 3½ digits (palmar) * **Injury:** Ape hand, loss of pronation, carpal tunnel syndrome --- ### **Ulnar Nerve (C8–T1)** * **Motor:** Intrinsic hand muscles * **Sensory:** Medial 1½ fingers * **Injury:** Claw hand, Froment sign --- ## **Clinical Correlations** ### **Upper Trunk Lesion (Erb Palsy – C5–C6)** * Causes: Birth injury, fall on shoulder * Deformity: **“Waiter’s tip”** * Affected nerves: Axillary, musculocutaneous, suprascapular --- ### **Lower Trunk Lesion (Klumpke Palsy – C8–T1)** * Causes: Traction of abducted arm * Features: * Intrinsic hand muscle paralysis * **Claw hand** * **Horner syndrome** (if T1 sympathetic affected) --- ## **Applied Anatomy** * **Scalene block anesthesia** targets roots/trunks * **Axillary block** targets terminal branches * **Thoracic outlet syndrome** affects lower trunk * **Winged scapula** → Long thoracic nerve injury --- ## **Key Exam Mnemonic** **Roots → Trunks → Divisions → Cords → Branches** **“Randy Travis Drinks Cold Beer”** --- If you want, I can also provide: * **High-yield exam tables** * **Clinical case-based MCQs** * **Dermatome & myotome correlation** * **Pure neuroanatomy vs applied surgery focus** Just tell me 👍
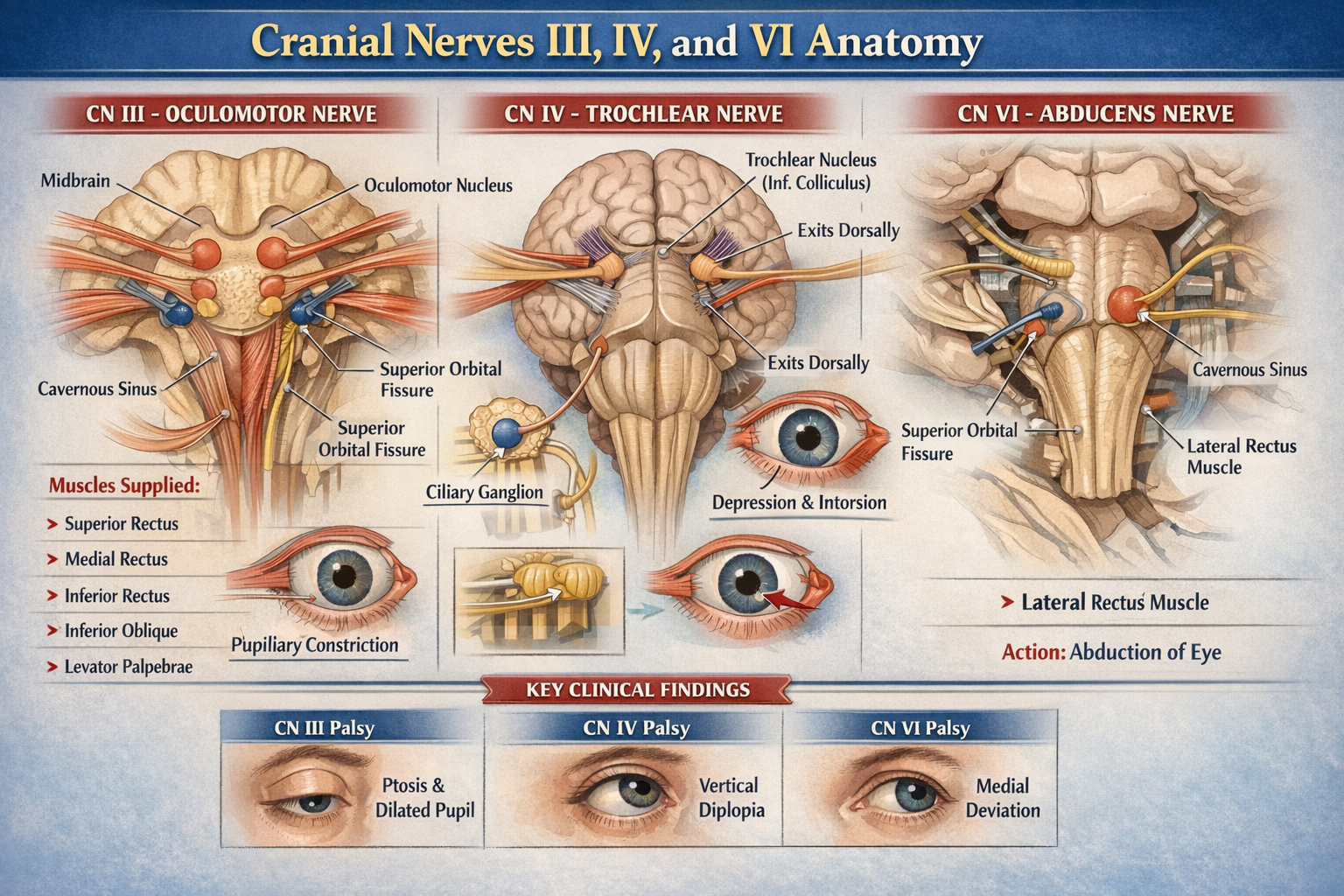
Cranial Nerves III IV VI Anatomy Detailed Overview for Medical Students
Below is a **concise but complete, exam-oriented anatomy reference** for **Cranial Nerves III, IV, and VI** (oculomotor, trochlear, abducens). **No images included**, as requested. --- # Cranial Nerves III, IV, and VI – Detailed Anatomy ## Overview (Common Function) Cranial nerves **III, IV, and VI** are **purely motor nerves** supplying the **extra-ocular muscles** that control eye movements. Cranial nerve III also carries **parasympathetic fibers** for pupil constriction and accommodation. --- ## CRANIAL NERVE III – OCULOMOTOR NERVE ### Functional Components * **Somatic efferent** → extra-ocular muscles * **General visceral efferent (parasympathetic)** → pupil and lens --- ### Nuclei (Midbrain) Located at the **level of the superior colliculus**: 1. **Oculomotor nuclear complex** * Supplies all extra-ocular muscles except SO and LR 2. **Edinger–Westphal nucleus** * Parasympathetic nucleus * Supplies sphincter pupillae and ciliary muscle --- ### Intracranial Course * Emerges from **ventral midbrain** in the **interpeduncular fossa** * Passes between: * **Posterior cerebral artery** * **Superior cerebellar artery** * Runs in **lateral wall of cavernous sinus** * Divides into **superior and inferior divisions** * Enters orbit through **superior orbital fissure** (inside common tendinous ring) --- ### Orbital Course and Branches #### Superior Division * Levator palpebrae superioris * Superior rectus #### Inferior Division * Medial rectus * Inferior rectus * Inferior oblique * Parasympathetic root to **ciliary ganglion** --- ### Parasympathetic Pathway * Edinger–Westphal nucleus → oculomotor nerve * Synapse in **ciliary ganglion** * Postganglionic fibers via **short ciliary nerves** to: * Sphincter pupillae → pupillary constriction * Ciliary muscle → accommodation --- ### Muscles Supplied * Superior rectus * Inferior rectus * Medial rectus * Inferior oblique * Levator palpebrae superioris --- ### Actions * Eye elevation, depression, adduction * Pupillary constriction * Accommodation * Eyelid elevation --- ## CRANIAL NERVE IV – TROCHLEAR NERVE ### Functional Component * **Somatic efferent only** --- ### Nucleus (Midbrain) * Located at **level of inferior colliculus** --- ### Unique Anatomical Features * Only cranial nerve: * That **emerges dorsally** * That **decussates completely** * That has the **longest intracranial course** * That supplies the **contralateral muscle** --- ### Intracranial Course * Exits dorsal midbrain * Winds around brainstem laterally * Passes through: * Cavernous sinus (lateral wall) * Superior orbital fissure (outside common tendinous ring) --- ### Orbital Course * Enters orbit superiorly * Supplies **superior oblique muscle** --- ### Muscle Supplied * **Superior oblique** --- ### Action of Superior Oblique * Intorsion * Depression (especially in adducted eye) * Abduction --- ## CRANIAL NERVE VI – ABDUCENS NERVE ### Functional Component * **Somatic efferent only** --- ### Nucleus (Pons) * Located in **dorsal pons**, beneath **facial colliculus** * Facial nerve fibers loop around abducens nucleus --- ### Intracranial Course * Emerges at **pontomedullary junction** * Ascends along clivus * Sharp bend over **petrous apex** * Passes through **cavernous sinus** (adjacent to internal carotid artery) * Enters orbit via **superior orbital fissure** (inside common tendinous ring) --- ### Orbital Course * Supplies **lateral rectus muscle** --- ### Muscle Supplied * **Lateral rectus** --- ### Action * **Abduction of eyeball** --- ## Summary Table | Cranial Nerve | Nucleus Level | Exit from Brainstem | Muscle Supplied | Main Action | | ------------- | -------------------------- | ----------------------- | -------------------------- | -------------------------------- | | CN III | Midbrain (sup. colliculus) | Ventral | Most EOM + parasympathetic | Eye movement, pupil constriction | | CN IV | Midbrain (inf. colliculus) | Dorsal | Superior oblique | Depression, intorsion | | CN VI | Pons | Pontomedullary junction | Lateral rectus | Abduction | --- ## Key Clinical Correlations (Brief) * **CN III palsy** → ptosis, dilated pupil, eye down and out * **CN IV palsy** → vertical diplopia, worse on stairs * **CN VI palsy** → inability to abduct eye, medial deviation --- If you want, I can also provide: * **Cavernous sinus relations** * **Brainstem cross-section correlations** * **Clinical case-based MCQs** * **SEO-friendly formatted version for medical websites**
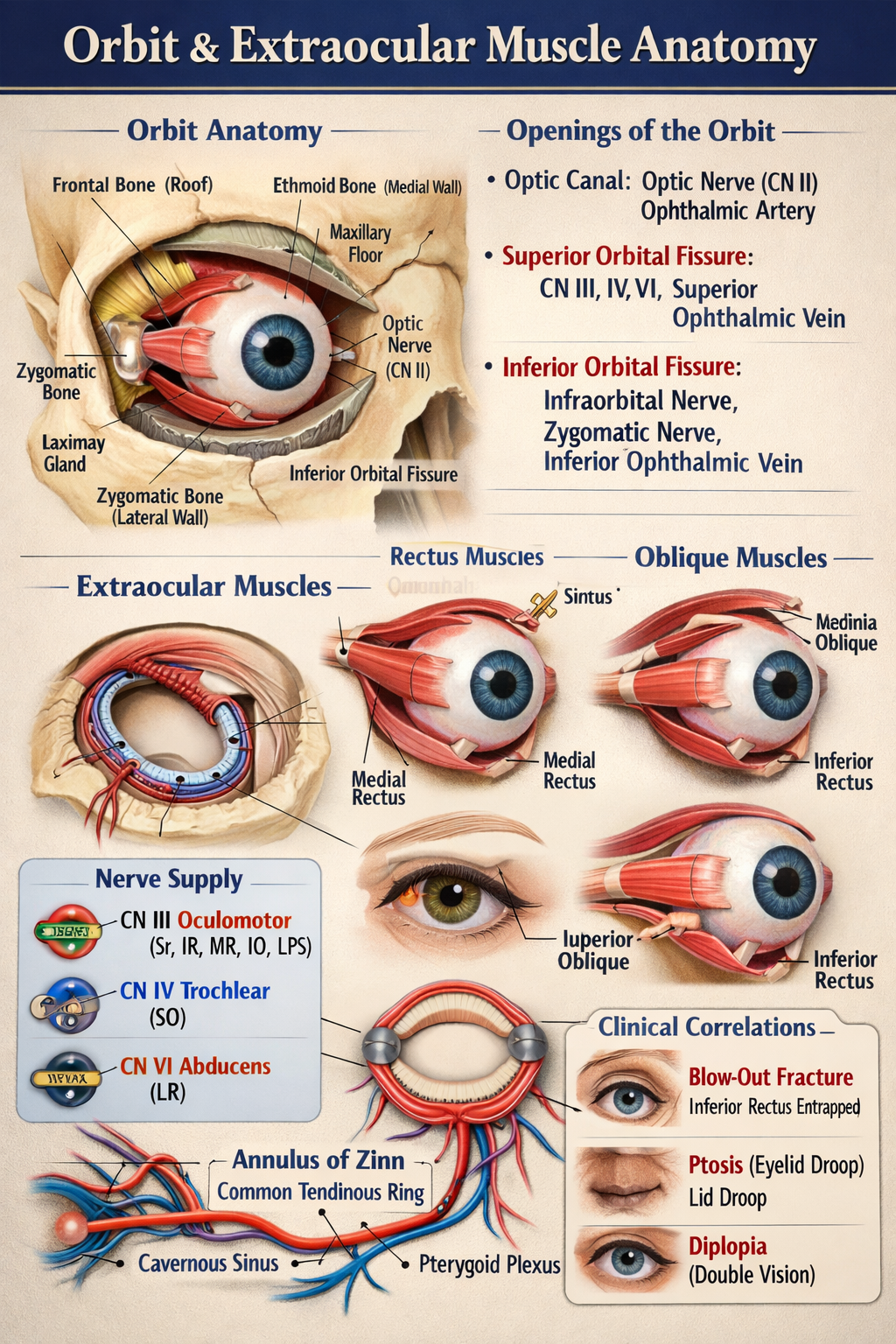
Orbit and Extraocular Muscle Anatomy Explained for Medical Students
## Orbit and Extraocular Muscle Anatomy (Detailed, No Images) --- ## 1. Orbit – Overview The **orbit** is a paired pyramidal bony cavity that houses and protects the eyeball and its associated structures. ### Contents * Eyeball (globe) * Extraocular muscles * Optic nerve (CN II) * Oculomotor (CN III), Trochlear (CN IV), Abducens (CN VI) * Ophthalmic division of trigeminal nerve (CN V1) * Lacrimal gland * Ophthalmic artery and veins * Orbital fat and connective tissue ### Shape and Orientation * **Pyramidal**: base anterior (orbital margin), apex posterior (optic canal) * Apex points medially and posteriorly --- ## 2. Bony Walls of the Orbit ### Roof **Bones:** Frontal bone, lesser wing of sphenoid **Relations:** Anterior cranial fossa, frontal sinus **Structures:** Lacrimal gland fossa, trochlear fossa ### Floor **Bones:** Maxilla, zygomatic, palatine **Relations:** Maxillary sinus **Clinical:** Most common site of blow-out fracture **Structures:** Infraorbital groove and canal ### Medial Wall **Bones:** Ethmoid (lamina papyracea), lacrimal, maxilla, sphenoid **Relations:** Ethmoidal air sinuses **Clinical:** Very thin → spread of infection ### Lateral Wall **Bones:** Zygomatic, greater wing of sphenoid **Strongest wall** **Relations:** Temporal fossa --- ## 3. Openings of the Orbit ### Optic Canal * **Contents:** Optic nerve (CN II), ophthalmic artery * **Location:** Lesser wing of sphenoid ### Superior Orbital Fissure * **Contents:** CN III, IV, V1, VI, superior ophthalmic vein * **Connects:** Middle cranial fossa ### Inferior Orbital Fissure * **Contents:** Infraorbital nerve, zygomatic nerve, inferior ophthalmic vein * **Connects:** Pterygopalatine and infratemporal fossae --- ## 4. Extraocular Muscles – Overview There are **7 extraocular muscles**: * **4 Recti:** Superior, Inferior, Medial, Lateral * **2 Obliques:** Superior, Inferior * **1 Elevator:** Levator palpebrae superioris ### Common Origin * **Annulus of Zinn (Common tendinous ring)** at orbital apex (All recti + levator palpebrae superioris) --- ## 5. Rectus Muscles ### Superior Rectus * **Origin:** Annulus of Zinn * **Insertion:** Superior sclera (anterior to equator) * **Action:** Elevation, adduction, intorsion * **Nerve:** Oculomotor nerve (CN III – superior division) ### Inferior Rectus * **Origin:** Annulus of Zinn * **Insertion:** Inferior sclera * **Action:** Depression, adduction, extorsion * **Nerve:** Oculomotor nerve (CN III – inferior division) ### Medial Rectus * **Origin:** Annulus of Zinn * **Insertion:** Medial sclera * **Action:** Adduction * **Nerve:** Oculomotor nerve (CN III) ### Lateral Rectus * **Origin:** Annulus of Zinn * **Insertion:** Lateral sclera * **Action:** Abduction * **Nerve:** Abducens nerve (CN VI) --- ## 6. Oblique Muscles ### Superior Oblique * **Origin:** Body of sphenoid * **Course:** Passes through trochlea (fibrous pulley) * **Insertion:** Posterosuperolateral sclera * **Action:** Intorsion, depression, abduction * **Nerve:** Trochlear nerve (CN IV) ### Inferior Oblique * **Origin:** Anterior orbital floor (maxilla) * **Insertion:** Posteroinferolateral sclera * **Action:** Extorsion, elevation, abduction * **Nerve:** Oculomotor nerve (CN III) --- ## 7. Levator Palpebrae Superioris * **Origin:** Lesser wing of sphenoid * **Insertion:** Upper eyelid * **Action:** Elevation of upper eyelid * **Nerve:** Oculomotor nerve (CN III – superior division) * **Sympathetic supply:** Müller’s muscle (smooth muscle component) --- ## 8. Blood Supply * **Ophthalmic artery** (branch of internal carotid) * Supplies eyeball, muscles, optic nerve ### Venous Drainage * **Superior and inferior ophthalmic veins** * Drain into cavernous sinus and pterygoid plexus --- ## 9. Nerve Supply Summary (Rule of 3-4-6) * **CN III (Oculomotor):** All extraocular muscles except SO and LR * **CN IV (Trochlear):** Superior oblique * **CN VI (Abducens):** Lateral rectus --- ## 10. Important Clinical Correlations * **Blow-out fracture:** Floor of orbit → inferior rectus entrapment * **Cavernous sinus thrombosis:** Ophthalmic veins involvement * **Ptosis:** CN III palsy or sympathetic damage * **Diplopia:** Extraocular muscle or nerve dysfunction --- If you want, I can next provide **nerve lesions with eye deviation patterns**, **muscle action tables**, **MCQs**, or **SEO-optimized medical content format** for this topic.
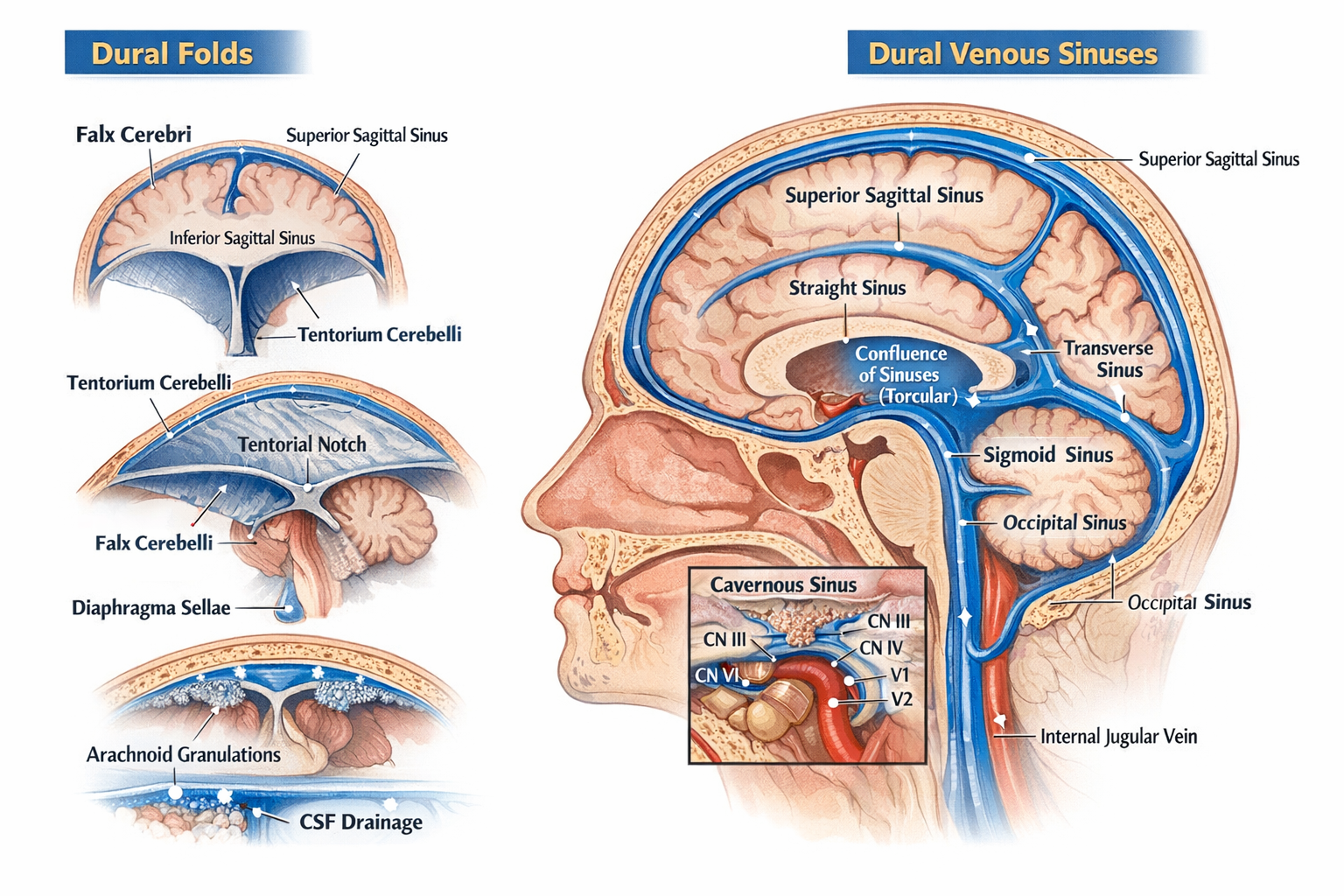
Dural Folds and Dural Venous Sinuses Anatomy, Features and Clinical Significance
## Dural Folds and Dural Venous Sinuses — Complete, Exam-Oriented Anatomy Guide (No Images) --- ## 1. Dura Mater: Brief Context The **dura mater** is the outermost meningeal layer of the brain. It has **two layers**: * **Periosteal (endosteal) layer** – lines the inner surface of the skull * **Meningeal layer** – forms inward folds (**dural folds**) Where these two layers separate, **dural venous sinuses** are formed. 🔗 *Related topic:* [Meninges of Brain](#) --- ## 2. Dural Folds (Dural Septa) Dural folds are **double-layered reflections of meningeal dura mater** that: * Stabilize the brain * Limit excessive movement * Contain venous sinuses at their attachments ### 2.1 Falx Cerebri A **sickle-shaped vertical fold** in the midline. **Attachments** * Anterior: Crista galli of ethmoid * Posterior: Internal occipital protuberance (joins tentorium cerebelli) **Separates** * Right and left cerebral hemispheres **Venous Sinuses Contained** * Superior sagittal sinus (upper border) * Inferior sagittal sinus (free lower border) * Straight sinus (posterior attachment) **Clinical relevance** * Falx meningioma * Subfalcine herniation 🔗 *See also:* [Cerebral Herniation Syndromes](#) --- ### 2.2 Tentorium Cerebelli A **horizontal tent-like fold**. **Attachments** * Anterior: Clinoid processes * Lateral: Superior border of petrous temporal bone * Posterior: Occipital bone **Separates** * Cerebrum (above) from cerebellum (below) **Opening** * Tentorial notch → passage for midbrain **Venous Sinuses Contained** * Transverse sinus * Superior petrosal sinus * Straight sinus (junction with falx cerebri) **Clinical relevance** * Transtentorial (uncal) herniation * Compression of oculomotor nerve 🔗 *Related topic:* [Midbrain Anatomy](#) --- ### 2.3 Falx Cerebelli A **small vertical fold** below the tentorium. **Attachments** * Internal occipital crest **Separates** * Two cerebellar hemispheres (partially) **Venous Sinus** * Occipital sinus --- ### 2.4 Diaphragma Sellae A **small circular dural fold** forming the roof of sella turcica. **Central opening** * Allows passage of pituitary stalk (infundibulum) **Clinical relevance** * Pituitary adenoma expansion * CSF leak after trans-sphenoidal surgery 🔗 *See also:* [Pituitary Gland Anatomy](#) --- ## 3. Dural Venous Sinuses ### Definition **Endothelial-lined venous channels** between layers of dura mater that drain venous blood from brain, meninges, and skull. **Key characteristics** * No valves * No muscular layer * Rigid walls (do not collapse) --- ## 4. Classification of Dural Venous Sinuses ### 4.1 Unpaired Sinuses #### Superior Sagittal Sinus * Location: Upper margin of falx cerebri * Drains: Cerebral veins, CSF via arachnoid granulations * Ends in: Confluence of sinuses **Clinical** * Site of CSF absorption * Thrombosis → raised intracranial pressure --- #### Inferior Sagittal Sinus * Location: Free lower margin of falx cerebri * Drains into: Straight sinus --- #### Straight Sinus * Formed by union of inferior sagittal sinus + great cerebral vein (of Galen) * Ends in: Confluence of sinuses --- #### Occipital Sinus * Smallest sinus * Located in falx cerebelli --- ### 4.2 Paired Sinuses #### Transverse Sinuses * Located along posterolateral margin of tentorium * Drain into: Sigmoid sinuses --- #### Sigmoid Sinuses * S-shaped * Continue as: Internal jugular veins 🔗 *Related topic:* [Internal Jugular Vein](#) --- #### Cavernous Sinus (Highly Important) Located on either side of body of sphenoid. **Contents** * Internal carotid artery * CN VI (abducent nerve) **Lateral wall (superior to inferior)** * CN III * CN IV * V1 * V2 **Drains** * Superior & inferior ophthalmic veins **Clinical** * Cavernous sinus thrombosis * Carotid–cavernous fistula 🔗 *See also:* [Cranial Nerves in Cavernous Sinus](#) --- #### Petrosal Sinuses * **Superior petrosal sinus**: cavernous → transverse * **Inferior petrosal sinus**: cavernous → internal jugular vein --- ## 5. Confluence of Sinuses (Torcular Herophili) * Located at internal occipital protuberance * Receives: * Superior sagittal sinus * Straight sinus * Occipital sinus * Drains into: Transverse sinuses --- ## 6. CSF Drainage and Arachnoid Granulations * CSF absorbed into **superior sagittal sinus** * Via arachnoid villi and granulations 🔗 *Related topic:* [CSF Circulation and Absorption](#) --- ## 7. Clinical Correlation Summary | Condition | Related Structure | | ----------------- | -------------------------- | | Raised ICP | Superior sagittal sinus | | Uncal herniation | Tentorium cerebelli | | Diplopia | Cavernous sinus (CN VI) | | CSF leak | Diaphragma sellae | | Venous thrombosis | Sagittal / cavernous sinus | --- ## 8. One-Line Exam Pearls * Dural folds are formed by **meningeal dura only** * Venous sinuses lack valves and smooth muscle * Cavernous sinus is the **only sinus containing cranial nerves** * Falx cerebri contains **two sagittal sinuses** --- If you want, I can next provide: * **SEO title, meta description, and long-tail keywords** * **20 hard MCQs (including case-based)** * **FAQ schema JSON** * **Internal link structure optimized for a medical website**
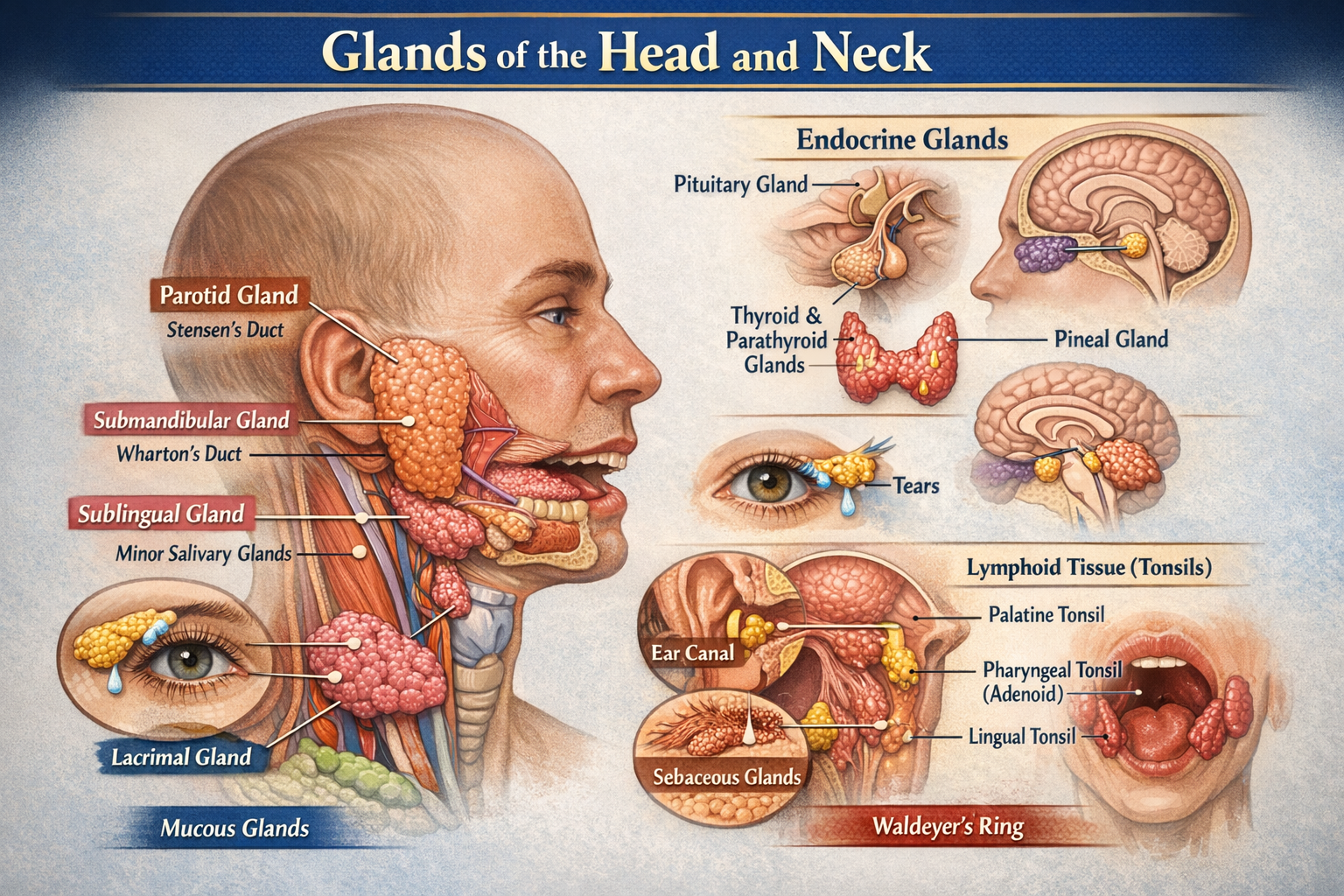
Glands of Head and Neck Anatomy Types Functions and Clinical Importance
Below is a **clear, exam-oriented yet complete description of the glands in the head and neck**, **without images**, suitable for **medical students, anatomy revision, and clinical correlation**. --- # Glands of the Head and Neck – Detailed Anatomy Glands in the head and neck are primarily **exocrine glands** involved in **saliva production, lubrication, immunity, thermoregulation, and endocrine regulation**. They are classified into **salivary glands, endocrine glands, mucous glands, sebaceous glands, and specialized glands**. --- ## I. SALIVARY GLANDS Responsible for saliva secretion → lubrication, digestion (amylase), oral hygiene. ### A. Major Salivary Glands #### 1. Parotid Gland * **Largest salivary gland** * **Type:** Pure serous * **Location:** * In the **parotid bed** * Anterior to ear, posterior to ramus of mandible * **Relations (Superficial to deep):** * Skin → fascia → facial nerve → retromandibular vein → external carotid artery * **Duct:** Stensen’s duct * Opens opposite **upper second molar** * **Nerve supply:** * Parasympathetic: Glossopharyngeal nerve (CN IX) via **otic ganglion** * **Clinical relevance:** * Parotitis (mumps) * Facial nerve injury during surgery --- #### 2. Submandibular Gland * **Type:** Mixed (predominantly serous) * **Location:** * Submandibular triangle * Superficial and deep parts around **mylohyoid muscle** * **Duct:** Wharton’s duct * Opens at **sublingual papilla** * **Nerve supply:** * Parasympathetic: Facial nerve (CN VII) via **chorda tympani** * **Clinical relevance:** * Common site of **salivary stones (sialolithiasis)** --- #### 3. Sublingual Gland * **Smallest major gland** * **Type:** Mixed (predominantly mucous) * **Location:** * Floor of mouth * Beneath mucosa, above mylohyoid * **Ducts:** Multiple ducts of Rivinus * **Nerve supply:** * Facial nerve (CN VII) * **Clinical relevance:** * Ranula (mucous cyst) --- ### B. Minor Salivary Glands * Numerous small glands embedded in mucosa * **Locations:** * Lips * Cheeks * Tongue * Soft palate * **Type:** Mostly mucous * **Clinical importance:** * Tumors (often malignant) --- ## II. ENDOCRINE GLANDS OF HEAD AND NECK ### 1. Thyroid Gland * **Largest endocrine gland** * **Location:** * Anterior neck * Opposite C5–T1 vertebrae * **Structure:** * Two lobes + isthmus * **Hormones:** * T3, T4 → metabolism * Calcitonin → calcium regulation * **Blood supply:** * Superior thyroid artery * Inferior thyroid artery * **Clinical relevance:** * Goiter * Hypothyroidism, hyperthyroidism --- ### 2. Parathyroid Glands * Usually **four glands** * **Location:** * Posterior surface of thyroid * **Hormone:** * Parathyroid hormone (PTH) * **Function:** * Increases blood calcium * **Clinical relevance:** * Hypocalcemia after thyroid surgery --- ### 3. Pituitary Gland * **Master endocrine gland** * **Location:** * Sella turcica of sphenoid bone * **Divisions:** * Anterior pituitary * Posterior pituitary * **Function:** * Controls growth, reproduction, stress response * **Clinical relevance:** * Pituitary adenomas --- ### 4. Pineal Gland * **Location:** * Roof of third ventricle * **Hormone:** * Melatonin * **Function:** * Circadian rhythm regulation --- ## III. MUCOUS GLANDS ### Nasal Glands * Found in nasal mucosa * Produce mucus to humidify air ### Palatine Glands * Located in soft palate * Lubricate food during swallowing --- ## IV. SEBACEOUS GLANDS * Associated with hair follicles * Abundant on: * Face * Scalp * Produce **sebum** * **Clinical relevance:** * Acne vulgaris * Sebaceous cysts --- ## V. SWEAT GLANDS (MODIFIED) ### Ceruminous Glands * Located in **external auditory canal** * Produce **ear wax (cerumen)** * Protect tympanic membrane --- ## VI. SPECIALIZED GLANDS ### Lacrimal Gland * Produces tears * Located in **superolateral orbit** * Drains into conjunctival sac * **Clinical relevance:** Dry eye syndrome --- ## VII. LYMPHOID GLANDULAR STRUCTURES ### Tonsils (Waldeyer’s Ring) * Palatine tonsils * Pharyngeal tonsil (adenoids) * Lingual tonsils * Function: Immune defense --- ## SUMMARY TABLE | Gland | Type | Function | | ------------- | --------- | ---------------- | | Parotid | Serous | Saliva (amylase) | | Submandibular | Mixed | Saliva | | Sublingual | Mucous | Lubrication | | Thyroid | Endocrine | Metabolism | | Parathyroid | Endocrine | Calcium balance | | Pituitary | Endocrine | Hormonal control | | Lacrimal | Exocrine | Tear secretion | --- If you want next: * **SEO-friendly version** * **MCQs (case-based)** * **FAQ JSON schema** * **Embryological development** * **Clinical correlations only** Just tell me 👍
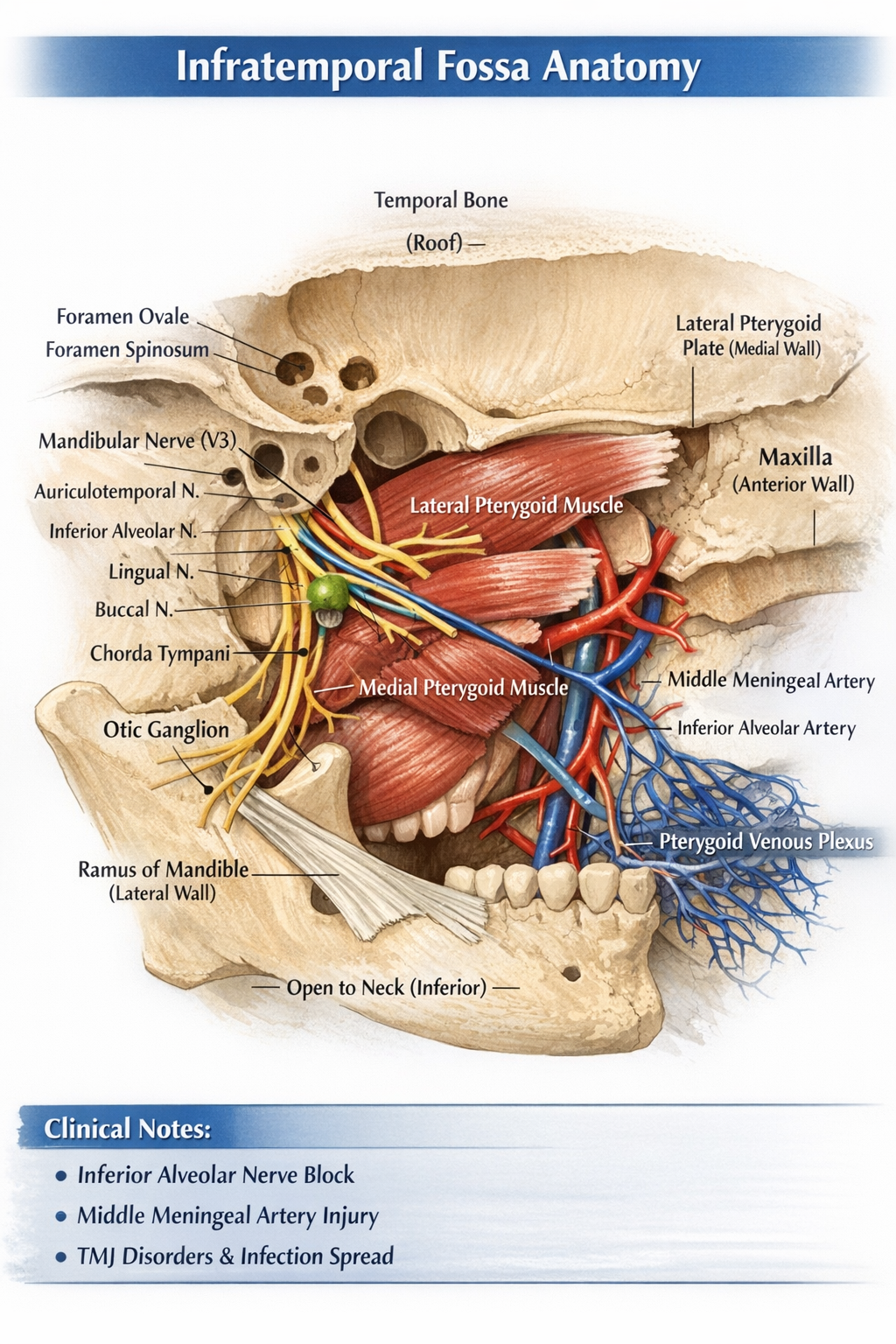
Infratemporal Fossa Anatomy Boundaries Contents Nerves Vessels and Clinical Importance
## Infratemporal Fossa – Detailed Anatomy (No Images) ### **Definition** The **infratemporal fossa** is an irregular, wedge-shaped deep space located **below the base of the skull**, **medial to the ramus of the mandible**, and **posterior to the maxilla**. It is a major neurovascular and muscular compartment involved in **mastication, facial sensation, and cranial–facial circulation**. --- ## **Boundaries** ### **Roof (Superior)** * **Infratemporal surface of greater wing of sphenoid** * **Squamous part of temporal bone** * Contains: * **Foramen ovale** – mandibular nerve (V3), accessory meningeal artery, lesser petrosal nerve * **Foramen spinosum** – middle meningeal artery and vein, meningeal branch of V3 ### **Lateral Wall** * **Ramus of mandible** ### **Medial Wall** * **Lateral pterygoid plate (sphenoid)** * **Tensor veli palatini muscle** ### **Anterior Wall** * **Posterior surface of maxilla** ### **Posterior Wall** * **Tympanic plate** * **Mastoid and styloid processes of temporal bone** * Separates infratemporal fossa from **parotid region** ### **Inferior Boundary** * **Open** (continuous with tissues of the neck) --- ## **Contents** ### **Muscles of Mastication** 1. **Medial pterygoid** * Origin: medial surface of lateral pterygoid plate * Insertion: medial surface of mandibular angle * Action: elevation and protrusion of mandible 2. **Lateral pterygoid** * Two heads: * Superior: greater wing of sphenoid * Inferior: lateral pterygoid plate * Insertion: neck of mandible and TMJ disc * Action: depression, protrusion, lateral movement of mandible 3. **Lower part of temporalis** (tendon passing through fossa) --- ## **Nerves** ### **Mandibular Nerve (V3) – Main Nerve** Exits skull via **foramen ovale** #### **Branches** * **Auriculotemporal nerve** – sensation to temporal region and TMJ * **Inferior alveolar nerve** * Gives **nerve to mylohyoid** * Enters mandibular foramen * **Lingual nerve** – general sensation to anterior 2/3 of tongue * **Buccal nerve** – sensory to cheek * **Motor branches** to muscles of mastication ### **Chorda Tympani (Facial nerve branch)** * Joins lingual nerve * Carries: * Taste fibers (anterior 2/3 of tongue) * Parasympathetic fibers to submandibular and sublingual glands ### **Otic Ganglion** * Parasympathetic ganglion * Related to mandibular nerve * Secretomotor supply to **parotid gland** via auriculotemporal nerve --- ## **Arteries** ### **Maxillary Artery (Terminal branch of external carotid)** Major arterial content of infratemporal fossa #### **Branches (Mandibular Part)** * **Deep auricular artery** * **Anterior tympanic artery** * **Middle meningeal artery** * **Accessory meningeal artery** * **Inferior alveolar artery** --- ## **Veins** ### **Pterygoid Venous Plexus** * Extensive venous network * Drains into **maxillary vein** * Communicates with: * Cavernous sinus (via emissary veins) * Clinical relevance: spread of infection --- ## **Ligaments** * **Sphenomandibular ligament** * Extends from spine of sphenoid to lingula of mandible * Separates inferior alveolar nerve from lingual nerve --- ## **Communications** | Communication | Opening | Connects With | | --------------------- | ------------------------ | ------------------------------ | | Middle cranial fossa | Foramen ovale | V3, lesser petrosal nerve | | Middle cranial fossa | Foramen spinosum | Middle meningeal artery | | Pterygopalatine fossa | Pterygomaxillary fissure | Maxillary nerve and vessels | | Orbit | Inferior orbital fissure | Infraorbital nerve and vessels | | Temporal fossa | Deep to zygomatic arch | Temporalis muscle | --- ## **Clinical Importance** * **Inferior alveolar nerve block** administered in infratemporal fossa * **Middle meningeal artery injury** → extradural hematoma * **TMJ disorders** involve lateral pterygoid * **Spread of infection** via pterygoid venous plexus to cavernous sinus * **Trigeminal neuralgia** may involve V3 branches --- ## **Summary** The infratemporal fossa is a complex anatomical space housing **muscles of mastication, the mandibular nerve and its branches, maxillary artery, pterygoid venous plexus, and parasympathetic ganglia**. It plays a crucial role in **chewing, facial sensation, salivation, and cranial circulation**, and is of high **clinical and surgical significance**. If you want, I can also provide **SEO title, MCQs (case-based), FAQ JSON, or exam-oriented tables** for this topic.
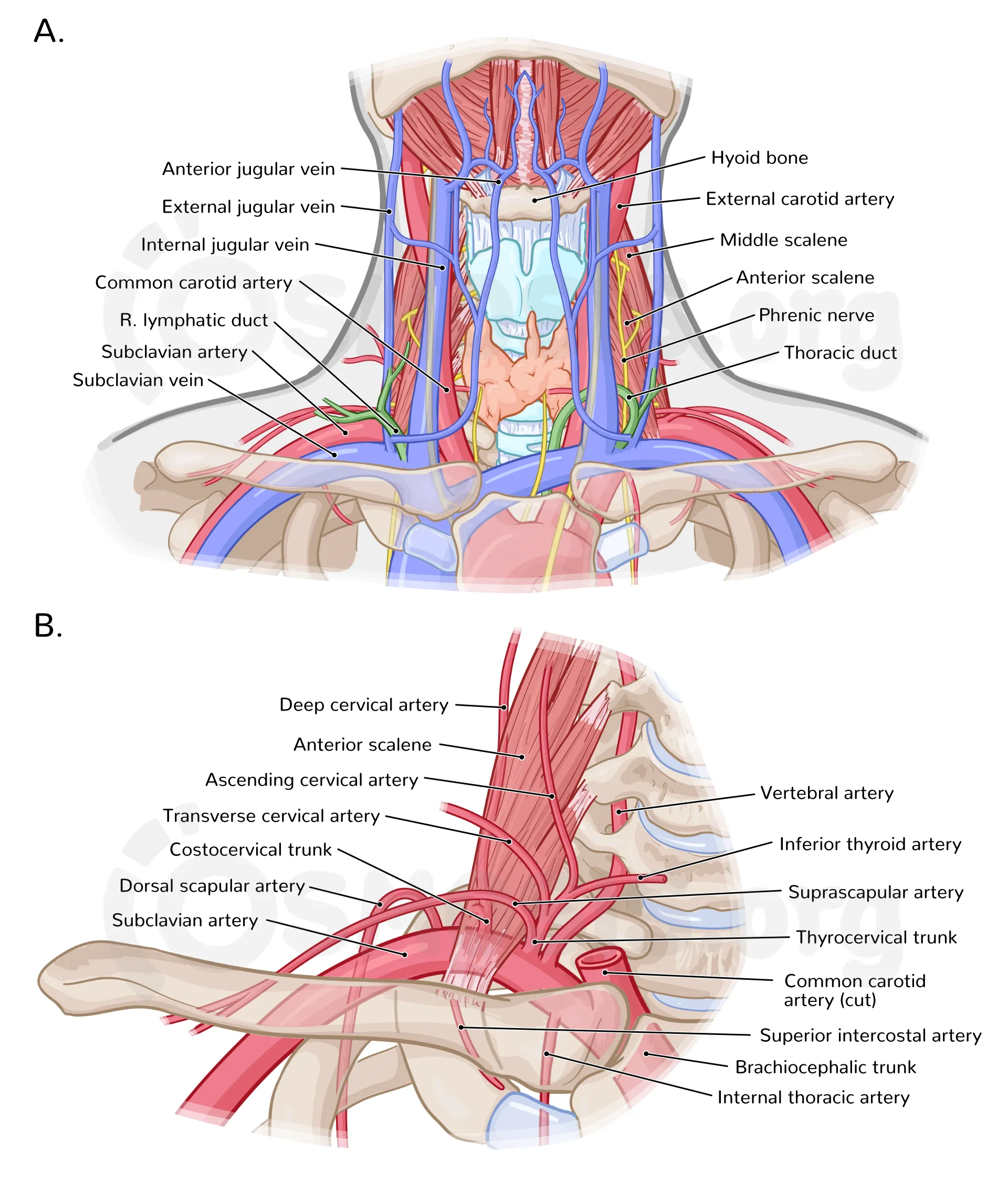
Neurovascular Structures of the Neck Anatomy Clinical Importance and Exam Guide
Below is a **concise but complete, exam-oriented explanation** of **neurovascular structures of the neck**, written **without images**, covering **arteries, veins, nerves, and key clinical correlations** in one place. --- ## Neurovascular Structures of the Neck The neck contains vital **arterial, venous, and neural structures** that connect the brain with the rest of the body. These structures are arranged in **distinct fascial compartments**, most importantly within the **carotid sheath**. --- ## 1. Arterial Structures of the Neck ### A. Common Carotid Arteries (CCA) * **Origin** * Right: From **brachiocephalic trunk** * Left: From **arch of aorta** * **Course** * Ascend in the neck within the **carotid sheath** * Divide at **C4 vertebral level** (upper border of thyroid cartilage) * **Termination** * External carotid artery * Internal carotid artery --- ### B. External Carotid Artery (ECA) * Supplies **structures of face, scalp, neck** * Lies **anteromedial** to internal carotid initially **Branches (Mnemonic: *Some Angry Lady Figured Out PMS*)** 1. Superior thyroid 2. Ascending pharyngeal 3. Lingual 4. Facial 5. Occipital 6. Posterior auricular 7. Maxillary 8. Superficial temporal --- ### C. Internal Carotid Artery (ICA) * Supplies **brain and eye** * **No branches in the neck** * Enters skull via **carotid canal** * Clinical importance: **stroke, carotid stenosis** --- ### D. Subclavian Artery (Neck Part) **Major branches** * Vertebral artery → brainstem, posterior brain * Thyrocervical trunk * Costocervical trunk --- ## 2. Venous Structures of the Neck ### A. Internal Jugular Vein (IJV) * Drains **brain, face, neck** * Lies **lateral to common carotid artery** * Joins subclavian vein → **brachiocephalic vein** * Important landmark for **central venous access** --- ### B. External Jugular Vein (EJV) * Drains scalp and face * Superficial, crosses sternocleidomastoid * Visible in raised venous pressure --- ### C. Anterior Jugular Veins * Drain submental region * May form **jugular venous arch** --- ## 3. Neural Structures of the Neck ### A. Cranial Nerves in the Neck #### 1. Vagus Nerve (CN X) * Lies **between carotid artery and jugular vein** * Supplies: * Parasympathetic to thoracic and abdominal organs * Laryngeal branches (voice) #### 2. Glossopharyngeal Nerve (CN IX) * Supplies: * Stylopharyngeus * Taste posterior 1/3 tongue * Carotid body & sinus #### 3. Accessory Nerve (CN XI) * Supplies: * Sternocleidomastoid * Trapezius * Vulnerable during **neck surgeries** #### 4. Hypoglossal Nerve (CN XII) * Motor to tongue muscles * Injury causes **tongue deviation** --- ### B. Cervical Plexus (C1–C4) * Located deep to sternocleidomastoid * **Sensory branches** * Lesser occipital * Great auricular * Transverse cervical * Supraclavicular * **Motor branches** * Ansa cervicalis → infrahyoid muscles * Phrenic nerve (C3–C5) → diaphragm --- ### C. Brachial Plexus (Neck Part) * Roots: **C5–T1** * Lies between **anterior and middle scalene muscles** * Supplies **upper limb** --- ### D. Sympathetic Trunk * Lies posterior to carotid sheath * Cervical ganglia: * Superior * Middle * Inferior (stellate) * Injury → **Horner syndrome** * Ptosis * Miosis * Anhidrosis --- ## 4. Carotid Sheath – Core Neurovascular Bundle ### Contents * Common/Internal carotid artery (medial) * Internal jugular vein (lateral) * Vagus nerve (posterior) * Deep cervical lymph nodes * Carotid plexus (sympathetic fibers) ### Clinical relevance * Carotid endarterectomy * Central line placement * Neck trauma --- ## 5. Important Clinical Correlations * **Carotid sinus**: Baroreceptor → BP regulation * **Carotid body**: Chemoreceptor → oxygen sensing * **Neck hematoma**: Can compress airway * **Surgical risk**: Accessory nerve injury → shoulder droop --- ## Quick Summary Table | Structure | Function | | ----------------- | ------------------------- | | Carotid arteries | Brain & face blood supply | | Jugular veins | Venous drainage of head | | Vagus nerve | Parasympathetic, voice | | Cervical plexus | Neck sensation & movement | | Sympathetic trunk | Autonomic control | --- If you want next: * **Exam-oriented MCQs** * **Clinical case-based questions** * **SEO-optimized version** * **FAQ JSON** * **HTML/CSS/JS interactive content** Just tell me.
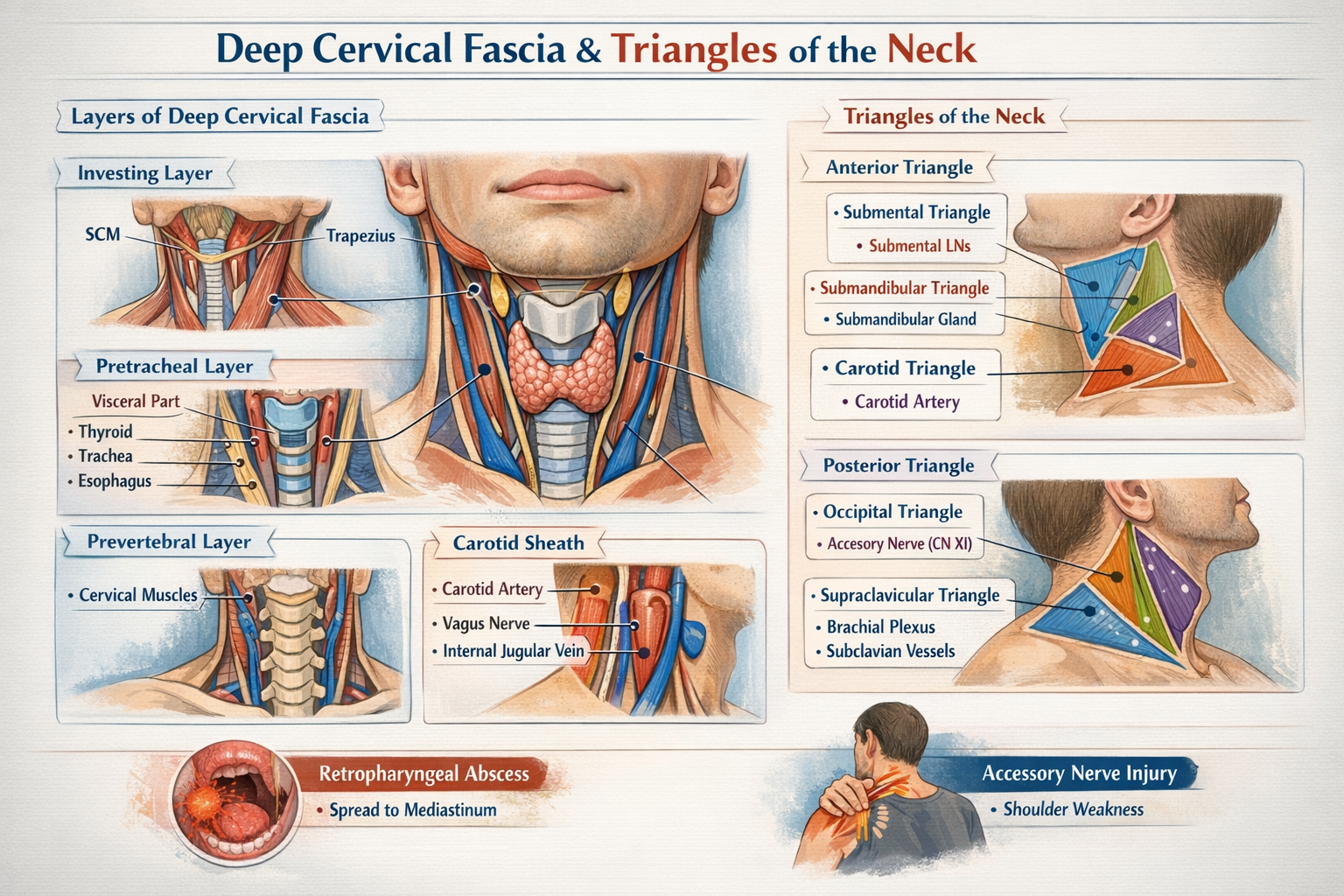
Deep Cervical Fascia and Triangles of the Neck Anatomy Explained in Detail
## Deep Cervical Fascia and Triangles of the Neck — Detailed Anatomical Guide --- # **Deep Cervical Fascia** ### **Definition** The **deep cervical fascia** is a dense connective tissue layer in the neck that surrounds, supports, and compartmentalizes muscles, vessels, nerves, and viscera. It plays a critical role in structural support, movement coordination, and containment of infections. --- ## **Layers of Deep Cervical Fascia** ### **1. Investing Layer (Superficial Layer of Deep Fascia)** **Extent** * Encloses the entire neck like a collar * Splits to surround **sternocleidomastoid (SCM)** and **trapezius** * Extends: * Superiorly: superior nuchal line, mandible, zygomatic arch * Inferiorly: clavicle, sternum, acromion **Attachments** * Mastoid process * External occipital protuberance * Lower border of mandible * Spine of scapula **Structures Enclosed** * SCM * Trapezius * Parotid gland (forms parotid fascia) * Submandibular gland (forms submandibular fascia) **Clinical Importance** * Limits superficial spread of infection * Parotid abscess causes severe pain due to tight fascia * Forms stylomandibular ligament --- ### **2. Pretracheal Layer** Divided into **muscular** and **visceral** parts. #### **A. Muscular Part** **Encloses** * Infrahyoid (strap) muscles: * Sternohyoid * Sternothyroid * Thyrohyoid * Omohyoid **Extent** * Hyoid bone → superior mediastinum --- #### **B. Visceral Part** **Encloses** * Thyroid gland * Trachea * Esophagus **Special Features** * Forms **false capsule of thyroid** * Thickened posteriorly to form **Berry’s ligament** (anchors thyroid to cricoid cartilage) **Clinical Importance** * Explains movement of thyroid gland during swallowing * Thyroid swelling moves with deglutition --- ### **3. Prevertebral Layer** **Extent** * Base of skull → T3 vertebra **Encloses** * Cervical vertebrae * Deep neck muscles: * Longus colli * Longus capitis * Scalene muscles * Vertebral vessels * Cervical sympathetic trunk **Lateral Extension** * Forms **axillary sheath**, enclosing: * Subclavian artery * Brachial plexus **Clinical Importance** * Infection here can spread to posterior mediastinum * Involvement affects neck movements --- ### **4. Carotid Sheath** A tubular condensation of deep cervical fascia formed by: * Investing layer * Pretracheal layer * Prevertebral layer **Extent** * Base of skull → root of neck **Contents** * Common carotid artery (internal carotid above bifurcation) * Internal jugular vein * Vagus nerve * Deep cervical lymph nodes * Sympathetic fibers **Arrangement** * Artery: medial * Vein: lateral * Nerve: posterior **Clinical Importance** * Compression can affect cerebral blood flow * Infections can spread vertically --- ## **Spaces Formed by Deep Cervical Fascia** * **Pretracheal space** → anterior mediastinum * **Retropharyngeal space** → posterior mediastinum (danger space) * **Prevertebral space** → posterior mediastinum --- # **Triangles of the Neck** The neck is divided by **sternocleidomastoid (SCM)** into **anterior** and **posterior triangles**. --- ## **Anterior Triangle** ### **Boundaries** * Medial: midline of neck * Lateral: anterior border of SCM * Superior: lower border of mandible * Apex: suprasternal notch ### **Roof** * Skin * Superficial fascia * Platysma * Investing layer of deep fascia ### **Floor** * Pharynx * Larynx * Thyroid gland --- ### **Subdivisions of Anterior Triangle** --- ### **1. Submental Triangle** **Boundaries** * Two anterior bellies of digastric * Base: body of hyoid **Contents** * Submental lymph nodes * Small veins forming anterior jugular vein **Clinical Importance** * Drains lower lip, chin, tip of tongue --- ### **2. Submandibular (Digastric) Triangle** **Boundaries** * Anterior and posterior bellies of digastric * Lower border of mandible **Contents** * Submandibular gland * Facial artery and vein * Hypoglossal nerve * Submandibular lymph nodes --- ### **3. Carotid Triangle** **Boundaries** * Posterior belly of digastric * Superior belly of omohyoid * Anterior border of SCM **Contents** * Common carotid artery and bifurcation * Internal and external carotid arteries * Internal jugular vein * Vagus nerve * Hypoglossal nerve * Carotid sinus and body **Clinical Importance** * Site for carotid pulse * Carotid endarterectomy --- ### **4. Muscular Triangle** **Boundaries** * Midline of neck * Anterior border of SCM * Superior belly of omohyoid **Contents** * Infrahyoid muscles * Thyroid and parathyroid glands * Larynx * Trachea --- ## **Posterior Triangle** ### **Boundaries** * Anterior: posterior border of SCM * Posterior: anterior border of trapezius * Inferior: clavicle * Apex: where SCM and trapezius meet ### **Roof** * Skin * Superficial fascia * Platysma * Investing layer of deep fascia ### **Floor** * Splenius capitis * Levator scapulae * Scalene muscles --- ### **Subdivision of Posterior Triangle** --- ### **1. Occipital Triangle** **Boundaries** * SCM * Trapezius * Inferior belly of omohyoid **Contents** * Spinal accessory nerve (CN XI) * Cervical plexus branches * Occipital artery * Lymph nodes **Clinical Importance** * CN XI injury causes shoulder droop --- ### **2. Supraclavicular (Subclavian) Triangle** **Boundaries** * Clavicle * SCM * Inferior belly of omohyoid **Contents** * Subclavian artery and vein * Brachial plexus trunks * Supraclavicular lymph nodes **Clinical Importance** * Venous access * Pancoast tumor involvement --- ## **Key Clinical Correlations (High-Yield)** * Deep cervical fascia directs spread of neck infections * Retropharyngeal abscess can descend into mediastinum * Thyroid movement with swallowing explained by pretracheal fascia * Accessory nerve vulnerability in posterior triangle * Carotid sheath protects vital neurovascular structures --- If you want, I can also provide: * **SEO-optimized title, description, keywords** * **Hard MCQs with case-based questions (HTML/CSS/JS)** * **FAQ in JSON schema format** * **One-page exam revision notes** Just tell me 👍
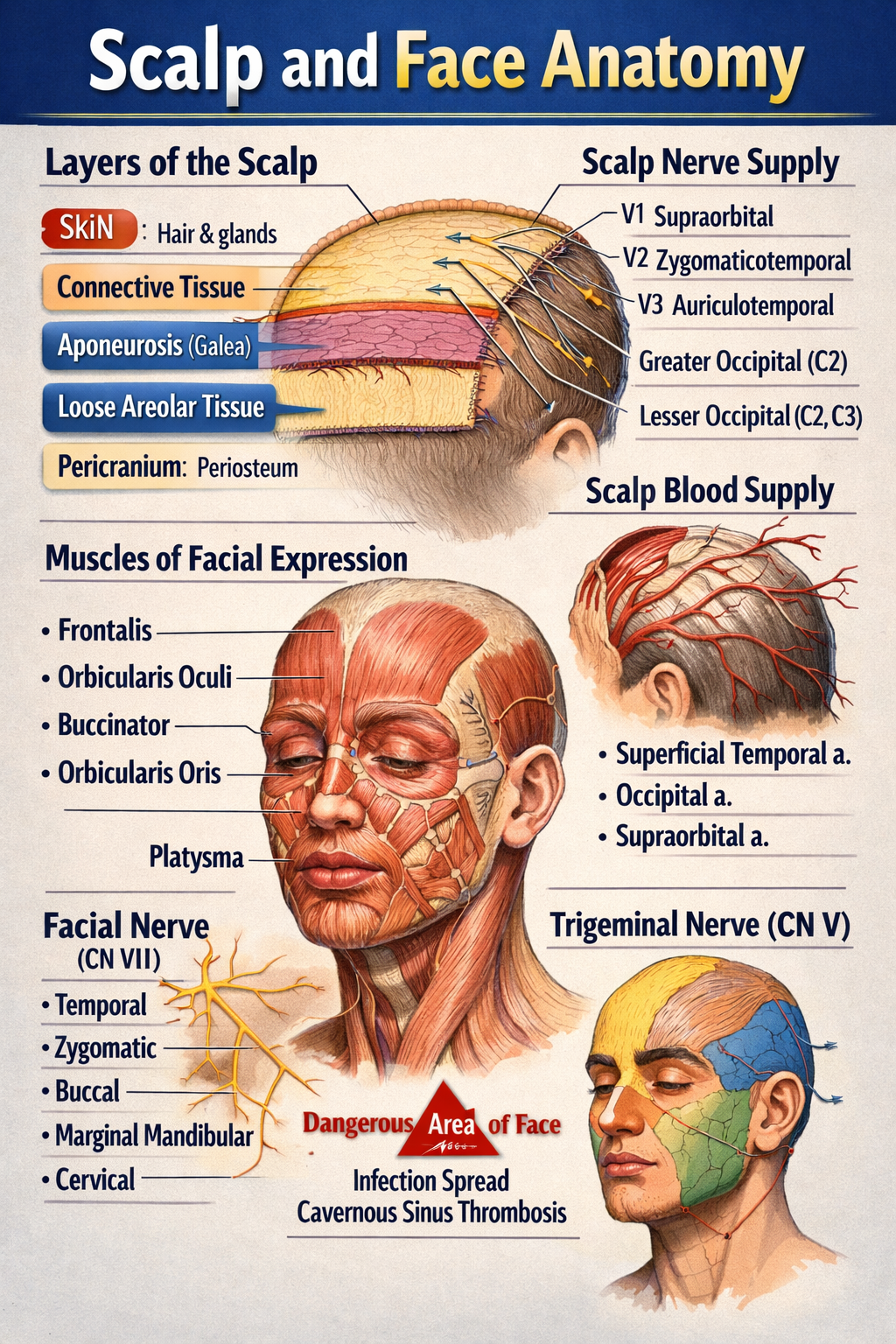
Scalp and Face Anatomy Complete Structure Nerves Blood Supply and Clinical Correlation
Below is a **complete, structured, exam-oriented yet clinically relevant explanation of SCALP AND FACE ANATOMY** — **text only, no images**, written clearly for medical students and healthcare learners. --- # SCALP AND FACE ANATOMY – COMPLETE DETAILED GUIDE --- ## PART A: SCALP ANATOMY ### 1. Definition The **scalp** is the soft tissue covering the cranial vault, extending: * **Anteriorly**: up to the supraorbital margins * **Posteriorly**: to the superior nuchal lines * **Laterally**: to the zygomatic arches --- ### 2. Layers of the Scalp (Mnemonic: **SCALP**) 1. **S – Skin** * Thick, hair-bearing * Rich in sebaceous and sweat glands * Contains hair follicles * Highly vascular → profuse bleeding from cuts 2. **C – Connective Tissue (Dense)** * Fibrofatty layer * Contains **blood vessels and nerves** * Vessels are fixed → cannot retract → excessive bleeding 3. **A – Aponeurosis (Galea Aponeurotica)** * Tough fibrous sheet * Connects: * **Frontalis muscle (anterior)** * **Occipitalis muscle (posterior)** * Lacerations here gape widely 4. **L – Loose Areolar Tissue** * Also called **“danger area of scalp”** * Allows movement of upper 3 layers * Contains emissary veins → connects scalp veins to intracranial venous sinuses * Infection may spread → **cavernous sinus thrombosis / meningitis** 5. **P – Pericranium** * Periosteum covering skull bones * Loosely attached except at sutures * Subperiosteal hematoma limited by sutures --- ### 3. Muscles of the Scalp **Occipitofrontalis muscle** * Frontal belly: elevates eyebrows, wrinkles forehead * Occipital belly: retracts scalp * Innervation: **Facial nerve (CN VII)** --- ### 4. Blood Supply of Scalp #### Arteries (ECA + ICA branches) * **From External Carotid Artery** * Superficial temporal artery * Posterior auricular artery * Occipital artery * **From Internal Carotid Artery (Ophthalmic branch)** * Supraorbital artery * Supratrochlear artery --- ### 5. Venous Drainage * Superficial temporal vein * Posterior auricular vein * Occipital vein → drain into **external jugular vein** **Emissary veins** * Connect extracranial veins to intracranial sinuses * Pathway for infection spread --- ### 6. Nerve Supply of Scalp #### Sensory (Trigeminal + Cervical nerves) * **Anterior to auricle** * Supraorbital nerve (V1) * Supratrochlear nerve (V1) * Zygomaticotemporal nerve (V2) * Auriculotemporal nerve (V3) * **Posterior to auricle** * Greater occipital nerve (C2) * Lesser occipital nerve (C2) * Third occipital nerve (C3) #### Motor * Facial nerve (CN VII) → occipitofrontalis --- ### 7. Applied Anatomy of Scalp * Scalp wounds bleed profusely * Loose areolar tissue → danger area * Cephalhematoma (subperiosteal) * Caput succedaneum (superficial swelling) --- --- ## PART B: FACE ANATOMY --- ### 1. Definition The **face** is the anterior part of the head extending: * From the hairline to the chin * Between the ears laterally --- ### 2. Muscles of Facial Expression * Derived from **second pharyngeal arch** * Insert into skin → facial expressions * Supplied by **Facial nerve (CN VII)** #### Major Groups **Orbital group** * Orbicularis oculi (closes eye) **Oral group** * Orbicularis oris (closes mouth) * Buccinator (cheek muscle) **Nasal group** * Nasalis * Levator labii superioris alaeque nasi --- ### 3. Blood Supply of Face #### Arteries (External Carotid mainly) * Facial artery * Superficial temporal artery * Maxillary artery **Dangerous area of face** * Upper lip, nose, medial cheek * Infection may spread via angular vein → cavernous sinus --- ### 4. Venous Drainage of Face * Facial vein * Angular vein * Retromandibular vein **Communicates with cavernous sinus via** * Ophthalmic veins --- ### 5. Nerve Supply of Face #### Sensory – Trigeminal Nerve (CN V) * **Ophthalmic (V1)**: forehead, upper eyelid * **Maxillary (V2)**: cheek, upper lip * **Mandibular (V3)**: lower lip, chin #### Motor – Facial Nerve (CN VII) Branches within parotid gland: * Temporal * Zygomatic * Buccal * Marginal mandibular * Cervical (Mnemonic: **To Zanzibar By Motor Car**) --- ### 6. Lymphatic Drainage of Face * Submental nodes (chin, lower lip) * Submandibular nodes (cheeks, upper lip) * Preauricular nodes (lateral face) --- ### 7. Skin of Face * Thin, highly vascular * Rich sebaceous glands * Heals well with minimal scarring --- ### 8. Applied Anatomy of Face * Bell’s palsy → facial nerve paralysis * Trigeminal neuralgia * Cavernous sinus thrombosis * Facial nerve injury during parotid surgery * Acne common due to sebaceous glands --- ## QUICK EXAM SUMMARY * **Scalp layers**: Skin, Connective tissue, Aponeurosis, Loose areolar tissue, Pericranium * **Danger areas**: Loose areolar tissue of scalp, Central face * **Motor nerve of face**: Facial nerve (CN VII) * **Sensory nerve of face**: Trigeminal nerve (CN V) * **Main artery of face**: Facial artery --- If you want next: * **MCQs (hard + case based)** * **Clinical correlations only** * **Embryological basis** * **SEO-optimized version** * **Notes in table format** Just tell me 👍
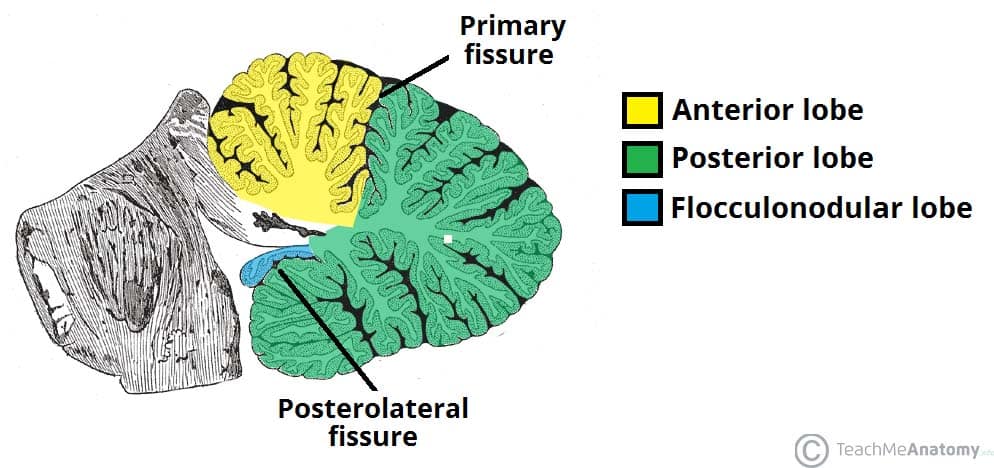
Cerebellum Anatomy Structure Functions and Clinical Importance
## Cerebellum Anatomy – Complete SEO-Friendly Guide ### Introduction The **cerebellum** is a major part of the hindbrain that plays a critical role in **coordination of movement, balance, posture, muscle tone, and motor learning**. Although it does not initiate movement, it fine-tunes motor activity to ensure accuracy and smooth execution. --- ## Location and Relations * Situated in the **posterior cranial fossa** * Lies **behind the pons and medulla** * Separated from the cerebrum by the **tentorium cerebelli** * Forms the **roof of the fourth ventricle** --- ## Gross Anatomy of the Cerebellum ### External Features The cerebellum consists of: 1. **Two hemispheres** (right and left) 2. **Vermis** (midline structure connecting hemispheres) #### Surfaces * **Superior surface** * **Inferior surface** * Both surfaces show numerous transverse folds called **folia** --- ## Lobes of the Cerebellum The cerebellum is divided by fissures into **three lobes**: ### 1. Anterior Lobe * Located anterior to the **primary fissure** * Functionally related to **spinocerebellum** * Involved in **posture and gait control** ### 2. Posterior Lobe * Largest lobe * Lies between primary fissure and posterolateral fissure * Involved in **fine voluntary movements** ### 3. Flocculonodular Lobe * Composed of **flocculus + nodulus** * Also called **vestibulocerebellum** * Responsible for **balance and eye movements** --- ## Functional Divisions of the Cerebellum ### 1. Cerebrocerebellum * Lateral hemispheres * Connected to cerebral cortex * Controls **planning and coordination of skilled movements** ### 2. Spinocerebellum * Vermis and intermediate zones * Regulates **muscle tone and ongoing movements** ### 3. Vestibulocerebellum * Flocculonodular lobe * Maintains **equilibrium and eye coordination** --- ## Cerebellar Cortex (Microscopic Anatomy) ### Layers of Cerebellar Cortex The cerebellar cortex has **three layers**: 1. **Molecular Layer** * Contains stellate and basket cells * Few neurons, mostly fibers 2. **Purkinje Cell Layer** * Single layer of large **Purkinje cells** * Output neurons of the cerebellar cortex * Inhibitory (GABAergic) 3. **Granular Layer** * Contains granule cells and Golgi cells * Highly cellular --- ## White Matter of Cerebellum * Located deep to the cortex * Appears as **arbor vitae** (tree-like pattern) * Carries fibers connecting cortex to cerebellar nuclei --- ## Deep Cerebellar Nuclei Embedded within white matter: 1. **Dentate** 2. **Emboliform** 3. **Globose** 4. **Fastigial** These nuclei serve as **major output centers** of the cerebellum. --- ## Cerebellar Peduncles The cerebellum connects to the brainstem via **three paired peduncles**: ### 1. Superior Cerebellar Peduncle * Connects to **midbrain** * Mainly **efferent (output)** fibers ### 2. Middle Cerebellar Peduncle * Connects to **pons** * Largest peduncle * Carries **afferent fibers from cerebral cortex** ### 3. Inferior Cerebellar Peduncle * Connects to **medulla** * Mixed afferent and efferent fibers --- ## Blood Supply of the Cerebellum * **Superior cerebellar artery (SCA)** * **Anterior inferior cerebellar artery (AICA)** * **Posterior inferior cerebellar artery (PICA)** All arise from the **vertebrobasilar system**. --- ## Functional Summary * Coordinates voluntary movements * Maintains posture and balance * Regulates muscle tone * Involved in motor learning and error correction --- ## Clinical Correlation (Brief) Lesions of the cerebellum lead to: * **Ataxia** * **Dysmetria** * **Intention tremor** * **Nystagmus** * **Hypotonia** * **Scanning speech** --- ## SEO Title **Cerebellum Anatomy Structure Functions and Clinical Importance** ## Meta Description Comprehensive SEO-friendly guide on cerebellum anatomy covering location lobes functional divisions cerebellar cortex peduncles blood supply and clinical significance. ## SEO Keywords cerebellum anatomy, cerebellar lobes, cerebellar cortex layers, cerebellar peduncles, deep cerebellar nuclei, cerebellum functions, hindbrain anatomy, neuroanatomy cerebellum --- If you want next: * **30 case-based cerebellar lesion scenarios** * **Hard MCQs with explanations** * **Clinical syndromes of cerebellar lesions** * **HTML/CSS/JS exam-mode MCQs** Just tell me 👍 Below are **high-yield clinical case scenarios of cerebellar lesions with clear diagnosis and management**, written in an **exam-oriented, clinical approach**. Concise but complete. --- ## 1. Midline (Vermis) Lesion – Truncal Ataxia **Case** A 45-year-old man with chronic alcohol use presents with inability to sit or stand without support. Limb movements are relatively normal. Gait is broad-based and staggering. **Clinical Diagnosis** Vermian cerebellar lesion (anterior lobe degeneration) **Key Features** * Truncal ataxia * Broad-based gait * Minimal limb ataxia **Management** * Treat underlying cause (alcohol cessation) * Thiamine supplementation * Physiotherapy for gait and balance * Fall-prevention measures --- ## 2. Cerebellar Hemisphere Lesion – Ipsilateral Limb Ataxia **Case** A 60-year-old man with hypertension presents with clumsiness of the right hand. Finger-nose test shows past pointing on the right. **Clinical Diagnosis** Right cerebellar hemisphere infarction **Key Features** * Ipsilateral limb ataxia * Dysmetria * Intention tremor **Management** * MRI brain to confirm stroke * Antiplatelet therapy * Blood pressure and risk factor control * Neurorehabilitation --- ## 3. Flocculonodular Lobe Lesion – Balance Disorder **Case** A child presents with frequent falls, vertigo, and abnormal eye movements. **Clinical Diagnosis** Vestibulocerebellar lesion **Key Features** * Nystagmus * Vertigo * Severe balance impairment **Management** * Treat underlying cause (tumor/infection) * Vestibular rehabilitation * Anti-vertigo medications (short term) --- ## 4. Acute Cerebellar Stroke **Case** A 70-year-old patient presents with sudden onset vertigo, vomiting, ataxia, and headache. **Clinical Diagnosis** Cerebellar infarction (PICA/AICA territory) **Management** * Emergency CT/MRI brain * Manage raised intracranial pressure * Antiplatelet or anticoagulation as indicated * Neurosurgical decompression if brainstem compression --- ## 5. Cerebellar Hemorrhage **Case** A hypertensive patient develops sudden headache, vomiting, and rapid deterioration of consciousness. **Clinical Diagnosis** Cerebellar hemorrhage **Management** * Immediate CT brain * Blood pressure control * Neurosurgical evacuation if large bleed * ICU monitoring --- ## 6. Alcoholic Cerebellar Degeneration **Case** A chronic alcoholic presents with progressive gait instability over months. **Clinical Diagnosis** Anterior cerebellar lobe degeneration **Management** * Alcohol abstinence * Nutritional rehabilitation * Thiamine and multivitamins * Long-term physiotherapy --- ## 7. Multiple Sclerosis with Cerebellar Involvement **Case** A young woman presents with intention tremor, scanning speech, and nystagmus. **Clinical Diagnosis** Cerebellar involvement in multiple sclerosis **Management** * MRI brain with contrast * Acute relapse: corticosteroids * Disease-modifying therapy * Speech and occupational therapy --- ## 8. Cerebellar Tumor (Medulloblastoma) **Case** A child presents with morning vomiting, headache, and gait ataxia. **Clinical Diagnosis** Midline cerebellar tumor (medulloblastoma) **Management** * MRI brain * Surgical excision * Radiotherapy and chemotherapy * Long-term neurodevelopmental follow-up --- ## 9. Cerebellar Abscess **Case** A patient with chronic otitis media presents with fever, headache, and ataxia. **Clinical Diagnosis** Cerebellar abscess **Management** * MRI with contrast * IV broad-spectrum antibiotics * Surgical drainage if indicated * Treat source of infection --- ## 10. Drug-Induced Cerebellar Toxicity **Case** A patient on phenytoin presents with nystagmus and ataxia. **Clinical Diagnosis** Drug-induced cerebellar dysfunction **Management** * Check drug levels * Stop or reduce offending drug * Supportive care * Monitor recovery --- ## 11. Paraneoplastic Cerebellar Degeneration **Case** A middle-aged woman presents with rapidly progressive ataxia; later found to have ovarian carcinoma. **Clinical Diagnosis** Paraneoplastic cerebellar degeneration **Management** * Treat underlying malignancy * Immunotherapy (steroids, IVIG) * Supportive rehabilitation --- ## 12. Cerebellar Ataxia in Hypothyroidism **Case** A patient presents with slow speech, unsteady gait, and fatigue. **Clinical Diagnosis** Metabolic cerebellar dysfunction **Management** * Thyroid function tests * Thyroxine replacement * Gradual neurological improvement --- ## 13. Arnold–Chiari Malformation **Case** A young adult presents with occipital headache worsened by coughing and gait imbalance. **Clinical Diagnosis** Chiari malformation affecting cerebellum **Management** * MRI brain and cervical spine * Neurosurgical decompression if symptomatic * Analgesia for headache --- ## 14. Post-Infectious Cerebellitis **Case** A child develops acute ataxia after viral illness. **Clinical Diagnosis** Acute cerebellitis **Management** * Usually self-limiting * Supportive care * Steroids if severe * Physiotherapy --- ## 15. Degenerative Spinocerebellar Ataxia **Case** Progressive ataxia with positive family history. **Clinical Diagnosis** Spinocerebellar degeneration **Management** * Genetic testing * Symptomatic treatment * Rehabilitation * Genetic counseling --- ### One-Line Exam Summary > **Cerebellar lesions produce ipsilateral signs and are managed by treating the cause, controlling complications, and long-term neurorehabilitation.** If you want next: * **30 hard case-based MCQs** * **HTML/CSS/JS interactive exam module** * **Cerebellar syndromes comparison table** * **SEO FAQ schema for cerebellar lesions** Just tell me.
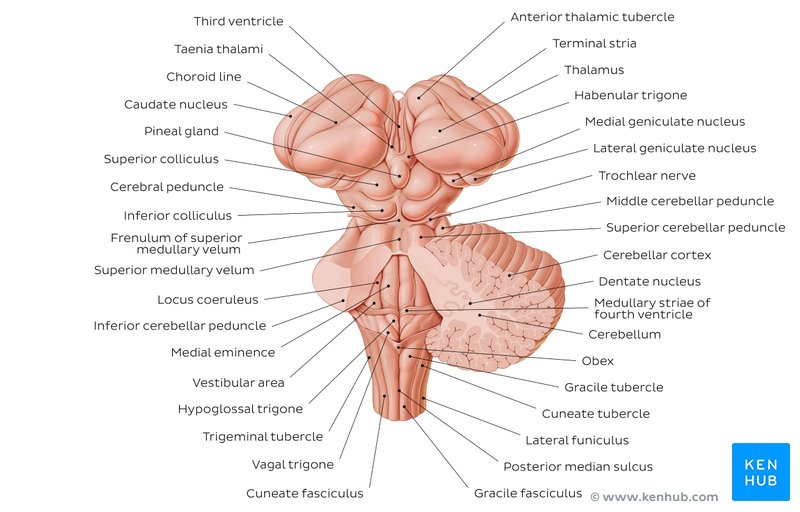
Brainstem Syndromes Explained With 30 High-Yield Case Scenarios and Management
## **Brainstem Syndromes Case Scenarios With Clinical Explanation and Management Guide** ### **SEO Title** **Brainstem Syndromes Explained With 30 High-Yield Case Scenarios and Management** ### **SEO Description** Comprehensive SEO-friendly guide on brainstem syndromes with 30 detailed clinical case scenarios, anatomical explanations, lesion localization, and stepwise management for medical exams and clinical practice. ### **SEO Keywords** brainstem syndromes, midbrain syndromes, pontine syndromes, medullary syndromes, weber syndrome, benedict syndrome, lateral medullary syndrome, brainstem lesion cases, neurology case scenarios, brainstem stroke management --- ## **MIDBRAIN SYNDROMES** --- ### **1. Weber Syndrome** **Case Scenario:** A 55-year-old man presents with sudden right-sided weakness and drooping of the left eyelid. Examination shows left eye ptosis, dilated pupil, and right hemiplegia. **Explanation:** Lesion in **ventromedial midbrain** affecting: * Oculomotor nerve (III) * Corticospinal tract Usually due to **posterior cerebral artery infarct** **Management:** * Acute ischemic stroke protocol * Antiplatelet therapy * Blood pressure and glucose control * Physiotherapy for hemiplegia --- ### **2. Benedikt Syndrome** **Case Scenario:** A patient has ipsilateral oculomotor palsy with contralateral tremor and ataxia. **Explanation:** Lesion in **tegmentum of midbrain** involving: * Oculomotor nerve * Red nucleus * Medial lemniscus **Management:** * Treat stroke or tumor cause * Antiplatelets or anticoagulation * Rehabilitation for ataxia --- ### **3. Claude Syndrome** **Case Scenario:** A patient presents with ipsilateral third nerve palsy and contralateral limb ataxia. **Explanation:** Combination of **Weber + Benedikt** * Oculomotor nerve * Red nucleus * Corticospinal tract **Management:** * Stroke management * Neurorehabilitation --- ### **4. Parinaud Syndrome** **Case Scenario:** Young adult with inability to look upward and light-near dissociation. **Explanation:** Lesion in **dorsal midbrain (pineal region)** Often due to pineal tumor or hydrocephalus. **Management:** * Treat raised intracranial pressure * Neurosurgical tumor management --- ### **5. Nothnagel Syndrome** **Case Scenario:** Patient has ipsilateral third nerve palsy and cerebellar ataxia. **Explanation:** Lesion of **superior cerebellar peduncle + oculomotor nerve** **Management:** * Tumor or demyelination treatment * Supportive therapy --- ## **PONTINE SYNDROMES** --- ### **6. Millard-Gubler Syndrome** **Case Scenario:** A patient shows facial paralysis on left side with right-sided hemiplegia. **Explanation:** Lesion in **ventral pons** * Facial nerve (VII) * Corticospinal tract **Management:** * Stroke care * Facial physiotherapy --- ### **7. Foville Syndrome** **Case Scenario:** Inability to abduct eye, facial weakness, and contralateral hemiplegia. **Explanation:** Lesion in **pontine tegmentum** * Abducens nucleus * Facial nerve * Corticospinal tract **Management:** * Antiplatelets * Eye care for diplopia --- ### **8. Raymond Syndrome** **Case Scenario:** Ipsilateral lateral rectus palsy with contralateral hemiplegia. **Explanation:** Lesion affects: * Abducens nerve * Corticospinal tract **Management:** * Stroke treatment * Physical rehabilitation --- ### **9. Lateral Pontine Syndrome (AICA)** **Case Scenario:** Patient presents with facial paralysis, loss of pain and temperature on contralateral body, and vertigo. **Explanation:** AICA infarct affects: * Facial nerve * Spinothalamic tract * Vestibular nuclei **Management:** * Antiplatelets * Symptomatic vertigo treatment --- ### **10. Locked-In Syndrome** **Case Scenario:** Patient is conscious but cannot move limbs or speak, only vertical eye movements preserved. **Explanation:** Bilateral lesion of **ventral pons** * Corticospinal * Corticobulbar tracts **Management:** * Supportive ICU care * Communication aids * Prevention of complications --- ## **MEDULLARY SYNDROMES** --- ### **11. Lateral Medullary Syndrome (Wallenberg)** **Case Scenario:** Patient has dysphagia, hoarseness, ipsilateral facial pain loss, and contralateral body pain loss. **Explanation:** PICA infarct affects: * Nucleus ambiguus * Spinothalamic tract * Inferior cerebellar peduncle **Management:** * Airway protection * Nasogastric feeding * Stroke management --- ### **12. Medial Medullary Syndrome (Dejerine)** **Case Scenario:** Contralateral hemiplegia with loss of proprioception and ipsilateral tongue deviation. **Explanation:** Anterior spinal artery infarct involving: * Hypoglossal nerve * Corticospinal tract * Medial lemniscus **Management:** * Antiplatelets * Speech therapy --- ### **13. Jackson Syndrome** **Case Scenario:** Patient presents with ipsilateral hypoglossal paralysis and contralateral hemiplegia. **Explanation:** Lesion affects: * Hypoglossal nerve * Corticospinal tract **Management:** * Treat underlying lesion * Rehabilitation --- ### **14. Avellis Syndrome** **Case Scenario:** Hoarseness with contralateral loss of pain and temperature. **Explanation:** Lesion affects: * Nucleus ambiguus * Spinothalamic tract **Management:** * Swallowing therapy * Stroke care --- ### **15. Babinski-Nageotte Syndrome** **Case Scenario:** Features of lateral medullary syndrome plus contralateral hemiplegia. **Explanation:** Extension of lateral medullary lesion into corticospinal tract. **Management:** * Stroke management * Physiotherapy --- ## **MIXED AND FUNCTIONAL BRAINSTEM SYNDROMES** --- ### **16. Central Pontine Myelinolysis** **Case Scenario:** Alcoholic patient develops acute quadriplegia after rapid sodium correction. **Explanation:** Demyelination of central pons due to osmotic injury. **Management:** * Slow correction of sodium * Supportive care --- ### **17. Brainstem Glioma** **Case Scenario:** Child presents with cranial nerve palsies and long tract signs. **Explanation:** Diffuse intrinsic pontine glioma compresses nuclei. **Management:** * Radiotherapy * Steroids --- ### **18. Multiple Sclerosis Brainstem Lesion** **Case Scenario:** Young female with internuclear ophthalmoplegia and sensory symptoms. **Explanation:** Demyelination of medial longitudinal fasciculus. **Management:** * High-dose steroids * Disease-modifying therapy --- ### **19. Syringobulbia** **Case Scenario:** Patient has dissociated sensory loss in face with dysphagia. **Explanation:** Extension of syrinx into brainstem. **Management:** * Neurosurgical decompression --- ### **20. Brainstem Encephalitis** **Case Scenario:** Fever, altered sensorium, and multiple cranial nerve palsies. **Explanation:** Inflammatory involvement of brainstem nuclei. **Management:** * Antivirals or antibiotics * ICU monitoring --- ## **ADDITIONAL HIGH-YIELD CASE SCENARIOS** --- ### **21. Inferior Alternating Hemiplegia** **22. Superior Alternating Hemiplegia** **23. Pontine Hemorrhage** **24. Vertebrobasilar Insufficiency** **25. Brainstem Abscess** **26. Cavernous Hemangioma of Brainstem** **27. Progressive Bulbar Palsy** **28. Motor Neuron Disease with Brainstem Involvement** **29. Trauma-Induced Brainstem Lesion** **30. Metabolic Brainstem Dysfunction** *(Each presents with characteristic cranial nerve palsies + long tract signs and is managed by treating the underlying cause with supportive neurocritical care.)* --- ## **Key Exam Tip** > **Brainstem syndromes always show “crossed findings” – ipsilateral cranial nerve palsy with contralateral motor or sensory deficit.** --- ## **FAQ (SEO-Friendly)** **Q1. Which artery causes lateral medullary syndrome?** Posterior inferior cerebellar artery (PICA). **Q2. Most common brainstem stroke?** Lateral medullary syndrome. **Q3. Why is locked-in syndrome unique?** Consciousness preserved with complete paralysis. **Q4. Which nerve is involved in medial medullary syndrome?** Hypoglossal nerve. --- If you want, I can also provide: * **30 hard case-based MCQs** * **HTML/CSS/JS exam mode test** * **Schema-ready FAQ + breadcrumb** * **Illustrated lesion localization tables** Just tell me what to generate next.
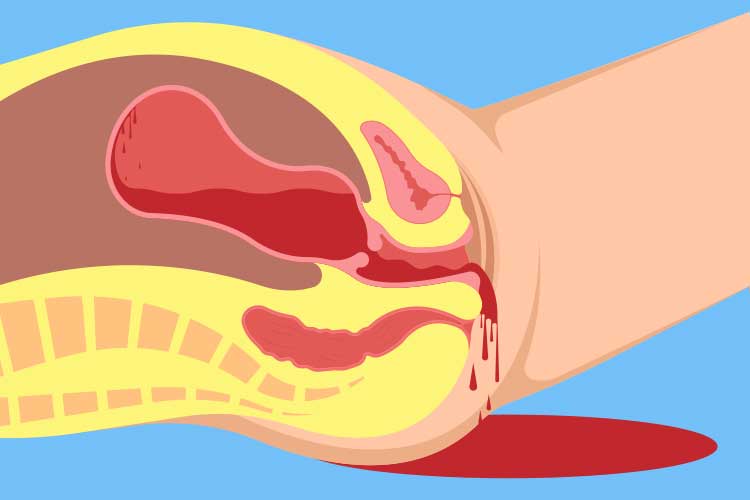
Postpartum Hemorrhage Causes Diagnosis and Management
## **Postpartum Hemorrhage Clinical Guide Causes Diagnosis and Management** ### **Definition** **Postpartum hemorrhage (PPH)** is excessive bleeding after childbirth. * **Primary (early) PPH:** ≥500 mL after vaginal delivery or ≥1000 mL after cesarean section within **24 hours** * **Secondary (late) PPH:** Excessive bleeding from **24 hours to 6 weeks** postpartum --- ## **Epidemiology and Importance** * Leading cause of **maternal mortality worldwide** * Rapid onset and progression require **early recognition and protocol-based management** --- ## **Pathophysiology** Normal hemostasis after delivery depends on **uterine contraction** compressing spiral arteries. Failure of contraction or disruption of clotting leads to uncontrolled bleeding. --- ## **Causes – “4 Ts” Framework** 1. **Tone (most common – uterine atony)** * Overdistended uterus (multiple pregnancy, polyhydramnios, macrosomia) * Prolonged or precipitous labor * Chorioamnionitis 2. **Trauma** * Cervical, vaginal, perineal tears * Uterine rupture * Hematomas 3. **Tissue** * Retained placental tissue * Placenta accreta spectrum 4. **Thrombin** * Coagulopathies (DIC, severe preeclampsia, HELLP, anticoagulant use) --- ## **Risk Factors** * Previous PPH * Operative delivery * Induction or augmentation of labor * Anemia * Placenta previa or accreta --- ## **Clinical Features** * Excessive vaginal bleeding * Boggy or enlarged uterus * Signs of hypovolemia: tachycardia, hypotension, pallor, altered sensorium * Reduced urine output --- ## **Initial Assessment and Diagnosis** **Diagnosis is clinical and urgent** * Quantify blood loss (visual + weighing) * Assess uterine tone * Inspect birth canal * Evaluate placenta completeness ### **Investigations (do not delay treatment)** * CBC (Hb, platelets) * Blood group and cross-match * Coagulation profile (PT, aPTT, fibrinogen) * ABG if severe shock --- ## **Management – Stepwise Approach** ### **Immediate Resuscitation** * Call for help * Airway and oxygen * Two wide-bore IV lines * Crystalloids followed by blood products (1:1:1 PRBC:plasma:platelets if massive) --- ## **Uterotonic Drugs (Cornerstone of Treatment)** ### **1. Oxytocin** * **Indication:** First-line for uterine atony * **Mechanism:** Stimulates uterine smooth muscle contraction * **Dose:** * IV infusion: 10–40 IU in 1 L NS/RL * IM: 10 IU * **Adverse effects:** Hypotension (rapid IV), water intoxication * **Contraindications:** None significant in PPH * **Monitoring:** Uterine tone, vitals * **Counselling:** First-line and safe --- ### **2. Methylergometrine** * **Mechanism:** Sustained uterine contraction via alpha-adrenergic stimulation * **Dose:** 0.2 mg IM (may repeat) * **Adverse effects:** Hypertension, nausea * **Contraindications:** Hypertension, preeclampsia, cardiac disease * **Monitoring:** Blood pressure --- ### **3. Carboprost (15-methyl PGF2α)** * **Mechanism:** Prostaglandin-induced myometrial contraction * **Dose:** 250 µg IM every 15–90 min (max 8 doses) * **Adverse effects:** Bronchospasm, diarrhea, fever * **Contraindications:** Asthma * **Monitoring:** Respiratory status --- ### **4. Misoprostol** * **Mechanism:** Prostaglandin E1 analog * **Dose:** 800–1000 µg rectal or sublingual * **Adverse effects:** Fever, shivering * **Use:** Low-resource settings --- ### **5. Tranexamic Acid** * **Indication:** All PPH within 3 hours of onset * **Mechanism:** Inhibits fibrinolysis * **Dose:** 1 g IV over 10 min (repeat once if bleeding continues) * **Adverse effects:** Rare thrombosis * **Contraindications:** Active thromboembolic disease * **Monitoring:** Renal function if repeated * **Counselling:** Reduces mortality when given early --- ## **Mechanical and Surgical Measures** ### **Mechanical** * Bimanual uterine massage * Uterine balloon tamponade (Bakri balloon) * Uterine packing ### **Surgical** * Uterine compression sutures (B-Lynch) * Uterine artery ligation * Internal iliac artery ligation * **Hysterectomy** (life-saving last resort) --- ## **Management by Cause** * **Atony:** Uterotonics → balloon → surgery * **Trauma:** Immediate repair of tears * **Tissue:** Manual removal, curettage * **Thrombin:** Correct coagulopathy with blood products --- ## **Secondary Postpartum Hemorrhage** **Causes** * Retained products * Subinvolution of uterus * Endometritis **Management** * Antibiotics * Uterotonics * Ultrasound-guided evacuation if indicated --- ## **Complications** * Hypovolemic shock * Acute kidney injury * DIC * Sheehan syndrome * Maternal death --- ## **Prevention** * Active management of third stage of labor * Antenatal anemia correction * Risk stratification and preparedness --- ## **Prognosis** Excellent with early recognition and protocol-driven care; delays increase morbidity and mortality. --- ## **SEO Meta Data** **SEO Title:** Postpartum Hemorrhage Causes Diagnosis and Management **Meta Description:** Comprehensive clinical guide on postpartum hemorrhage covering causes, diagnosis, stepwise management, uterotonic drugs, surgical options, prevention, and complications. **SEO Keywords (comma separated):** postpartum hemorrhage, PPH management, uterine atony, causes of PPH, tranexamic acid PPH, obstetric emergency, maternal hemorrhage, third stage labor complications --- ## **Frequently Asked Questions** **What is the most common cause of postpartum hemorrhage?** Uterine atony. **When should tranexamic acid be given in PPH?** Within 3 hours of onset of bleeding. **What is the first-line drug for PPH?** Oxytocin. **When is hysterectomy indicated in PPH?** When bleeding is uncontrollable and life-threatening despite conservative measures. **Can PPH occur after 24 hours?** Yes, it is termed secondary postpartum hemorrhage. --- If you want, I can **convert this into a CMS-ready HTML or PHP page**, **add FAQ schema and Article schema**, or **create MCQs and case-based questions** for your medical knowledge platform.
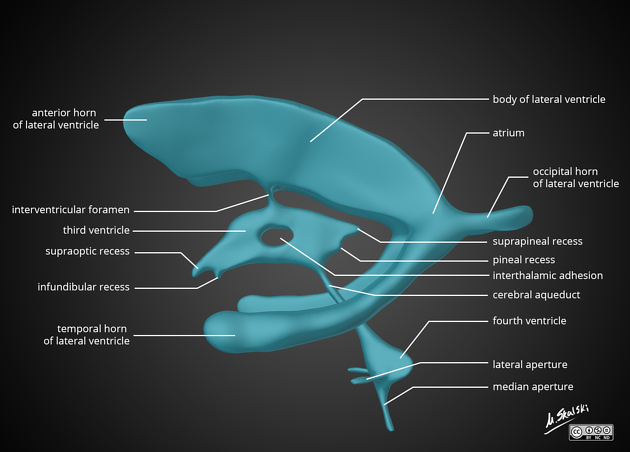
Cerebrospinal Fluid and Ventricular System Anatomy
## Cerebrospinal Fluid and Ventricular System Anatomy – Complete SEO-Friendly Guide ### SEO Title **Cerebrospinal Fluid and Ventricular System Anatomy** ### Meta Description Detailed anatomy of cerebrospinal fluid and the ventricular system covering formation, circulation, absorption, functions, ventricular components, and important clinical correlations. ### Keywords cerebrospinal fluid anatomy, ventricular system brain, lateral ventricles anatomy, third ventricle anatomy, fourth ventricle anatomy, CSF circulation, choroid plexus, arachnoid villi, hydrocephalus anatomy --- ## 1. Cerebrospinal Fluid (CSF) ### Definition Cerebrospinal fluid is a **clear, colorless fluid** that circulates within the **ventricular system of the brain and subarachnoid space** surrounding the brain and spinal cord, providing protection, nutrition, and waste removal. ### Normal Volume and Pressure * Total volume (adult): **≈150 mL** * Daily production: **≈500 mL** * Normal opening pressure (lumbar puncture): **70–180 mm H₂O** --- ## 2. Formation of CSF ### Choroid Plexus CSF is primarily produced by the **choroid plexus**, a vascular structure lined by **ependymal cells**. **Locations of choroid plexus** * Lateral ventricles (body and temporal horn) * Third ventricle * Fourth ventricle **Mechanism** * Active secretion via **Na⁺/K⁺ ATPase** * Water follows osmotically * Independent of intracranial pressure --- ## 3. Ventricular System of the Brain The ventricular system consists of **four interconnected cavities** lined by ependyma and filled with CSF. --- ### 3.1 Lateral Ventricles (First and Second Ventricles) **Location** * One in each cerebral hemisphere **Parts** 1. **Anterior (frontal) horn** * In frontal lobe * Roof: Corpus callosum * Floor: Head of caudate nucleus 2. **Body** * Extends through parietal lobe 3. **Posterior (occipital) horn** * In occipital lobe 4. **Inferior (temporal) horn** * In temporal lobe * Floor: Hippocampus * Roof: Tail of caudate nucleus **Communication** * Each lateral ventricle communicates with the third ventricle via the **interventricular foramen (foramen of Monro)** --- ### 3.2 Third Ventricle **Location** * Midline cavity between the two thalami **Boundaries** * Lateral walls: Thalamus and hypothalamus * Floor: Hypothalamus * Roof: Tela choroidea * Anterior wall: Lamina terminalis * Posterior wall: Pineal region **Connections** * Receives CSF from lateral ventricles * Drains into the fourth ventricle via the **cerebral aqueduct (aqueduct of Sylvius)** --- ### 3.3 Fourth Ventricle **Location** * Between pons and medulla anteriorly * Cerebellum posteriorly **Boundaries** * Floor: Rhomboid fossa * Roof: Superior and inferior medullary vela **Openings** * **One median aperture (foramen of Magendie)** * **Two lateral apertures (foramina of Luschka)** These openings allow CSF to enter the **subarachnoid space**. --- ## 4. Circulation of CSF **Flow pathway** 1. Lateral ventricles 2. Foramen of Monro 3. Third ventricle 4. Cerebral aqueduct 5. Fourth ventricle 6. Foramen of Magendie and Luschka 7. Subarachnoid space 8. Arachnoid villi and granulations 9. Superior sagittal sinus --- ## 5. Absorption of CSF ### Arachnoid Villi and Granulations * Protrusions of arachnoid mater into venous sinuses * Act as **one-way valves** * Absorption occurs when CSF pressure exceeds venous pressure Minor absorption also occurs via: * Spinal nerve sheaths * Choroid plexus --- ## 6. Composition of CSF * Clear and acellular * Low protein * Low potassium and calcium * Higher chloride compared to plasma * Glucose ≈ 60% of plasma glucose --- ## 7. Functions of CSF * **Mechanical protection** (shock absorber) * **Buoyancy** (reduces effective brain weight) * **Nutrient delivery** * **Removal of metabolic waste** * **Maintenance of intracranial pressure** --- ## 8. Blood–CSF Barrier Formed by: * Tight junctions between **choroid plexus epithelial cells** Functions: * Regulates composition of CSF * Protects CNS from toxins --- ## 9. Clinical Correlations ### Hydrocephalus * Abnormal accumulation of CSF **Types** * **Non-communicating (obstructive):** Block within ventricular system (e.g., aqueductal stenosis) * **Communicating:** Impaired absorption at arachnoid villi * **Normal pressure hydrocephalus:** Triad of gait disturbance, dementia, urinary incontinence --- ### Raised Intracranial Pressure * Headache * Vomiting * Papilledema * Altered consciousness --- ### Lumbar Puncture * Performed at **L3–L4 or L4–L5** * Measures CSF pressure and composition --- ## 10. High-Yield Exam Points * CSF production: **Choroid plexus** * Narrowest part of ventricular system: **Cerebral aqueduct** * Largest ventricles: **Lateral ventricles** * Main absorption site: **Arachnoid granulations** * CSF volume remains constant despite high daily production --- If you want, I can also provide **MCQs (exam-oriented)**, **clinical case-based questions**, or **schema-style revision tables** for CSF and ventricles.
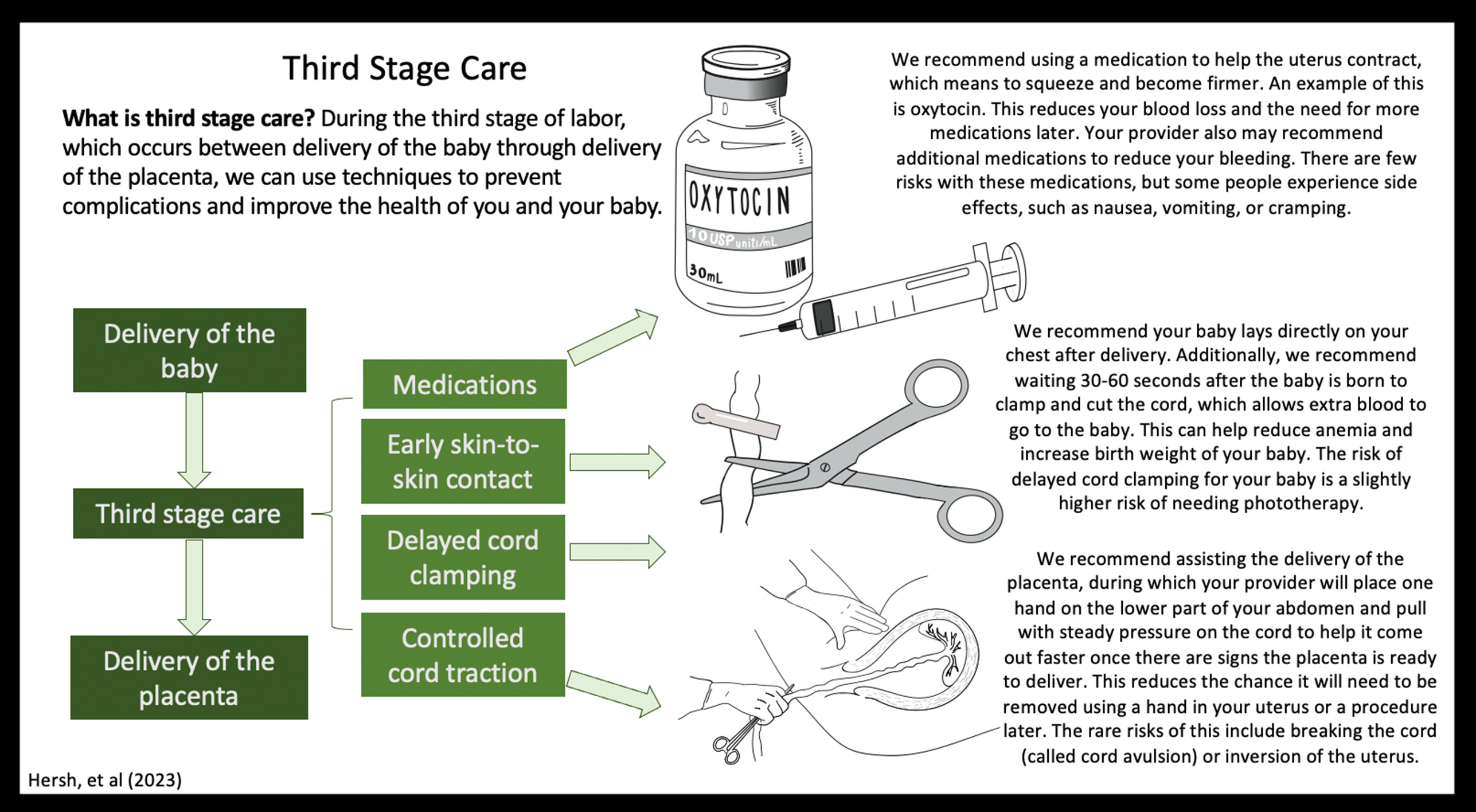
Active Management of Third Stage of Labor Complete Guide for PPH Prevention
Below is a **concise yet complete, exam-oriented, SEO-friendly reference** on **Active Management of Third Stage of Labor (AMTSL)**, structured for **medical students, clinicians, and obstetric exams**. --- # **Active Management of Third Stage of Labor (AMTSL)** ## **Definition** **Active Management of the Third Stage of Labor (AMTSL)** is a **planned set of interventions** performed **immediately after the birth of the baby** to **facilitate placental delivery and prevent postpartum hemorrhage (PPH)**, the leading cause of maternal mortality worldwide. --- ## **Importance and Rationale** * **Postpartum hemorrhage** accounts for a significant proportion of **maternal deaths** * AMTSL **reduces blood loss**, **shortens third stage**, and **lowers risk of uterine atony** * Recommended by **WHO, FIGO, ICM, and ACOG** --- ## **Components of AMTSL (Core Steps)** ### **1. Administration of a Uterotonic Drug (Most Important Step)** * Given **within 1 minute after delivery of the baby** * **After delivery of anterior shoulder or complete birth** * **Before or after placental delivery** (as per guideline) ### **2. Controlled Cord Traction (CCT)** * Gentle traction on umbilical cord * Combined with **counter-traction on uterus** * Performed **only after signs of placental separation** ### **3. Uterine Massage After Placental Delivery** * Ensures **uterine contraction** * Reduces risk of uterine atony * Routine sustained massage **not recommended**, but **assessment of tone is essential** --- ## **Uterotonic Drugs Used in AMTSL** ### **Oxytocin (Drug of Choice)** * **Dose:** 10 IU IM or slow IV * **Onset:** 2–3 minutes * **Advantages:** Highly effective, minimal side effects * **Preferred by WHO** ### **Ergometrine / Methylergometrine** * **Dose:** 0.2 mg IM/IV * **Contraindications:** Hypertension, pre-eclampsia, heart disease * Causes sustained uterine contraction ### **Oxytocin + Ergometrine (Syntometrine)** * More effective but **higher side effects** * Nausea, vomiting, hypertension ### **Misoprostol** * **Dose:** 600 μg orally * Used where injectables unavailable * Side effects: Fever, shivering --- ## **Controlled Cord Traction (CCT): Key Points** * Perform only when uterus is **well contracted** * Look for **signs of placental separation**: * Lengthening of cord * Gush of blood * Uterus becomes globular and rises * Prevents **retained placenta** * Reduces duration of third stage --- ## **Uterine Massage** * After placenta delivery * Assess uterine tone **every 15 minutes for first 2 hours** * Continuous massage is **not routinely advised** --- ## **Timing of Cord Clamping** * **Delayed cord clamping (1–3 minutes)** recommended * Does **not interfere with AMTSL** * Improves neonatal iron stores --- ## **Benefits of AMTSL** * ↓ Postpartum hemorrhage by **50–70%** * ↓ Severe blood loss (>1000 mL) * ↓ Need for blood transfusion * ↓ Duration of third stage * ↓ Maternal morbidity and mortality --- ## **AMTSL vs Expectant Management** | Feature | AMTSL | Expectant Management | | ------------- | ------------------ | -------------------- | | Uterotonic | Given routinely | Not given | | Cord traction | Yes | No | | Blood loss | Significantly less | More | | Duration | Shorter | Longer | | PPH risk | Low | High | --- ## **Indications** * **All vaginal deliveries** * Especially important in: * Anemia * Multiple pregnancy * Prolonged labor * Polyhydramnios * Grand multiparity --- ## **Contraindications** * No absolute contraindication * Avoid **ergometrine** in: * Hypertension * Preeclampsia * Cardiac disease --- ## **Complications (Rare)** * Retained placenta (if CCT done improperly) * Uterine inversion (improper traction) * Drug side effects (ergometrine, misoprostol) --- ## **WHO Recommended AMTSL Protocol (Summary)** 1. **Oxytocin 10 IU IM/IV** 2. **Delayed cord clamping** 3. **Controlled cord traction** 4. **Assess uterine tone** --- ## **Key Exam Pearls** * **Most important component:** Uterotonic administration * **Drug of choice:** Oxytocin * **Primary aim:** Prevention of postpartum hemorrhage * **Third stage normal duration:** ≤ 30 minutes --- ## **Conclusion** **Active Management of Third Stage of Labor** is a **simple, cost-effective, life-saving obstetric intervention**. Universal implementation of AMTSL significantly reduces **postpartum hemorrhage and maternal mortality**, making it a **standard of care in modern obstetrics**. --- ### If you want next: * **SEO title and meta keywords** * **High-yield MCQs (exam mode) in single HTML-CSS-JS file** * **Clinical flowchart image** * **Comparison table for exams** Just tell me 👍
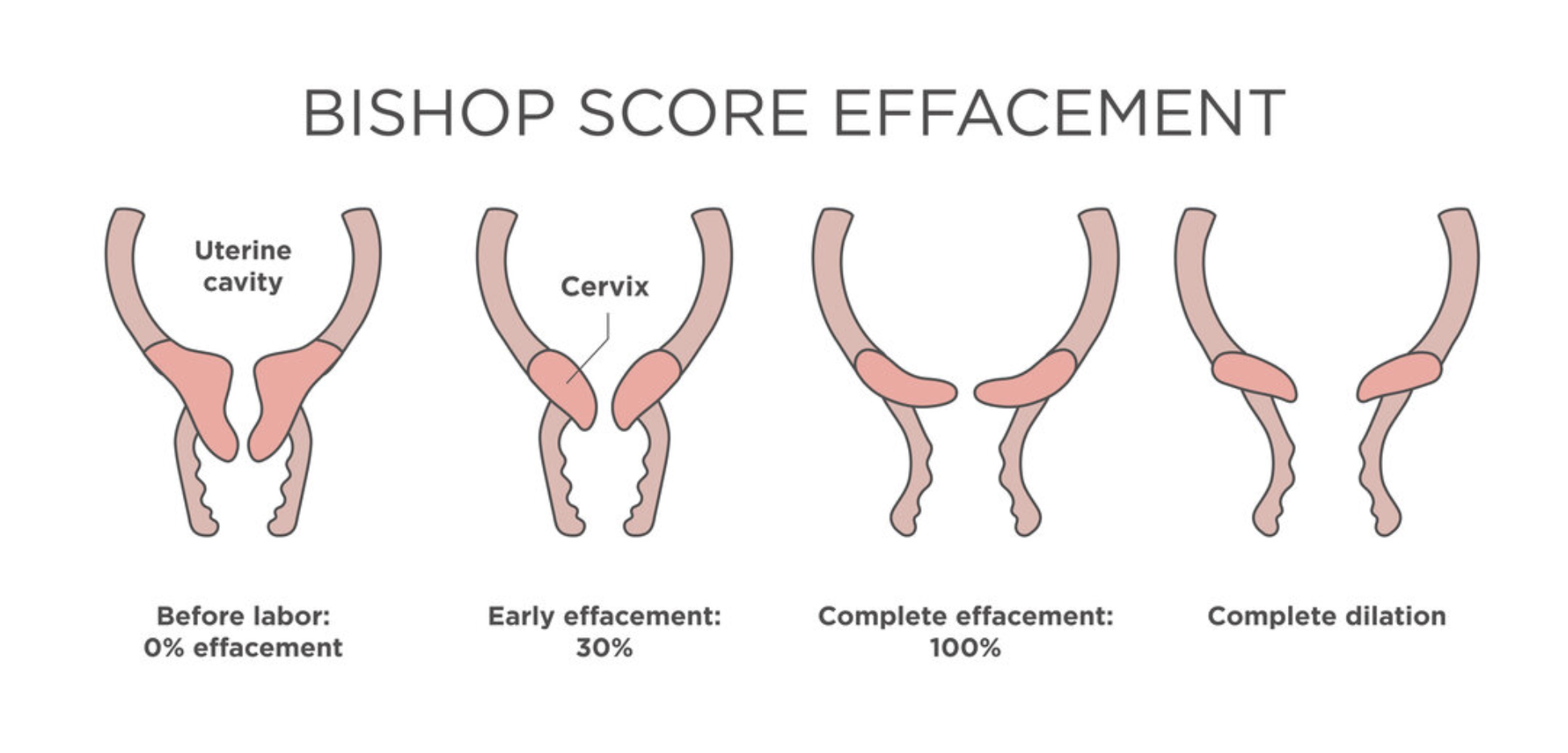
Induction of Labor Indications Methods Contraindications Complications
Below is a **concise yet complete, SEO-friendly, exam-ready reference** on **Induction of Labor**, structured with clear headings (H1–H3 style) and high-yield clinical content. --- # **Induction of Labor** ## **Definition** **Induction of labor (IOL)** is the **artificial initiation of uterine contractions** before the spontaneous onset of labor, with the aim of achieving **vaginal delivery**, when continuation of pregnancy poses **greater maternal or fetal risk** than delivery. --- ## **Indications for Induction of Labor** ### **Maternal Indications** * Post-term pregnancy (≥41 weeks) * Pre-eclampsia and eclampsia * Gestational hypertension * Diabetes mellitus (gestational or pre-existing) * Premature rupture of membranes (PROM) at term * Chorioamnionitis * Rh isoimmunization * Maternal medical disorders (renal, cardiac disease) * Intrauterine fetal demise (IUFD) ### **Fetal Indications** * Intrauterine growth restriction (IUGR) * Oligohydramnios * Non-reassuring fetal status (controlled setting) * Fetal anomalies requiring early delivery ### **Elective Induction** * At ≥39 weeks with confirmed gestational age and favorable cervix --- ## **Contraindications to Induction of Labor** ### **Absolute Contraindications** * Placenta previa * Vasa previa * Transverse lie * Cord prolapse * Previous classical cesarean section * Previous uterine rupture * Invasive cervical cancer * Cephalopelvic disproportion (CPD) ### **Relative Contraindications** * Multiple previous cesarean sections * Grand multiparity * Unstable lie * Active genital herpes --- ## **Pre-Induction Assessment** Show readiness of cervix and maternal-fetal safety. ### **Bishop Score** Assesses **cervical favorability** using: * Cervical dilatation * Effacement * Consistency * Position * Fetal station **Score interpretation:** * **≥6–8** → Favorable cervix (high success) * **<6** → Unfavorable cervix (requires cervical ripening) --- ## **Methods of Induction of Labor** ### **1. Mechanical Methods** * **Membrane sweeping** * **Foley catheter (balloon catheter)** * Double balloon catheter **Advantages:** Low cost, minimal uterine hyperstimulation **Disadvantages:** Discomfort, infection risk --- ### **2. Pharmacological Methods** #### **Prostaglandins** * **Dinoprostone (PGE₂)** – Gel, tablet, vaginal insert * **Misoprostol (PGE₁)** – Oral or vaginal **Actions:** * Cervical ripening * Uterine contractions **Contraindications:** * Previous uterine scar (relative for misoprostol) * Fetal distress * Hypersensitivity --- #### **Oxytocin** * Used after cervical ripening * IV infusion with titration **Mechanism:** Stimulates uterine smooth muscle contraction **Monitoring:** Continuous CTG required --- ### **3. Surgical Methods** * **Amniotomy (Artificial rupture of membranes)** **Prerequisites:** * Engaged head * Favorable cervix * No placenta previa --- ## **Monitoring During Induction** * Continuous fetal heart rate monitoring * Maternal vitals * Uterine contraction pattern * Progress of labor (partograph) --- ## **Complications of Induction of Labor** ### **Maternal Complications** * Uterine hyperstimulation * Uterine rupture * Postpartum hemorrhage * Infection * Failed induction leading to cesarean section ### **Fetal Complications** * Fetal distress * Meconium aspiration * Birth asphyxia * Cord prolapse (after amniotomy) --- ## **Failed Induction** **Definition:** Failure to establish active labor after adequate attempts with appropriate methods. **Management:** * Re-assess indication * Repeat cervical ripening * Cesarean delivery if indicated --- ## **Key Clinical Pearls** * Always confirm **gestational age** before induction * Bishop score guides method selection * Avoid prostaglandins in scarred uterus (especially misoprostol) * Continuous monitoring is mandatory * Individualize induction based on maternal and fetal condition --- ## **Conclusion** Induction of labor is a **critical obstetric intervention** that improves maternal and fetal outcomes when appropriately indicated. Proper **case selection, cervical assessment, method choice, and vigilant monitoring** are essential to maximize success and minimize complications. --- If you want, I can next provide: * **SEO title, meta description, and keywords** * **Exam-oriented tables** * **Case-based MCQs (HTML + CSS + JS, single file, modern UI)** * **Flowcharts for induction decision-making**
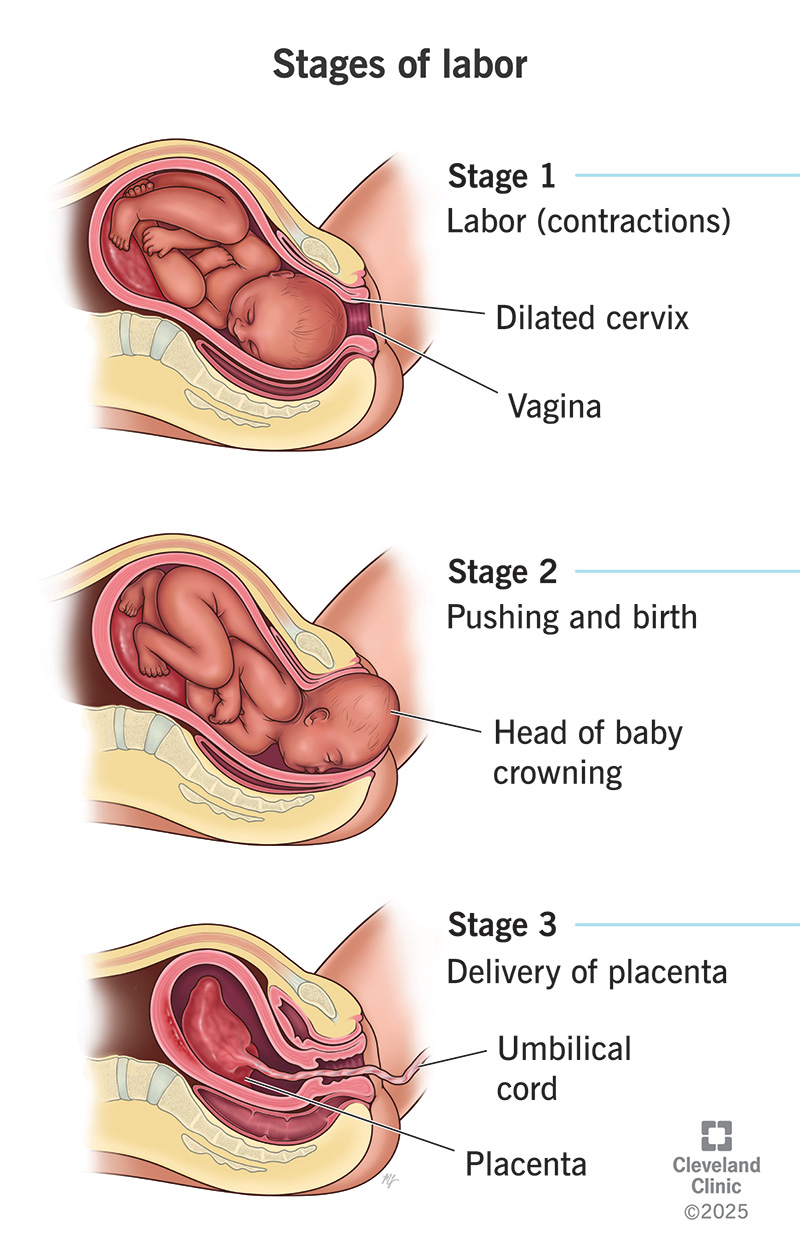
Normal Labour Definition Stages Physiology Management and Clinical Features
Below is a **concise yet complete, SEO-friendly medical reference** on **Normal Labour**, structured with clear **H1–H3 headings** and exam-oriented clarity. --- # **Normal Labour** ## **Definition of Normal Labour** Normal labour is a **physiological process** in which a **term pregnancy (37–42 weeks)** culminates in the **spontaneous onset of labour**, resulting in **vaginal delivery of a single, live fetus in vertex presentation**, followed by expulsion of the placenta, **without maternal or fetal complications**. --- ## **Criteria of Normal Labour** Normal labour fulfills all of the following: * **Gestational age:** 37–42 weeks * **Onset:** Spontaneous * **Presentation:** Vertex (cephalic) * **Number of fetus:** Singleton * **Progress:** Regular uterine contractions with progressive cervical dilatation * **Mode of delivery:** Vaginal, without operative intervention * **Outcome:** Healthy mother and baby --- ## **Physiology of Normal Labour** Labour is initiated by a complex interaction of: * **Hormonal factors:** ↑ Estrogen, ↓ Progesterone dominance, ↑ Prostaglandins, ↑ Oxytocin receptors * **Uterine activity:** Coordinated, rhythmic contractions starting from fundus * **Cervical changes:** Effacement and dilatation due to collagen remodeling * **Fetal contribution:** Fetal HPA axis activation and cortisol release --- ## **Stages of Normal Labour** ### **First Stage of Labour** **From onset of true labour pains to full cervical dilatation (10 cm)** #### Latent Phase * Cervical dilatation: 0–3/4 cm * Contractions: Mild, irregular * Duration: * Primigravida: up to 8–12 hours * Multigravida: shorter #### Active Phase * Cervical dilatation: 4–10 cm * Contractions: Regular, strong, 3–5 per 10 minutes * Rate of dilatation: * Primigravida: ~1 cm/hour * Multigravida: ~1.5 cm/hour --- ### **Second Stage of Labour** **From full dilatation to delivery of the fetus** * Duration: * Primigravida: ≤2 hours (≤3 hours with epidural) * Multigravida: ≤1 hour * Mechanism of labour occurs: * Engagement * Descent * Flexion * Internal rotation * Extension * Restitution and external rotation * Expulsion --- ### **Third Stage of Labour** **From delivery of fetus to expulsion of placenta** * Duration: ≤30 minutes * Placental separation mechanisms: * Schultze (central separation) * Duncan (marginal separation) * Managed actively to prevent postpartum hemorrhage --- ## **Mechanism of Normal Labour (Vertex Presentation)** 1. Engagement 2. Descent 3. Flexion 4. Internal rotation 5. Extension 6. Restitution 7. External rotation 8. Expulsion --- ## **Signs of True Labour** * Regular, painful uterine contractions * Progressive cervical effacement and dilatation * Show (blood-stained mucus) * Descent of presenting part --- ## **Monitoring in Normal Labour** * **Maternal:** Pulse, BP, temperature, uterine contractions * **Fetal:** Fetal heart rate monitoring * **Progress:** Partograph assessment of cervical dilatation, descent, and contractions --- ## **Management Principles of Normal Labour** * Supportive care and reassurance * Adequate hydration and nutrition * Pain relief (non-pharmacologic or pharmacologic) * Asepsis and bladder care * Continuous monitoring for deviations from normal --- ## **Outcome of Normal Labour** * Vaginal birth without complications * Minimal maternal morbidity * Healthy neonate with good Apgar score --- ## **Clinical Importance** * Benchmark for identifying **abnormal labour patterns** * Essential for **obstetric exams**, labour ward practice, and safe maternal care * Basis for using **partograph** and deciding interventions --- If you want, I can next provide: * **SEO title, meta description, and keywords** * **Abnormal labour comparison** * **Partograph-based exam notes** * **MCQs or case-based questions in HTML/CSS/JS (single file, modern UI)**
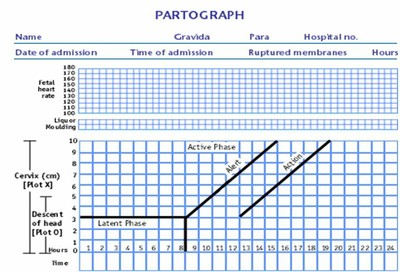
Partogram in Obstetrics Complete Guide for Monitoring Labour Progress
Below is a **single-place, exam-ready, clinically complete, SEO-friendly reference** on **Partogram**, written in a **clear H1–H4 structure** suitable for medical students, nurses, midwives, and clinicians. --- # **Partogram in Obstetrics: Complete Guide for Monitoring Labour Progress** ## **Introduction to Partogram** A **partogram (partograph)** is a **graphical tool** used to **monitor the progress of labour**, assess **maternal and fetal well-being**, and guide **timely clinical interventions**. It is a **WHO-recommended, low-cost, high-impact tool** for preventing **prolonged and obstructed labour**, thereby reducing **maternal and perinatal morbidity and mortality**. --- ## **Definition of Partogram** A **partogram** is a **chart that plots cervical dilatation against time**, along with **uterine contractions, fetal condition, and maternal parameters**, to provide a **continuous visual record of labour**. --- ## **Objectives of Using a Partogram** * Detect **abnormal labour progress early** * Identify **prolonged labour** * Prevent **obstructed labour** * Reduce **maternal complications** (PPH, sepsis, uterine rupture) * Reduce **fetal complications** (birth asphyxia, stillbirth) * Assist in **decision-making and referral** --- ## **Types of Partogram** ### **1. WHO Modified Partogram** * **Active phase starts at 4 cm cervical dilatation** * **Latent phase excluded** * Most commonly used in clinical practice ### **2. WHO Composite Partogram (Older)** * Includes **latent and active phase** * Latent phase up to **8 hours** * Less commonly used now ### **3. Simplified Partogram** * Focuses on **key parameters only** * Used in **low-resource settings** --- ## **Components of a Partogram** ### **A. Fetal Condition** Monitored to assess fetal well-being. #### **1. Fetal Heart Rate (FHR)** * Recorded **every 30 minutes** * Normal: **110–160 beats/min** * Abnormal: * <110 → Bradycardia * > 160 → Tachycardia #### **2. Amniotic Fluid** * **I** – Intact membranes * **C** – Clear liquor * **M** – Meconium-stained * **B** – Blood-stained #### **3. Moulding of Fetal Skull** * 0 → Sutures separated * * → Sutures touching * ++ → Sutures overlapping (reducible) * +++ → Sutures overlapping (irreducible) → **danger sign** --- ### **B. Progress of Labour** #### **1. Cervical Dilatation** * Plotted with **X** * Expected rate in active phase: **≥1 cm/hour** * Starts at **4 cm** #### **2. Descent of Head** * Plotted with **O** * Measured in **fifths palpable abdominally** * Or by **station (–5 to +5)** --- ### **C. Uterine Contractions** Recorded **every 30 minutes**: | Number / 10 min | Interpretation | | --------------- | ---------------- | | <2 | Inadequate | | 3–4 | Adequate | | ≥5 | Hyperstimulation | **Duration**: * <20 sec – Mild * 20–40 sec – Moderate * > 40 sec – Strong --- ### **D. Alert Line and Action Line** #### **Alert Line** * Drawn from **4 cm to full dilatation at 1 cm/hour** * Labour to the **left** → Normal * Crossing → **Slow progress** #### **Action Line** * Drawn **4 hours to the right of alert line** * Crossing → **Immediate intervention required** --- ### **E. Maternal Condition** #### **1. Pulse** * Every **30 minutes** #### **2. Blood Pressure** * Every **4 hours** * More frequent if abnormal #### **3. Temperature** * Every **2 hours** #### **4. Urine Examination** * Volume * Protein * Ketones --- ## **Interpretation of Partogram** ### **Normal Labour** * Cervical dilatation remains **left of alert line** * Adequate contractions * Normal fetal heart rate ### **Prolonged Labour** * Cervical dilatation crosses **alert line** * Requires: * Re-assessment * Amniotomy * Oxytocin augmentation * Referral if needed ### **Obstructed Labour** * Cervical dilatation reaches **action line** * Features: * No descent of head * Severe moulding (+++) * Maternal exhaustion * Management: * Operative delivery (CS / instrumental) --- ## **Indications for Using a Partogram** * All women in **active labour** * Especially useful in: * Primigravida * Induced labour * Previous prolonged labour * Referral cases --- ## **Contraindications / Limitations** * Not used in **latent phase (<4 cm)** * Less effective without **trained staff** * Requires **regular monitoring** --- ## **Advantages of Partogram** * Simple and cost-effective * Visual and easy to interpret * Reduces: * Prolonged labour * Obstructed labour * Unnecessary interventions * Improves maternal and neonatal outcomes --- ## **Disadvantages** * Incorrect plotting may mislead decisions * Requires training and adherence * Limited use without timely action --- ## **Role of Partogram in Modern Obstetrics** * Key tool in **Safe Motherhood Initiative** * Recommended by **WHO, FIGO** * Essential in **institutional deliveries** * Supports **evidence-based labour management** --- ## **Exam-Oriented Clinical Pearls** * **Alert line crossing** → Observe and evaluate * **Action line crossing** → Act immediately * **Moulding +++** → Suggests CPD * **Meconium liquor** → Fetal distress * **Rate <1 cm/hr** → Prolonged labour --- ## **Conclusion** The **partogram is a cornerstone of intrapartum care**, enabling **early detection of abnormal labour**, guiding **timely interventions**, and significantly improving **maternal and neonatal outcomes**. Proper understanding and correct use of the partogram are essential skills for all healthcare providers involved in childbirth. --- If you want next: * **SEO title, meta description, and keywords** * **Image-based explanation** * **25 hard case-based MCQs** * **HTML CSS JS interactive partogram simulator** Just tell me 👍
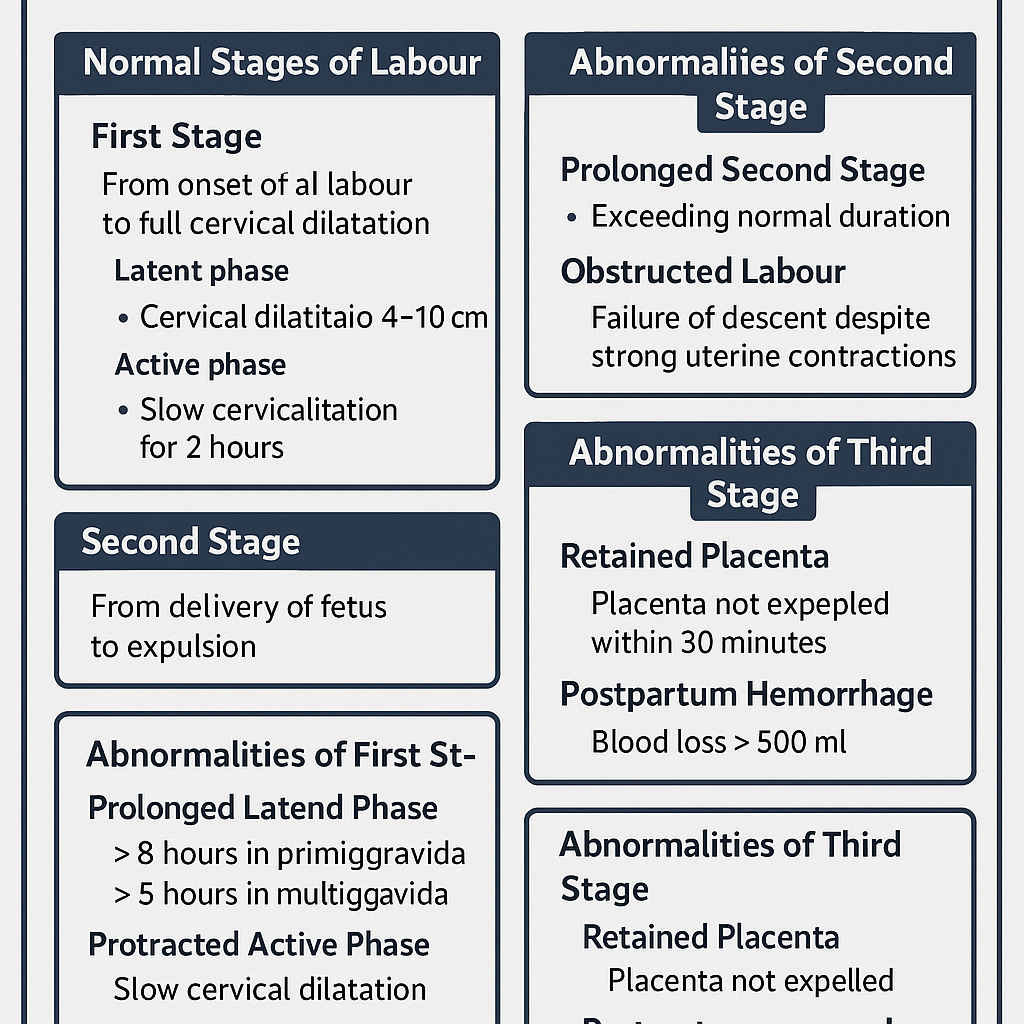
Stages of Labour Normal and Abnormal Progress Complete Clinical Guide
## **Stages of Labour Normal and Abnormal Progress Complete Clinical Guide** ### **SEO Description** Comprehensive obstetrics guide explaining normal and abnormal stages of labour with mechanisms, duration, clinical features, diagnosis, complications, and management for exams and clinical practice. ### **SEO Keywords** stages of labour, normal labour stages, abnormal labour, prolonged labour, obstructed labour, dysfunctional labour, first stage labour, second stage labour, third stage labour, active labour management, obstetrics labour guide --- # **Stages of Labour Normal and Abnormal** Labour is the **physiological process by which the fetus, placenta, and membranes are expelled from the uterus after fetal viability** through coordinated uterine contractions resulting in cervical effacement and dilatation. --- ## **Classification of Labour** * **Normal Labour**: Spontaneous onset, singleton, cephalic presentation, term pregnancy, no complications, vaginal delivery. * **Abnormal Labour**: Any deviation in onset, duration, progress, or outcome of labour. --- # **Normal Stages of Labour** ## **First Stage of Labour** **Definition:** Period from onset of true labour pains to full cervical dilatation (10 cm). ### **Phases** #### **Latent Phase** * Cervical dilatation: 0–3 cm * Cervical effacement occurs * Contractions mild to moderate * Duration: * Primigravida: up to 8 hours * Multigravida: up to 5 hours #### **Active Phase** * Cervical dilatation: 4–10 cm * Rapid dilatation * Strong, regular contractions * Rate of dilatation: * Primigravida: ~1 cm/hour * Multigravida: ~1.5 cm/hour ### **Normal Mechanism** * Uterine contractions * Cervical effacement and dilatation * Formation of forewaters and bulging membranes --- ## **Second Stage of Labour** **Definition:** Period from full cervical dilatation to delivery of the fetus. ### **Characteristics** * Strong expulsive uterine contractions * Voluntary maternal bearing down * Fetal descent, flexion, rotation, extension, restitution, expulsion ### **Duration** * Primigravida: up to 2 hours (3 hours with epidural) * Multigravida: up to 1 hour (2 hours with epidural) --- ## **Third Stage of Labour** **Definition:** Period from delivery of fetus to expulsion of placenta and membranes. ### **Mechanism** * Placental separation * Placental descent * Placental expulsion ### **Duration** * Usually within 5–15 minutes * Maximum acceptable: 30 minutes ### **Signs of Placental Separation** * Uterus becomes globular and firm * Lengthening of umbilical cord * Sudden gush of blood * Uterine fundus rises --- # **Abnormal Labour** Abnormal labour occurs due to problems related to **powers, passenger, or passage**. --- ## **Abnormalities of First Stage** ### **Prolonged Latent Phase** * > 8 hours in primigravida * > 5 hours in multigravida > **Causes** * Ineffective uterine contractions * Anxiety, dehydration * False labour **Management** * Reassurance * Hydration and analgesia * Rule out cephalopelvic disproportion --- ### **Protracted Active Phase** * Slow cervical dilatation **Causes** * Uterine inertia * Malposition * Mild CPD **Management** * Partograph monitoring * Amniotomy * Oxytocin augmentation if indicated --- ### **Arrest of Dilatation** * No cervical dilatation for 2 hours **Causes** * Obstructed labour * Malpresentation **Management** * Evaluate cause * Cesarean delivery if obstruction present --- ## **Abnormalities of Second Stage** ### **Prolonged Second Stage** * Exceeds normal duration **Causes** * Ineffective pushing * Epidural analgesia * Fetal malposition * Pelvic inadequacy **Complications** * Maternal exhaustion * Fetal distress **Management** * Assisted vaginal delivery * Cesarean section if indicated --- ### **Obstructed Labour** **Definition:** Failure of descent despite strong uterine contractions. **Causes** * Cephalopelvic disproportion * Fetal anomalies * Pelvic tumors **Complications** * Uterine rupture * Fetal hypoxia **Management** * Emergency cesarean section --- ## **Abnormalities of Third Stage** ### **Retained Placenta** * Placenta not expelled within 30 minutes **Types** * Placenta adherens * Trapped placenta * Placenta accreta spectrum **Management** * Active management * Manual removal under anesthesia --- ### **Postpartum Hemorrhage** * Blood loss >500 ml vaginal delivery **Causes** * Uterine atony * Retained placental tissue **Management** * Uterotonics * Bimanual compression * Surgical intervention if required --- # **Clinical Monitoring of Labour** * Partograph use * Fetal heart rate monitoring * Maternal vitals * Progress of cervical dilatation and descent --- # **Summary Table** | Stage | Normal Duration | Common Abnormalities | | ------ | --------------- | ---------------------- | | First | Latent + Active | Prolonged, Arrest | | Second | ≤2 hours | Prolonged, Obstructed | | Third | ≤30 minutes | Retained placenta, PPH | --- ## **Key Exam Pearls** * Active phase starts at 4 cm dilatation * Arrest disorders require prompt intervention * Third stage complications cause most maternal morbidity * Partograph is essential for early detection of abnormal labour --- If you want, I can **add MCQs, case based questions, management algorithms, or convert this into an exam-ready PDF or website content**.
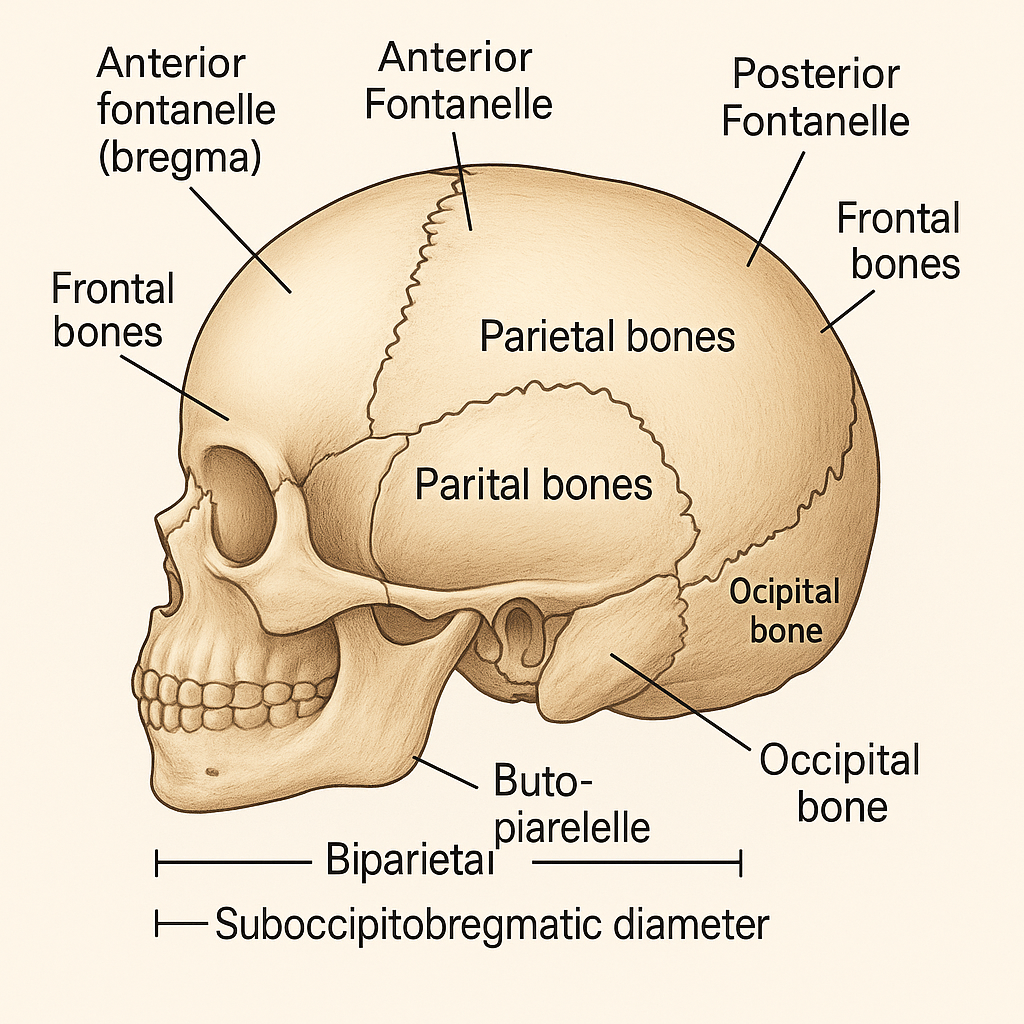
Fetal Skull Anatomy in Obstetrics: Sutures, Fontanelles, Diameters and Clinical Importance
## **SEO Title** **Fetal Skull Anatomy in Obstetrics: Sutures, Fontanelles, Diameters and Clinical Importance** ## **Meta Description** Comprehensive obstetrics-focused guide on fetal skull anatomy covering bones, sutures, fontanelles, diameters, molding, and their clinical significance during labor and delivery. ## **SEO Keywords** fetal skull obstetrics, fetal skull anatomy, sutures of fetal skull, fontanelles fetal skull, fetal skull diameters, molding of fetal skull, obstetric diameters, fetal head engagement, labor mechanism fetal skull --- # **Fetal Skull – Complete Obstetric Guide** ## **Introduction** The **fetal skull** is the most important part of the fetus in obstetrics because its **size, shape, flexibility, and diameters** determine the **mechanism of labor**, engagement, descent, and mode of delivery. --- ## **1. Structure of the Fetal Skull** The fetal skull is divided into **three main parts**: ### **A. Vault (Cranium) – Obstetrically Most Important** * Formed by **membranous bones** * Flexible and compressible * Allows **molding during labor** **Bones of the vault:** * 2 Frontal bones * 2 Parietal bones * Upper part of occipital bone --- ### **B. Base of the Skull** * Formed by **cartilaginous bones** * Rigid and non-compressible * Not affected by molding **Bones include:** * Sphenoid * Temporal * Lower occipital bone --- ### **C. Face** * Small obstetric significance * Important in **face presentation** --- ## **2. Sutures of the Fetal Skull** **Sutures** are fibrous joints between skull bones that allow overlapping during labor. | Suture | Location | Obstetric Importance | | ---------------------------- | ---------------------------------- | ---------------------------- | | **Sagittal suture** | Between parietal bones | Determines head position | | **Coronal suture** | Between frontal & parietal bones | Identifies degree of flexion | | **Lambdoid suture** | Between parietal & occipital bones | Helps locate occiput | | **Frontal (metopic) suture** | Between frontal bones | Indicates head attitude | --- ## **3. Fontanelles** Fontanelles are **membranous gaps** at the junction of sutures. ### **A. Anterior Fontanelle (Bregma)** * Diamond-shaped * Junction of **sagittal, coronal, and frontal sutures** * Closes by **18 months** * Palpation indicates **deflexed head** ### **B. Posterior Fontanelle (Lambda)** * Triangular * Junction of **sagittal and lambdoid sutures** * Closes by **6–8 weeks** * Palpation indicates **well-flexed vertex** **👉 Posterior fontanelle is the key landmark in normal labor** --- ## **4. Diameters of the Fetal Skull** Diameters are classified into **transverse and anteroposterior**. ### **A. Transverse Diameters** | Diameter | Measurement | Importance | | ----------------------------- | ----------- | ----------------- | | **Biparietal diameter (BPD)** | **9.5 cm** | Engaging diameter | | Bitemporal | 8 cm | Internal fit | | Bimastoid | 7.5 cm | Base diameter | --- ### **B. Anteroposterior Diameters** | Diameter | Measurement | Presentation | | ------------------------ | ----------- | -------------------------- | | **Suboccipitobregmatic** | **9.5 cm** | Well-flexed vertex (ideal) | | Suboccipitofrontal | 10 cm | Incomplete flexion | | Occipitofrontal | 11.5 cm | Deflexed vertex | | Mentovertical | 13.5 cm | Brow presentation | | Submentobregmatic | 9.5 cm | Face presentation | --- ## **5. Circumferences of the Fetal Head** | Circumference | Measurement | | -------------------- | ----------- | | Suboccipitobregmatic | ~32 cm | | Occipitofrontal | ~34 cm | | Mentovertical | ~38 cm | --- ## **6. Molding of the Fetal Skull** **Molding** refers to **overlapping of skull bones during labor**. ### **Grades of Molding** * **+ (Mild):** Sutures touching * **++ (Moderate):** Sutures overlapping but reducible * **+++ (Severe):** Overlapping not reducible (suggests CPD) **Clinical Importance** * Facilitates vaginal delivery * Excessive molding → fetal distress or obstructed labor --- ## **7. Caput Succedaneum** * Edematous swelling of scalp * Crosses suture lines * Appears at birth * Resolves spontaneously --- ## **8. Cephalhematoma** * Subperiosteal hemorrhage * Does **not cross suture lines** * Appears hours after birth * Resolves slowly --- ## **9. Obstetric Importance of the Fetal Skull** * Determines **engagement** * Helps assess **presentation and position** * Influences **mechanism of labor** * Guides **decision for vaginal delivery vs cesarean** * Critical in diagnosing **CPD and malpresentations** --- ## **Key Clinical Points** * **Best diameter for vaginal delivery:** Suboccipitobregmatic (9.5 cm) * **Most dangerous presentation:** Brow (mentovertical 13.5 cm) * **Posterior fontanelle palpable → normal vertex** * **Excessive molding → obstructed labor** --- If you want, I can also provide: * **SEO FAQs** * **Exam-oriented tables** * **25 hard case-based MCQs in HTML/CSS/JS (single file, modern UI)** * **Illustration prompts for image generation** Just tell me 👍

Contracted Pelvis and Cephalopelvic Disproportion Types Diagnosis Management
Below is a **concise yet complete, exam-oriented and SEO-friendly medical reference** covering **Contracted Pelvis, Cephalopelvic Disproportion (CPD), and Types of Pelvis**. Structured with **H1–H4 headings**, keyword-rich language, and clear clinical flow. **No images included**, as requested. --- # Contracted Pelvis and Cephalopelvic Disproportion: Types, Diagnosis and Management ## Introduction **Contracted pelvis** and **cephalopelvic disproportion (CPD)** are major causes of **obstructed labor**, **prolonged labor**, and **operative delivery**. Understanding **pelvic anatomy**, **pelvic types**, and **fetal–pelvic relationships** is essential for safe obstetric practice. --- ## Contracted Pelvis ### Definition A **contracted pelvis** is a pelvis in which **one or more pelvic diameters are reduced** below normal, interfering with the **descent and delivery of the fetus**. --- ### Causes of Contracted Pelvis #### Developmental Causes * Congenital pelvic abnormalities * Malnutrition during childhood * Rickets and osteomalacia #### Acquired Causes * Pelvic fractures with malunion * Tuberculosis of bones * Spinal deformities (kyphosis, scoliosis) * Previous pelvic surgery --- ### Classification of Contracted Pelvis #### 1. Anatomical Contracted Pelvis * **True contraction** of one or more diameters * Diagnosed by **pelvimetry** #### 2. Functional Contracted Pelvis * Pelvic diameters normal * Obstruction due to: * Large fetus * Malposition or malpresentation * Deflexed fetal head --- ### Degrees of Contracted Pelvis (Based on Obstetric Conjugate) | Degree | Obstetric Conjugate | Clinical Significance | | -------- | ------------------- | ------------------------- | | Mild | 9–10 cm | Vaginal delivery possible | | Moderate | 7.5–9 cm | Trial of labor | | Severe | <7.5 cm | Cesarean section | --- ## Cephalopelvic Disproportion (CPD) ### Definition **Cephalopelvic disproportion** occurs when the **fetal head is too large** or the **maternal pelvis too small** to allow vaginal delivery. --- ### Types of CPD #### 1. Absolute CPD * Gross pelvic contraction * Vaginal delivery **impossible** #### 2. Relative CPD * Borderline pelvis * Delivery depends on: * Fetal head molding * Position and attitude * Strength of uterine contractions --- ### Causes of CPD #### Maternal Factors * Contracted pelvis * Pelvic tumors * Short stature #### Fetal Factors * Macrosomia * Hydrocephalus * Occipitoposterior position * Deflexed head --- ### Clinical Features of CPD * Failure of head engagement * Prolonged labor * Cervical dystocia * Increasing caput and molding * Maternal exhaustion * Fetal distress --- ### Diagnosis of CPD #### Antenatal Assessment * History of difficult labor * Clinical pelvimetry * Ultrasound for fetal weight #### Intrapartum Diagnosis * Lack of descent despite good contractions * Non-progress of labor * Rising Bandl’s ring --- ### Management of CPD #### Antenatal * Identify high-risk cases * Plan mode of delivery #### Intrapartum * **Trial of labor** in selected cases * Continuous maternal and fetal monitoring #### Definitive Management * **Cesarean section** for: * Absolute CPD * Failed trial of labor * Fetal distress --- ## Types of Pelvis (Caldwell–Moloy Classification) ### 1. Gynecoid Pelvis * Most favorable for vaginal delivery * Rounded inlet * Wide subpubic angle * Straight side walls --- ### 2. Android Pelvis * Male-type pelvis * Heart-shaped inlet * Narrow mid-pelvis * Common cause of **arrest of descent** --- ### 3. Anthropoid Pelvis * Oval inlet (anteroposterior diameter increased) * Occipitoposterior position common * Vaginal delivery usually possible --- ### 4. Platypelloid Pelvis * Flattened pelvis * Wide transverse diameter * Narrow anteroposterior diameter * Engagement delayed --- ## Comparison of Pelvic Types | Pelvic Type | Inlet Shape | Labor Outcome | | ------------ | ------------ | ------------------ | | Gynecoid | Round | Best | | Android | Heart-shaped | Difficult | | Anthropoid | Oval (AP) | OP common | | Platypelloid | Flat | Engagement delayed | --- ## Clinical Importance * Major determinant of **mode of delivery** * Prevention of **obstructed labor** * Reduces maternal and perinatal morbidity * Essential for **exam preparation** and **clinical decision-making** --- ## Conclusion **Contracted pelvis and CPD** remain critical challenges in obstetrics. Accurate **pelvic assessment**, understanding **pelvic types**, and timely intervention ensure safe outcomes for both mother and fetus. --- ### SEO Keywords (Comma-Separated) contracted pelvis, cephalopelvic disproportion, CPD in obstetrics, types of pelvis, gynecoid pelvis, android pelvis, anthropoid pelvis, platypelloid pelvis, obstructed labor causes, pelvic contraction degrees, CPD diagnosis management If you want, I can also provide **case-based MCQs**, **exam notes**, or a **single-file HTML CSS JS quiz** on this topic.
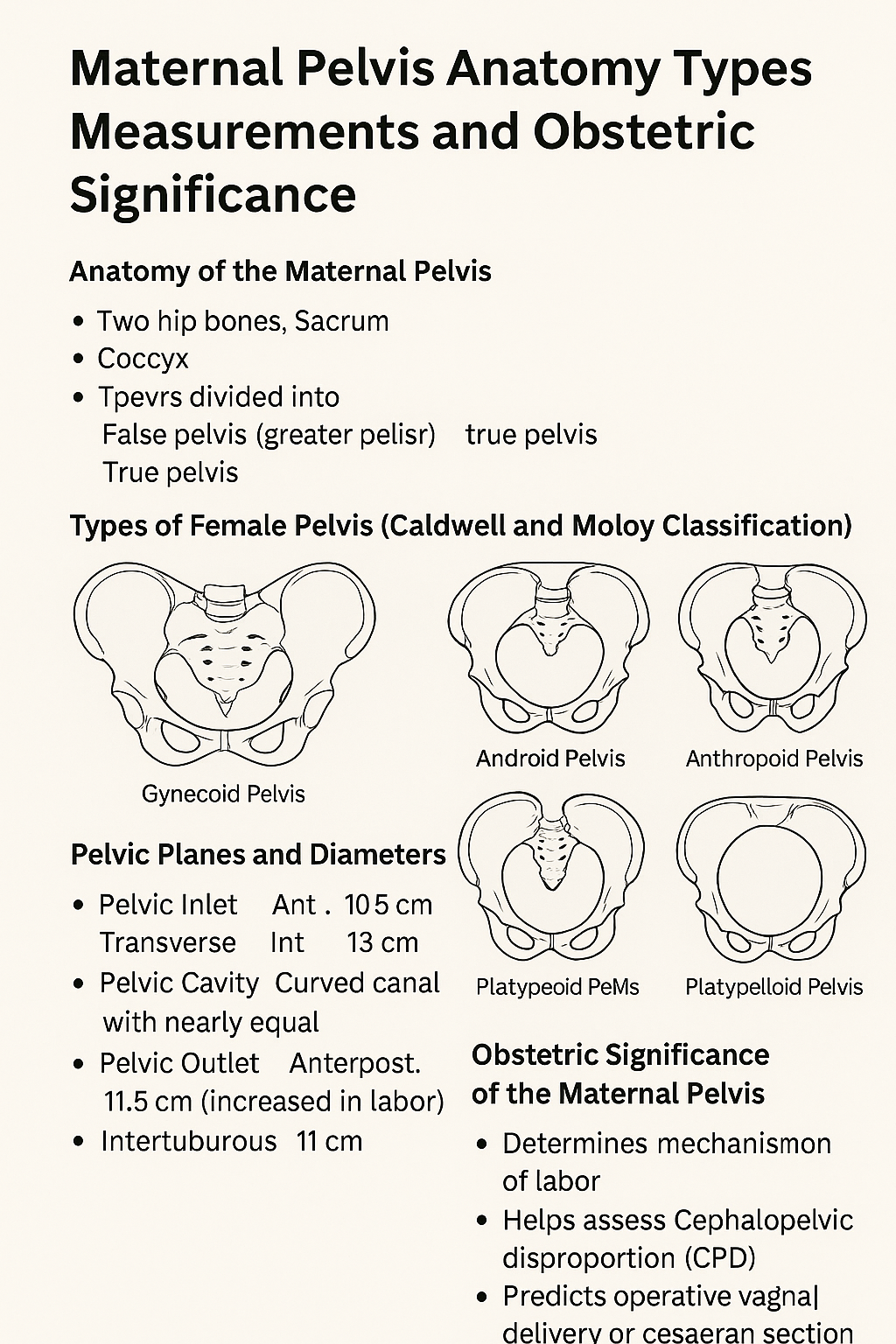
Maternal Pelvis Anatomy Types Measurements and Obstetric Significance
# **Maternal Pelvis Anatomy Types Measurements and Obstetric Significance** ## **Introduction** The **maternal pelvis** is a rigid bony structure that forms the birth canal. Its **shape, size, and dimensions** are critical determinants of **labor progression, fetal descent, and delivery outcome**. In obstetrics, detailed assessment of the maternal pelvis helps predict **normal vaginal delivery, obstructed labor, and cephalopelvic disproportion**. --- ## **Anatomy of the Maternal Pelvis** ### **1. Bones Forming the Pelvis** * **Two hip bones** (each formed by ilium, ischium, and pubis) * **Sacrum** * **Coccyx** These bones unite to form a **bony ring** that supports pelvic organs and provides a passage for childbirth. --- ## **Divisions of the Maternal Pelvis** ### **1. False Pelvis (Greater Pelvis)** * Located above the pelvic brim * Supports the gravid uterus * Has **no direct role in labor** ### **2. True Pelvis (Lesser Pelvis)** * Located below the pelvic brim * Forms the **birth canal** * Obstetrically important part --- ## **Pelvic Brim (Inlet)** The pelvic brim separates the false and true pelvis. ### **Boundaries** * Sacral promontory (posterior) * Ala of sacrum * Linea terminalis * Upper border of pubic symphysis (anterior) --- ## **Planes and Diameters of the Maternal Pelvis** ### **1. Pelvic Inlet** **Important diameters** * **Anteroposterior (Obstetric conjugate)**: ~10.5 cm * **Transverse diameter**: ~13 cm * **Oblique diameter**: ~12 cm **Clinical importance** * Determines engagement of fetal head --- ### **2. Pelvic Cavity** * Curved canal with nearly equal AP and transverse diameters * Smooth lateral walls favor rotation of the fetal head --- ### **3. Pelvic Outlet** **Boundaries** * Ischial tuberosities * Coccyx * Lower border of pubic arch **Important diameters** * **Anteroposterior**: ~11.5 cm (increases during labor due to coccygeal movement) * **Intertuberous diameter**: ~11 cm **Clinical importance** * Determines completion of vaginal delivery --- ## **Types of Female Pelvis (Caldwell and Moloy Classification)** ### **1. Gynecoid Pelvis** * Rounded inlet * Wide subpubic angle * Straight side walls **Most favorable for vaginal delivery** ### **2. Android Pelvis** * Heart-shaped inlet * Narrow forepelvis * Prominent ischial spines **Associated with deep transverse arrest** ### **3. Anthropoid Pelvis** * Oval inlet with long AP diameter * Favors occipitoposterior positions **Vaginal delivery usually possible** ### **4. Platypelloid Pelvis** * Flattened inlet * Wide transverse diameter * Short AP diameter **Engagement may be difficult** --- ## **Obstetric Significance of the Maternal Pelvis** * Determines **mechanism of labor** * Helps assess **cephalopelvic disproportion** * Predicts **operative vaginal delivery or cesarean section** * Influences fetal head **engagement, rotation, and descent** --- ## **Clinical Assessment of the Maternal Pelvis** ### **1. Clinical Pelvimetry** * Performed per vaginum * Assesses pelvic inlet, cavity, and outlet ### **2. Imaging Pelvimetry** * X-ray, CT, or MRI pelvimetry * Reserved for selected cases --- ## **Common Obstetric Problems Related to Pelvis** * Contracted pelvis * Obstructed labor * Prolonged labor * Fetal malposition and malrotation --- ## **Conclusion** The **maternal pelvis** plays a decisive role in childbirth. Knowledge of **pelvic anatomy, dimensions, and pelvic types** is essential for safe obstetric practice, early identification of labor complications, and appropriate delivery planning. --- ### **SEO Keywords** maternal pelvis anatomy, types of female pelvis, obstetric pelvis, pelvic inlet outlet diameters, gynecoid pelvis, android pelvis, anthropoid pelvis, platypelloid pelvis, pelvic planes obstetrics, clinical pelvimetry If you want, I can **generate 25 hard case-based MCQs in a single HTML CSS JS file**, or **convert this into exam notes or infographic-ready content**.
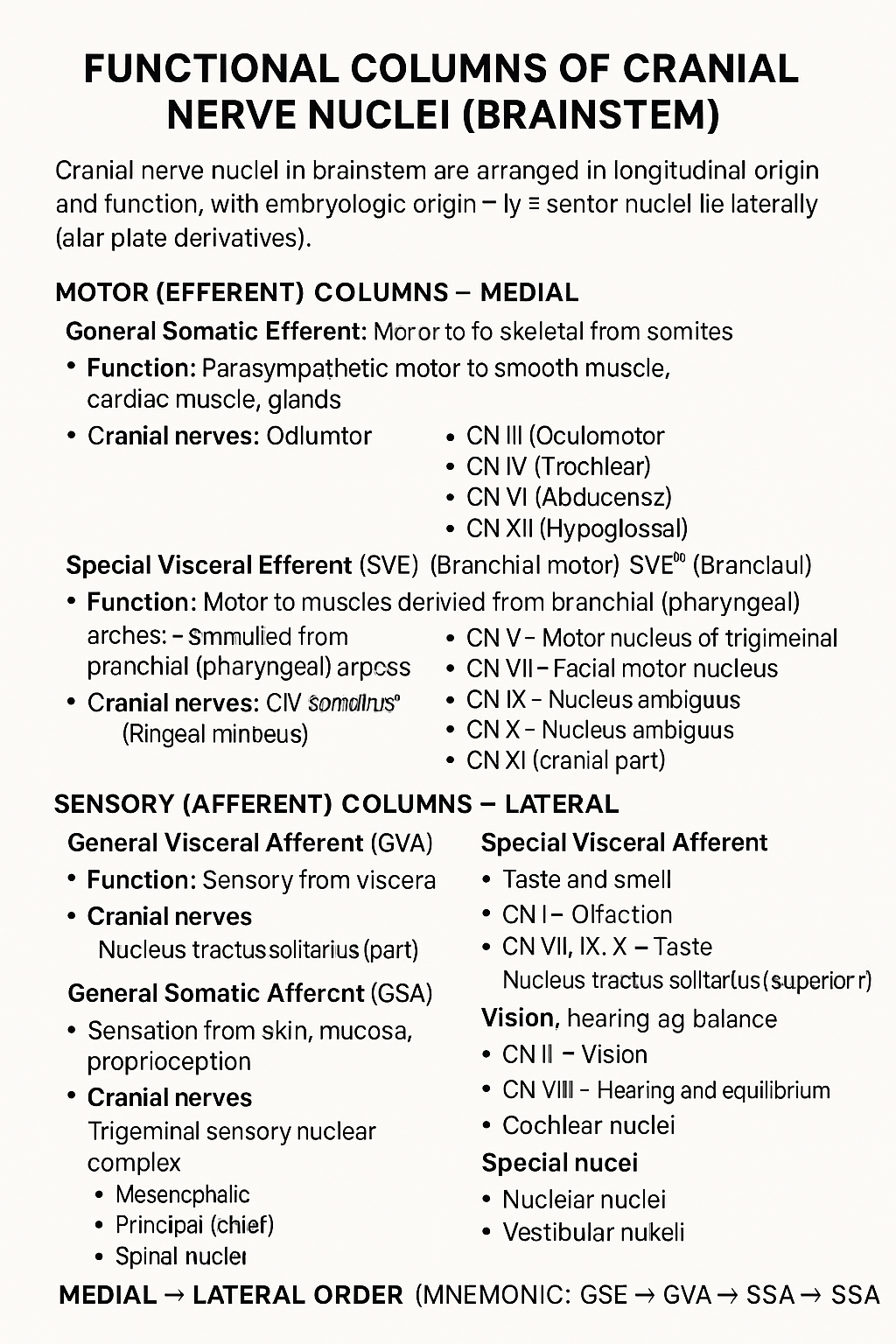
Functional Columns of Cranial Nerve Nuclei in Brainstem
## Functional Columns of Cranial Nerve Nuclei (Brainstem) Cranial nerve nuclei in the brainstem are arranged in **longitudinal functional columns** based on **embryologic origin** and **function**. **Motor nuclei lie medially** (basal plate derivatives) and **sensory nuclei lie laterally** (alar plate derivatives). --- ## MOTOR (EFFERENT) COLUMNS – Medial ### 1. **General Somatic Efferent (GSE)** * **Function:** Motor to skeletal muscles derived from **somites** * **Muscles supplied:** Extraocular muscles, tongue muscles * **Cranial nerves:** * CN III (Oculomotor) * CN IV (Trochlear) * CN VI (Abducens) * CN XII (Hypoglossal) --- ### 2. **General Visceral Efferent (GVE)** * **Function:** **Parasympathetic** motor to smooth muscle, cardiac muscle, glands * **Cranial nerves & nuclei:** * CN III – Edinger–Westphal nucleus * CN VII – Superior salivatory nucleus * CN IX – Inferior salivatory nucleus * CN X – Dorsal motor nucleus of vagus --- ### 3. **Special Visceral Efferent (SVE)** *(Branchial motor)* * **Function:** Motor to muscles derived from **branchial (pharyngeal) arches** * **Muscles supplied:** Muscles of mastication, facial expression, pharynx, larynx * **Cranial nerves:** * CN V – Motor nucleus of trigeminal * CN VII – Facial motor nucleus * CN IX – Nucleus ambiguus * CN X – Nucleus ambiguus * CN XI (cranial part) --- ## SENSORY (AFFERENT) COLUMNS – Lateral ### 4. **General Visceral Afferent (GVA)** * **Function:** Sensory from viscera * **Cranial nerves:** * CN IX * CN X * **Nucleus:** Nucleus tractus solitarius (inferior part) --- ### 5. **Special Visceral Afferent (SVA)** * **Function:** Taste and smell * **Cranial nerves:** * CN I – Olfaction * CN VII, IX, X – Taste * **Nucleus:** Nucleus tractus solitarius (superior part) --- ### 6. **General Somatic Afferent (GSA)** * **Function:** Sensation from skin, mucosa, proprioception * **Cranial nerves:** * CN V (main) * CN VII, IX, X (small contributions) * **Nuclei:** * Trigeminal sensory nuclear complex * Mesencephalic * Principal (chief) * Spinal nucleus --- ### 7. **Special Somatic Afferent (SSA)** * **Function:** Vision, hearing, balance * **Cranial nerves:** * CN II – Vision * CN VIII – Hearing and equilibrium * **Nuclei:** * Cochlear nuclei * Vestibular nuclei --- ## MEDIAL → LATERAL ORDER (Mnemonic) **GSE → GVE → SVE → GVA → SVA → GSA → SSA** --- If you want, I can also provide: * **One-table summary (exam revision)** * **Clinical correlations** * **Simple mnemonics for each column** * **Neat labelled text diagram (ASCII-style)**
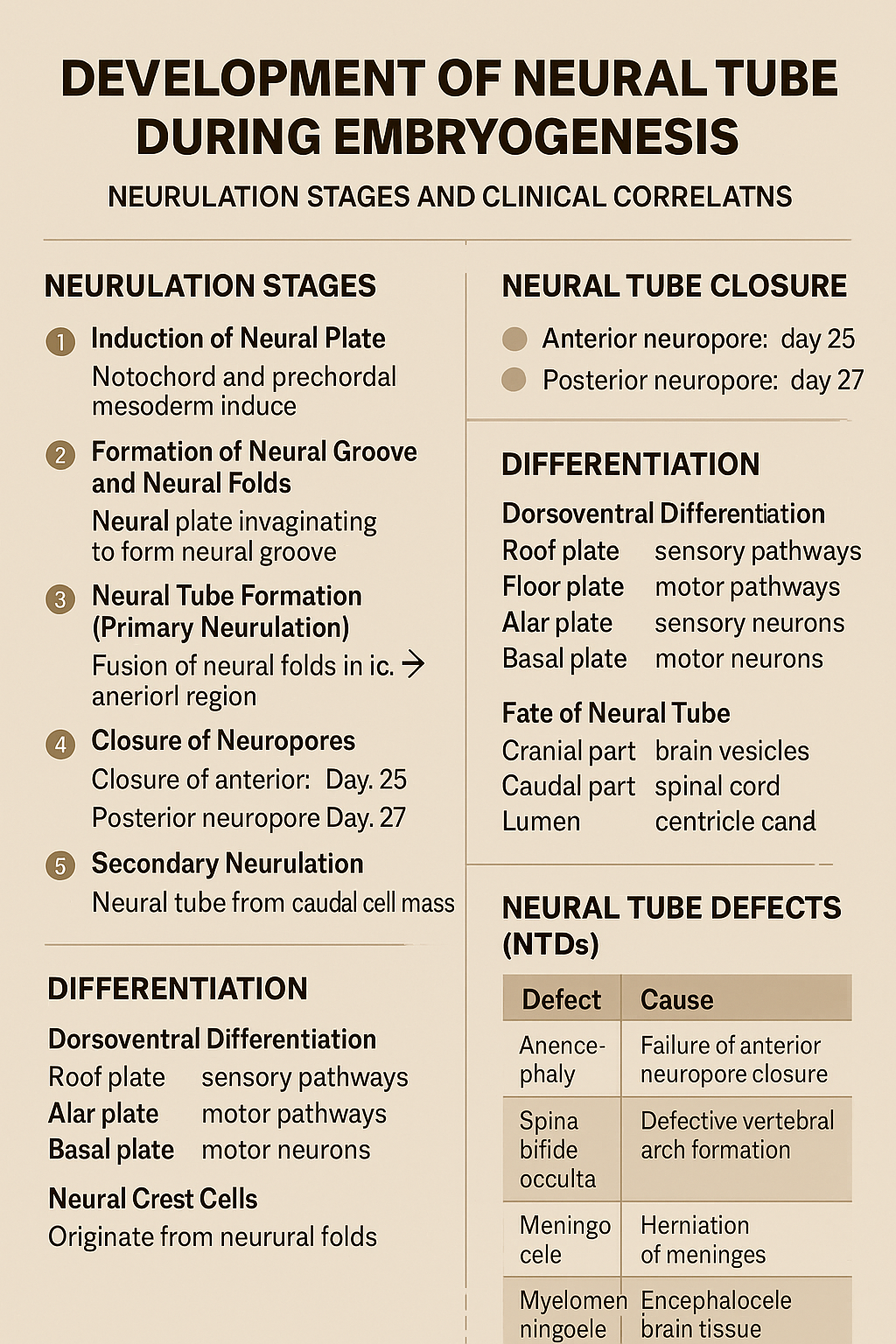
Development of Neural Tube During Embryogenesis Neurulation Stages and Clinical Correlation
## Development of the Neural Tube (Neurulation) ### **Definition** The **neural tube** is the embryonic precursor of the **central nervous system (CNS)**, forming the **brain and spinal cord**. Its development occurs by **neurulation** during the **3rd and 4th weeks of intrauterine life**. --- ## **Timeline** * **Day 18**: Neural plate appears * **Day 20–21**: Neural folds form * **Day 22**: Fusion begins in cervical region * **Day 25**: Closure of anterior (cranial) neuropore * **Day 27**: Closure of posterior (caudal) neuropore --- ## **Phases of Neural Tube Development** ### **1. Induction of Neural Plate** * The **notochord** and **prechordal mesoderm** induce overlying **ectoderm**. * Ectoderm thickens to form the **neural plate**. **Key signaling molecules**: * Sonic hedgehog (Shh) * Noggin * Chordin * Follistatin --- ### **2. Formation of Neural Groove and Neural Folds** * Central neural plate invaginates → **neural groove**. * Lateral edges elevate → **neural folds**. * Neural folds approach each other dorsally. --- ### **3. Neural Tube Formation (Primary Neurulation)** * Neural folds fuse in the **midline**, starting in the **cervical region**. * Fusion proceeds cranially and caudally. * Temporary openings remain: * **Anterior (cranial) neuropore** * **Posterior (caudal) neuropore** --- ### **4. Closure of Neuropores** * **Anterior neuropore closes (Day 25)** → brain development * **Posterior neuropore closes (Day 27)** → spinal cord development Failure of closure leads to **neural tube defects**. --- ### **5. Secondary Neurulation** * Occurs in the **caudal region (below S2)**. * Neural tube forms from **caudal cell mass**. * Important for formation of: * Conus medullaris * Filum terminale --- ## **Differentiation of the Neural Tube** ### **Neural Tube Wall Layers** 1. **Ventricular (ependymal) layer** – neuroepithelial cells 2. **Mantle layer** – gray matter 3. **Marginal layer** – white matter --- ### **Dorsoventral Differentiation** * **Roof plate** → sensory pathways * **Floor plate** → motor pathways * **Alar plate** → sensory neurons * **Basal plate** → motor neurons * **Sulcus limitans** separates alar and basal plates --- ## **Fate of Neural Tube** * **Cranial part** → brain vesicles * Prosencephalon * Mesencephalon * Rhombencephalon * **Caudal part** → spinal cord * **Lumen** → ventricles and central canal --- ## **Neural Crest Cells (Related Event)** * Originate from neural folds * Migrate extensively * Form: * Peripheral nervous system * Melanocytes * Adrenal medulla * Craniofacial cartilage --- ## **Clinical Correlation: Neural Tube Defects (NTDs)** | Defect | Cause | | -------------------- | ------------------------------------- | | Anencephaly | Failure of anterior neuropore closure | | Spina bifida occulta | Defective vertebral arch formation | | Meningocele | Herniation of meninges | | Myelomeningocele | Herniation of spinal cord + meninges | | Encephalocele | Herniation of brain tissue | **Risk factors**: * Folic acid deficiency * Maternal diabetes * Valproate exposure **Prevention**: * Folic acid 400–800 µg/day (preconception) --- ### **One-Line Exam Summary** > The neural tube forms from ectoderm by neurulation during weeks 3–4 and develops into the brain and spinal cord. If you want, I can also provide **exam-oriented MCQs, flowcharts, or comparison tables** for neurulation.
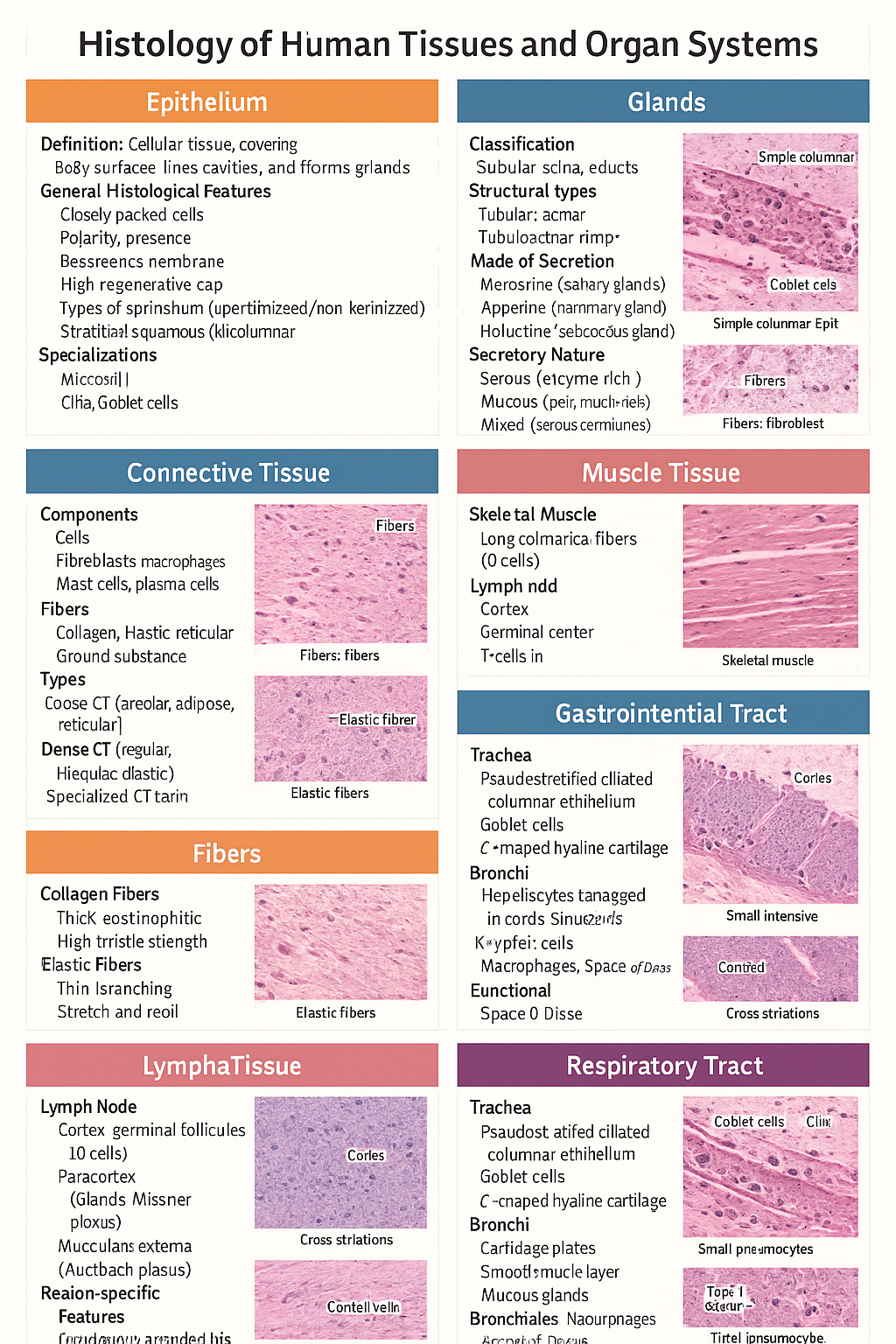
Histology of Epithelium, Connective Tissue, Muscle, Cartilage, Glands, GIT, Liver and Respiratory Tract
Below is a **single-place, SEO-optimized, exam-ready histology guide** covering **epithelium, glands, connective tissue, fibers, cartilage, muscle, lymphatic system, GIT, liver, and respiratory tract**. Structured with **clear H1–H3 headings**, **high-yield features**, and **clinical correlations** for medical students and competitive exams. --- # Histology of Human Tissues and Organ Systems – Complete Guide ## Histology of Epithelium ### Definition Epithelium is a **cellular tissue** that covers body surfaces, lines cavities, and forms glands. ### General Histological Features * Closely packed cells with **minimal extracellular matrix** * **Polarity**: apical, lateral, basal surfaces * **Basement membrane** present * **Avascular**, richly innervated * High **regenerative capacity** ### Types of Epithelium * **Simple squamous**: alveoli, capillaries * **Simple cuboidal**: kidney tubules, glands * **Simple columnar**: stomach, intestine * **Stratified squamous (keratinized/non-keratinized)**: skin / oral cavity * **Pseudostratified ciliated columnar**: trachea * **Transitional epithelium**: urinary bladder ### Specializations * **Microvilli** – absorption * **Cilia** – movement * **Goblet cells** – mucus secretion --- ## Histology of Glands ### Classification * **Exocrine glands** – ducts present * **Endocrine glands** – ductless, secrete into blood ### Structural Types * **Tubular**, **acinar**, **tubuloacinar** * **Simple** or **compound** ### Mode of Secretion * **Merocrine** (salivary glands) * **Apocrine** (mammary gland) * **Holocrine** (sebaceous gland) ### Secretory Nature * **Serous** – enzyme-rich, dark staining * **Mucous** – pale, mucin-rich * **Mixed** – serous demilunes --- ## Histology of Connective Tissue ### Components * **Cells**: fibroblasts, macrophages, mast cells, plasma cells * **Fibers**: collagen, elastic, reticular * **Ground substance**: proteoglycans, GAGs ### Types * **Loose CT**: areolar, adipose, reticular * **Dense CT**: regular, irregular, elastic * **Specialized CT**: cartilage, bone, blood --- ## Histology of Fibers ### Collagen Fibers * Thick, eosinophilic * High tensile strength * Seen in tendons, ligaments ### Elastic Fibers * Thin, branching * Stretch and recoil * Found in lungs, elastic arteries ### Reticular Fibers * Type III collagen * Supportive network * Seen in lymphoid organs --- ## Histology of Cartilage ### General Features * Avascular * Chondrocytes in **lacunae** * Perichondrium present (except articular cartilage) ### Types * **Hyaline cartilage**: trachea, articular surfaces * **Elastic cartilage**: pinna, epiglottis * **Fibrocartilage**: intervertebral discs, pubic symphysis --- ## Histology of Muscle Tissue ### Skeletal Muscle * Long cylindrical fibers * **Multinucleated**, peripheral nuclei * Cross striations present * Voluntary ### Cardiac Muscle * Branching fibers * Single central nucleus * **Intercalated discs** * Involuntary ### Smooth Muscle * Spindle-shaped cells * No striations * Involuntary * Found in viscera, vessels --- ## Histology of Lymphatic System ### Lymph Node * Capsule with trabeculae * **Cortex**: lymphoid follicles (B cells) * **Paracortex**: T cells * **Medulla**: medullary cords and sinuses ### Spleen * **White pulp**: lymphocytes around central artery * **Red pulp**: sinusoids and splenic cords ### Thymus * Cortex and medulla * **Hassall’s corpuscles** * T-cell maturation --- ## Histology of Gastrointestinal Tract (GIT) ### Common Layers 1. **Mucosa** – epithelium, lamina propria, muscularis mucosa 2. **Submucosa** – glands, Meissner plexus 3. **Muscularis externa** – Auerbach plexus 4. **Serosa/adventitia** ### Region-Specific Features * **Esophagus**: stratified squamous epithelium * **Stomach**: simple columnar epithelium, gastric glands * **Small intestine**: villi, plicae circulares, Peyer’s patches (ileum) * **Colon**: no villi, abundant goblet cells --- ## Histology of Liver ### Structural Unit * **Classical hepatic lobule** * Central vein * Portal triad: hepatic artery, portal vein, bile duct ### Cellular Features * Hepatocytes arranged in cords * **Sinusoids** lined by fenestrated endothelium * **Kupffer cells** – macrophages * **Space of Disse** ### Functional Significance * Metabolism * Detoxification * Bile production --- ## Histology of Respiratory Tract ### Trachea * Pseudostratified ciliated columnar epithelium * Goblet cells * C-shaped hyaline cartilage ### Bronchi * Cartilage plates * Smooth muscle layer * Mucous glands ### Bronchioles * No cartilage or glands * Simple ciliated columnar → cuboidal epithelium ### Alveoli * **Type I pneumocytes** – gas exchange * **Type II pneumocytes** – surfactant * Alveolar macrophages --- ## High-Yield Exam Pearls * Transitional epithelium is **unique to urinary tract** * Fibrocartilage **lacks perichondrium** * Peyer’s patches are characteristic of **ileum** * Kupffer cells are **liver macrophages** * Type II pneumocytes produce **surfactant** --- If you want, I can next: * ✅ Convert this into **HTML-CSS-JS single-file notes** * ✅ Add **labeled histology images** * ✅ Generate **25 image-based MCQs** * ✅ Create **printable PDF or exam charts** Just tell me 👍

Post Term Pregnancy and Fetal Macrosomia Causes Risks Diagnosis and Management
Below is a **SEO-friendly, exam-oriented, and clinically complete guide** on **Post-Term Pregnancy and Fetal Macrosomia**, written in clear **H1–H3 structure** and optimized for medical websites. --- ## **SEO Title** **Post Term Pregnancy and Fetal Macrosomia Clinical Guide 2025** --- ## **SEO Meta Description** Comprehensive medical guide on post term pregnancy and fetal macrosomia covering definition, causes, risks, diagnosis, management, induction of labor, complications, and prevention for obstetric practice and exams. --- ## **SEO Keywords** post term pregnancy, postdated pregnancy management, fetal macrosomia, macrosomia causes, post term pregnancy complications, induction of labor post term, macrosomic baby risks, shoulder dystocia, large for gestational age fetus, obstetrics clinical guide --- # **Post Term Pregnancy and Fetal Macrosomia** ## **1. Post Term Pregnancy** ### **Definition** Post term pregnancy is defined as a pregnancy that **extends beyond 42 completed weeks (≥294 days)** from the first day of the last menstrual period. --- ### **Classification** * **Late term:** 41⁰–41⁶ weeks * **Post term:** ≥42⁰ weeks --- ### **Etiology and Risk Factors** * Incorrect dating of pregnancy * Primigravida * Previous post term pregnancy * Male fetus * Maternal obesity * Genetic factors --- ### **Pathophysiology** * Progressive **placental aging and insufficiency** * Reduced uteroplacental perfusion * Oligohydramnios * Increased risk of fetal hypoxia --- ### **Maternal Complications** * Prolonged labor * Increased operative delivery * Perineal trauma * Postpartum hemorrhage * Infection --- ### **Fetal and Neonatal Complications** * Macrosomia * Meconium aspiration syndrome * Shoulder dystocia * Birth asphyxia * Stillbirth * Postmaturity syndrome (dry, peeling skin, decreased fat) --- ### **Diagnosis** * Accurate gestational age assessment (early ultrasound) * Fundal height * Ultrasound for: * Amniotic fluid index (AFI) * Estimated fetal weight * Fetal surveillance: * Non-stress test (NST) * Biophysical profile (BPP) --- ### **Management** * **41 weeks:** Begin antenatal surveillance * **≥41–42 weeks:** Induction of labor * **Cervical ripening:** Prostaglandins or Foley catheter * **Cesarean section:** If failed induction or fetal distress --- ## **2. Fetal Macrosomia** ### **Definition** Fetal macrosomia refers to a fetus with **birth weight ≥4,000 g** (some definitions use ≥4,500 g), irrespective of gestational age. --- ### **Risk Factors** * Maternal diabetes (gestational or pregestational) * Post term pregnancy * Maternal obesity * Excessive gestational weight gain * Multiparity * Previous macrosomic infant * Male fetus --- ### **Pathophysiology** * Maternal hyperglycemia → fetal hyperinsulinemia * Increased fat deposition and organ enlargement * Disproportionate growth of shoulders and trunk --- ### **Maternal Complications** * Prolonged labor * Operative vaginal delivery * Cesarean section * Postpartum hemorrhage * Genital tract injuries --- ### **Fetal and Neonatal Complications** * Shoulder dystocia * Brachial plexus injury * Clavicle fracture * Birth asphyxia * Neonatal hypoglycemia * Childhood obesity and metabolic syndrome --- ### **Diagnosis** * Clinical assessment (fundal height, Leopold maneuvers) * Ultrasound estimated fetal weight (EFW) * Limitations: ±10–15% error in late pregnancy --- ### **Management** * **Antenatal** * Optimize glycemic control * Monitor fetal growth * **Intrapartum** * Trial of labor if EFW <4,500 g (non-diabetic) * Elective cesarean if: * EFW ≥4,500 g (diabetic mother) * EFW ≥5,000 g (non-diabetic) * **Preparedness** * Anticipate shoulder dystocia * Skilled birth attendants --- ## **3. Relationship Between Post Term Pregnancy and Macrosomia** * Prolonged gestation allows continued fetal growth * Increased risk of large for gestational age fetus * Higher rates of operative delivery and birth trauma * Combined risk increases perinatal morbidity --- ## **4. Prevention Strategies** * Accurate pregnancy dating (first-trimester ultrasound) * Timely induction at 41 weeks * Optimal maternal weight and glucose control * Regular antenatal follow-up --- ## **5. Key Clinical Pearls** * Post term pregnancy significantly increases perinatal mortality * Macrosomia cannot be diagnosed with certainty antenatally * Induction at 41 weeks reduces stillbirth risk * Shoulder dystocia is the most feared complication of macrosomia --- If you want, I can next: * **Generate exam-oriented MCQs (HTML CSS JS single file)** * **Create FAQ schema for SEO** * **Generate medical illustrations** * **Convert this into a publish-ready SEO article page**
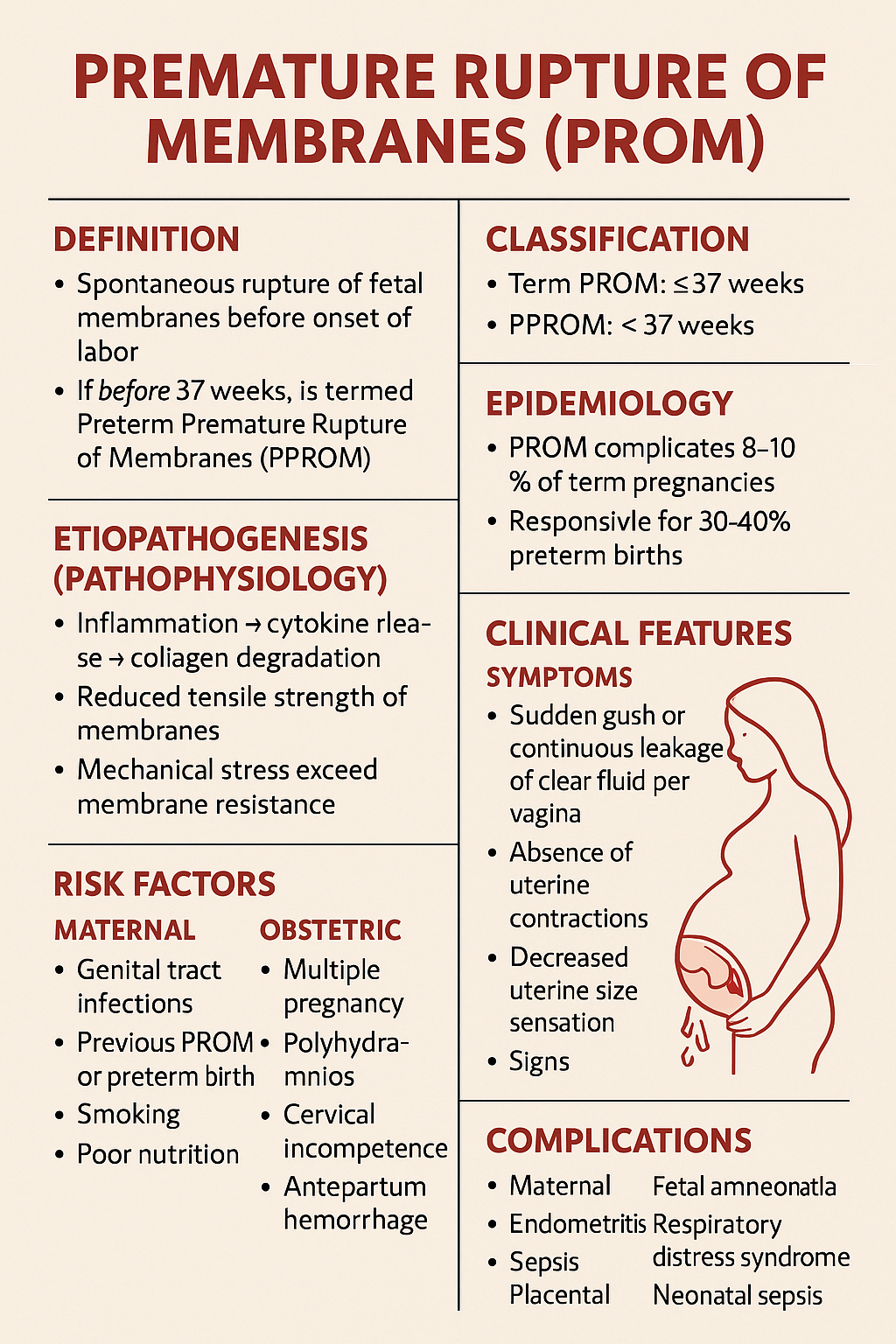
Premature Rupture of Membranes PROM – Causes Diagnosis Management and Complications
Below is a **complete, SEO-friendly, exam-oriented, single-place medical reference** on **Premature Rupture of Membranes (PROM)**, structured with clear **H1–H4 headings**, rich keywords, and clinically accurate content suitable for **medical students, clinicians, and health websites**. --- # **Premature Rupture of Membranes (PROM)** ## **Definition** **Premature Rupture of Membranes (PROM)** is defined as **spontaneous rupture of the fetal membranes before the onset of labor**, irrespective of gestational age. * If it occurs **before 37 completed weeks**, it is termed **Preterm Premature Rupture of Membranes (PPROM)**. --- ## **Classification** ### **1. Based on Gestational Age** * **Term PROM**: ≥ 37 weeks * **PPROM**: < 37 weeks ### **2. Based on Duration** * **Recent PROM**: < 18 hours * **Prolonged PROM**: ≥ 18 hours (↑ risk of infection) --- ## **Epidemiology** * PROM complicates **8–10% of term pregnancies** * PPROM accounts for **2–3% of all pregnancies** * Responsible for **30–40% of preterm births** --- ## **Etiopathogenesis (Pathophysiology)** ### **Normal Membrane Integrity** * Maintained by **collagen, elastin, and extracellular matrix** * Balance between **matrix synthesis and degradation** ### **Mechanisms Leading to PROM** * **Inflammation → cytokine release → collagen degradation** * **Reduced tensile strength of membranes** * **Mechanical stress exceeding membrane resistance** --- ## **Risk Factors** ### **Maternal Factors** * Genital tract infections (BV, UTI, STIs) * Previous PROM or preterm birth * Smoking * Poor nutrition * Low socioeconomic status ### **Obstetric Factors** * Multiple pregnancy * Polyhydramnios * Cervical incompetence * Antepartum hemorrhage ### **Iatrogenic Factors** * Amniocentesis * Cervical procedures --- ## **Clinical Features** ### **Symptoms** * Sudden **gush or continuous leakage of clear fluid per vagina** * Absence of uterine contractions initially * Decreased uterine size sensation ### **Signs** * Pooling of liquor in posterior fornix * Wet perineum * Reduced amniotic fluid volume --- ## **Diagnosis** ### **History** * Timing, amount, color, and odor of fluid * Associated fever, pain, reduced fetal movements ### **Physical Examination** * **Sterile speculum examination (preferred)** * Avoid digital vaginal examination unless in labor --- ### **Confirmatory Tests** #### **1. Bedside Tests** * **Nitrazine test**: Alkaline pH (false positives possible) * **Fern test**: Crystallization pattern on microscopy #### **2. Biochemical Tests** * PAMG-1 (AmniSure) * IGFBP-1 (Actim PROM) #### **3. Ultrasound** * Reduced Amniotic Fluid Index (AFI) * Assessment of fetal growth and presentation --- ## **Differential Diagnosis** * Urinary incontinence * Physiological vaginal discharge * Seminal fluid * Vaginal infections --- ## **Complications** ### **Maternal** * Chorioamnionitis * Endometritis * Sepsis * Placental abruption ### **Fetal and Neonatal** * Prematurity * Respiratory distress syndrome * Neonatal sepsis * Umbilical cord prolapse * Pulmonary hypoplasia (early PPROM) --- ## **Management of PROM** Management depends on **gestational age**, **infection status**, and **fetal condition**. --- ## **Management at Term PROM (≥ 37 Weeks)** ### **Principles** * Aim for **delivery** * Reduce infection risk ### **Management** * Induction of labor within **12–24 hours** * Oxytocin preferred * Prophylactic antibiotics if GBS positive --- ## **Management of PPROM (< 37 Weeks)** ### **General Principles** * Balance between **prematurity risks** and **infection risks** * Expectant management if stable --- ### **Stepwise Management** #### **1. Hospitalization and Monitoring** * Maternal vitals, fetal heart rate * Signs of infection #### **2. Antibiotic Therapy** **Indication**: Prolong latency, reduce infection **Standard Regimen** * Ampicillin IV → Amoxicillin oral * Erythromycin / Azithromycin **Benefits** * ↓ Chorioamnionitis * ↓ Neonatal sepsis * ↑ Latency period --- #### **3. Corticosteroids** **Indication**: 24–34 weeks **Drugs** * Betamethasone 12 mg IM × 2 doses (24 hours apart) **Benefits** * ↓ RDS * ↓ IVH * ↓ NEC --- #### **4. Tocolysis** * **Not routinely recommended** * Short-term use only to complete steroid course --- #### **5. Magnesium Sulfate** **Indication**: < 32 weeks **Purpose**: Fetal neuroprotection --- ### **Indications for Immediate Delivery** * Clinical chorioamnionitis * Non-reassuring fetal status * Placental abruption * Advanced labor * Severe oligohydramnios with distress --- ## **Prevention** * Screening and treatment of genital infections * Smoking cessation * Cervical cerclage in indicated cases * Adequate antenatal care --- ## **Prognosis** * **Term PROM**: Excellent with timely delivery * **PPROM**: Depends on gestational age and infection * Neonatal outcome improves significantly after **32–34 weeks** --- ## **Key Exam Points** * Avoid digital vaginal examination in PROM * Antibiotics increase latency in PPROM * Corticosteroids between 24–34 weeks * Infection = indication for delivery at any gestation --- ## **SEO Keywords (Comma-Separated)** premature rupture of membranes, prom pregnancy, pprom obstetrics, prom diagnosis management, preterm premature rupture membranes, prom complications, amniotic fluid leakage pregnancy, chorioamnionitis prom, prom treatment guidelines, pprom antibiotics steroids --- If you want, I can next: * Generate **SEO-optimized title and meta description** * Create **25 hard case-based MCQs (HTML CSS JS in one file)** * Generate **FAQ schema for SEO** * Provide **image prompts or medical diagrams**
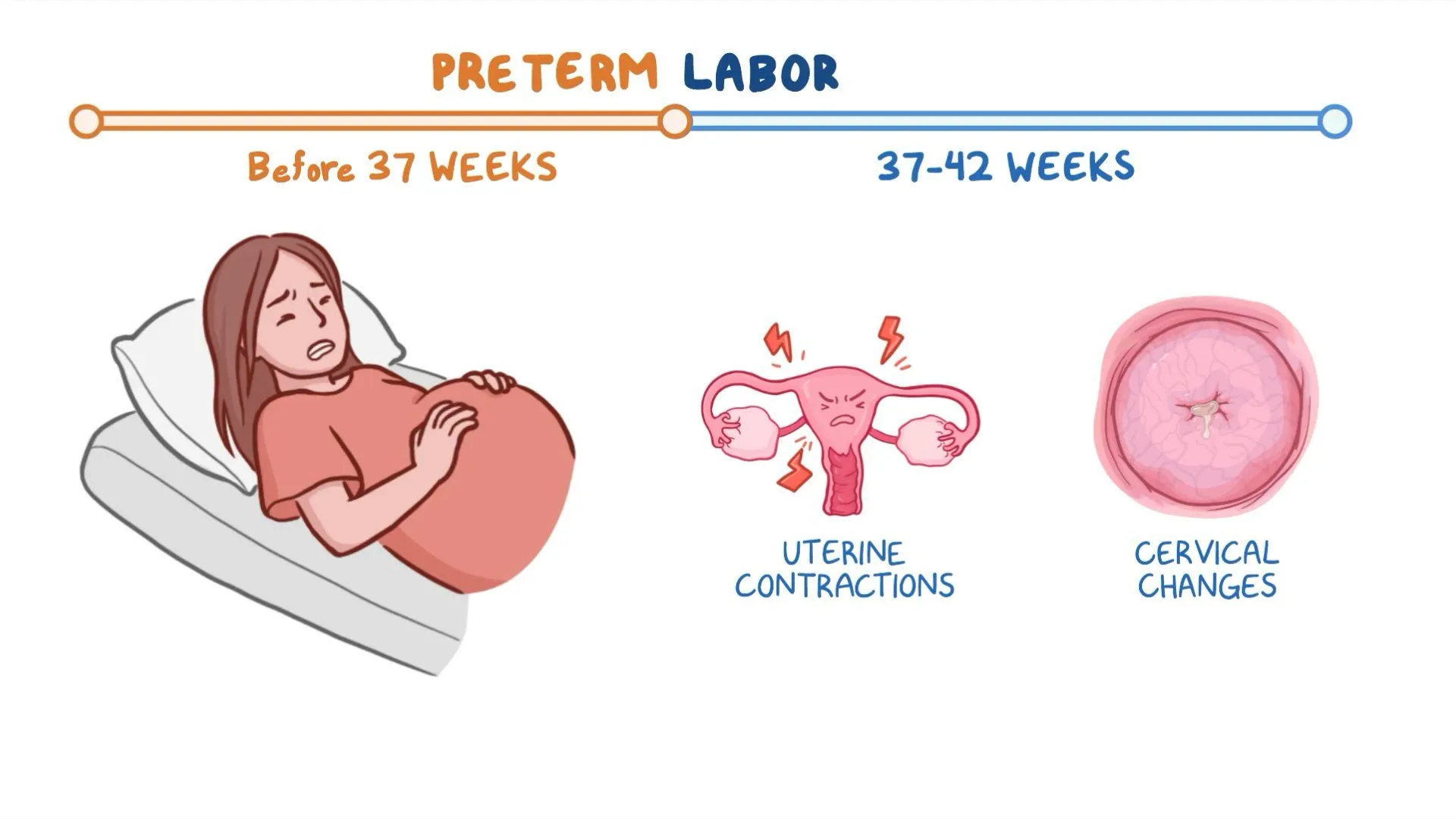
Preterm Labor: Causes, Diagnosis, Prevention and Management
Below is a **single-place, SEO-optimized, exam-ready and clinically complete reference** on **Preterm Labor**, written with clear **H1–H4 structure**, high-value keywords, and authoritative medical depth. --- # **Preterm Labor: Causes, Diagnosis, Prevention and Management** ## **Definition of Preterm Labor** Preterm labor is defined as **regular uterine contractions associated with cervical changes occurring between 20 weeks and before 37 completed weeks of gestation**, leading to preterm birth if not arrested. --- ## **Epidemiology and Importance** * Accounts for **10–12% of all pregnancies globally** * Major cause of **neonatal morbidity and mortality** * Responsible for complications such as **respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, sepsis, and long-term neurodevelopmental disability** --- ## **Pathophysiology of Preterm Labor** Preterm labor results from **premature activation of the normal labor pathway**, involving: ### **1. Uterine Activation** * Increased **oxytocin receptors** * Enhanced **prostaglandin synthesis** ### **2. Cervical Ripening** * Collagen degradation * Increased inflammatory mediators ### **3. Decidual and Membrane Activation** * Infection or inflammation leads to cytokine release * Prostaglandins stimulate uterine contractions --- ## **Etiology and Risk Factors** ### **Maternal Factors** * Previous preterm birth * Short interpregnancy interval * Extremes of maternal age * Smoking, substance abuse * Poor antenatal care * Low socioeconomic status ### **Obstetric Factors** * Multiple pregnancy * Polyhydramnios * Placental abruption * Placenta previa * Uterine anomalies ### **Infective Causes** * Urinary tract infection * Bacterial vaginosis * Chorioamnionitis ### **Fetal Factors** * Congenital anomalies * Fetal distress --- ## **Clinical Features of Preterm Labor** ### **Symptoms** * Regular uterine contractions (≥4 in 20 minutes or ≥8 in 60 minutes) * Lower abdominal or back pain * Pelvic pressure * Increased vaginal discharge * Vaginal spotting or bleeding ### **Signs** * Cervical dilation ≥1 cm * Cervical effacement ≥80% * Shortened cervical length on ultrasound --- ## **Diagnosis of Preterm Labor** ### **Clinical Assessment** * History of contractions and risk factors * Sterile speculum examination ### **Investigations** #### **1. Transvaginal Ultrasound** * Cervical length <25 mm before 24 weeks suggests high risk #### **2. Fetal Fibronectin Test** * Positive test indicates increased risk of preterm birth within 7–14 days #### **3. Laboratory Tests** * Urine analysis and culture * High vaginal swab if infection suspected * Complete blood count and CRP when indicated --- ## **Differential Diagnosis** * Braxton Hicks contractions * Urinary tract infection * Abruptio placentae * Placenta previa * Gastrointestinal causes --- ## **Management of Preterm Labor** ### **General Principles** * Confirm diagnosis * Exclude contraindications to tocolysis * Assess gestational age and fetal wellbeing --- ### **Tocolytic Therapy** Used to **delay delivery for 48 hours** to allow steroid administration. #### **1. Nifedipine (First Line)** * **Indication:** Suppression of uterine contractions * **Mechanism:** Calcium channel blockade * **Dose:** 20–30 mg orally loading, then 10–20 mg every 6–8 hours * **Adverse Effects:** Hypotension, headache, flushing * **Contraindications:** Hypotension, cardiac disease * **Monitoring:** Blood pressure, pulse * **Counselling:** Avoid sudden posture changes #### **2. Atosiban** * Oxytocin receptor antagonist * Preferred in cardiac disease #### **3. Indomethacin** * Used before 32 weeks * Risk of premature ductus arteriosus closure --- ### **Antenatal Corticosteroids** Enhance fetal lung maturity. #### **Betamethasone** * **Dose:** 12 mg IM, two doses 24 hours apart * **Benefits:** Reduces RDS, IVH, NEC, neonatal mortality * **Monitoring:** Blood glucose in diabetics --- ### **Magnesium Sulfate for Neuroprotection** * **Indication:** <32 weeks gestation * **Benefit:** Reduces cerebral palsy risk * **Adverse Effects:** Flushing, respiratory depression * **Monitoring:** Reflexes, urine output, respiratory rate --- ### **Antibiotics** * Not routinely indicated * Used when infection is confirmed or suspected --- ## **Contraindications to Tocolysis** * Intrauterine fetal demise * Lethal fetal anomalies * Severe preeclampsia or eclampsia * Chorioamnionitis * Significant vaginal bleeding --- ## **Prevention of Preterm Labor** ### **Primary Prevention** * Smoking cessation * Treatment of genital and urinary infections * Adequate antenatal care ### **Secondary Prevention** #### **Progesterone Therapy** * **Indication:** Previous preterm birth or short cervix * **Dose:** Vaginal progesterone 200 mg daily * **Mechanism:** Maintains uterine quiescence #### **Cervical Cerclage** * Indicated in cervical insufficiency * Performed between 12–14 weeks in selected cases --- ## **Complications** ### **Maternal** * Operative delivery * Infection * Postpartum hemorrhage ### **Neonatal** * Respiratory distress syndrome * Sepsis * Long-term neurodevelopmental impairment --- ## **Prognosis** * Depends on **gestational age at delivery** * Survival improves significantly after **32–34 weeks** * Early recognition and management improve outcomes --- ## **Key Clinical Pearls** * Cervical length is the **best predictor** of preterm birth * Tocolytics delay labor but **do not prevent preterm birth** * Corticosteroids are the **most effective intervention** for neonatal outcomes * Magnesium sulfate provides **neuroprotection**, not tocolysis --- ## **SEO Keywords (Comma Separated)** preterm labor, premature labor, causes of preterm labor, diagnosis of preterm labor, management of preterm labor, tocolytic therapy, antenatal corticosteroids, magnesium sulfate neuroprotection, cervical length ultrasound, fetal fibronectin test, prevention of preterm birth, progesterone therapy pregnancy --- If you want, I can **next provide**: * **25 hard case-based MCQs using HTML CSS JS (single file)** * **FAQs for SEO rich results** * **Schema-ready medical content** * **Exam-oriented summary tables** Just tell me 👍
Twin Pregnancy Complete Guide 2025 Causes Types Diagnosis Risks and Management
Below is a **complete, detailed, SEO-friendly medical article on Twin Pregnancy**, written **without images**, structured with clear **H1–H3 headings**, and optimized for **search engines and medical learning**. --- ## **SEO Title** Twin Pregnancy Complete Guide 2025 Causes Types Diagnosis Risks and Management --- ## **Meta Description** Comprehensive medical guide on twin pregnancy covering types, causes, diagnosis, antenatal care, complications, fetal surveillance, delivery planning, and prognosis for mother and babies. --- ## **SEO Keywords** twin pregnancy, multiple pregnancy twins, dichorionic twins, monochorionic twins, twin pregnancy diagnosis, twin pregnancy complications, twin pregnancy antenatal care, twin pregnancy delivery, twin pregnancy risks, twin pregnancy management, twin gestation obstetrics --- # **Twin Pregnancy** ## **1. Definition** Twin pregnancy is a type of **multiple gestation** in which **two fetuses develop simultaneously in the uterus**. It carries **higher maternal and fetal risks** compared to singleton pregnancy and requires **specialized antenatal monitoring and delivery planning**. --- ## **2. Epidemiology** * Incidence: **1 in 80–90 pregnancies** * Higher incidence with: * Assisted reproductive techniques * Advanced maternal age * Family history of twins * Multiparity --- ## **3. Classification of Twin Pregnancy** ### **3.1 Based on Zygosity** * **Dizygotic (Fraternal) Twins** * Fertilization of two separate ova * Always dichorionic and diamniotic * Most common type * **Monozygotic (Identical) Twins** * Division of a single fertilized ovum * Chorionicity depends on timing of division --- ### **3.2 Based on Chorionicity and Amnionicity** #### **3.2.1 Dichorionic Diamniotic Twins (DCDA)** * Two placentas, two amniotic sacs * Lowest complication rate * May have fused placentas #### **3.2.2 Monochorionic Diamniotic Twins (MCDA)** * One placenta, two amniotic sacs * Risk of twin-to-twin transfusion syndrome #### **3.2.3 Monochorionic Monoamniotic Twins (MCMA)** * One placenta, one amniotic sac * Highest risk * Cord entanglement common --- ## **4. Etiology and Risk Factors** * Assisted reproductive technology * Ovulation induction * Maternal age above 30 years * African ethnicity * Tall stature and high BMI * Family history of twins --- ## **5. Diagnosis of Twin Pregnancy** ### **5.1 Clinical Features** * Excessive uterine enlargement * Severe nausea and vomiting * Early perception of fetal movements * Palpation of multiple fetal parts ### **5.2 Ultrasonography** * Gold standard for diagnosis * Confirms: * Number of fetuses * Chorionicity and amnionicity * Gestational age * Placental location ### **5.3 Doppler Studies** * Used for fetal surveillance * Essential in monochorionic twins --- ## **6. Antenatal Care in Twin Pregnancy** ### **6.1 General Principles** * More frequent antenatal visits * Early booking * Multidisciplinary approach ### **6.2 Nutritional Requirements** * Increased calorie intake * Iron supplementation * Folic acid * Calcium and protein supplementation ### **6.3 Fetal Surveillance** * Serial growth scans every 2–4 weeks * Amniotic fluid assessment * Doppler velocimetry --- ## **7. Maternal Complications** * Anemia * Gestational hypertension * Preeclampsia * Gestational diabetes * Antepartum hemorrhage * Polyhydramnios * Increased operative delivery * Postpartum hemorrhage --- ## **8. Fetal Complications** * Preterm birth * Low birth weight * Intrauterine growth restriction * Congenital anomalies * Twin-to-twin transfusion syndrome * Cord accidents * Perinatal mortality --- ## **9. Special Complications in Monochorionic Twins** ### **9.1 Twin-to-Twin Transfusion Syndrome** * Unequal placental blood flow * Donor twin: growth restriction, oligohydramnios * Recipient twin: polyhydramnios, cardiac overload ### **9.2 Twin Anemia Polycythemia Sequence** * Chronic intertwin blood transfusion * Diagnosed by Doppler MCA PSV --- ## **10. Management of Twin Pregnancy** ### **10.1 Antenatal Management** * Strict blood pressure monitoring * Early detection of complications * Corticosteroids for lung maturity if preterm risk ### **10.2 Timing of Delivery** * DCDA twins: 37–38 weeks * MCDA twins: 36–37 weeks * MCMA twins: 32–34 weeks by planned cesarean ### **10.3 Mode of Delivery** * Vaginal delivery if: * First twin cephalic * No obstetric contraindications * Cesarean section if: * First twin non-cephalic * Monoamniotic twins * Obstetric complications --- ## **11. Intrapartum Care** * Continuous fetal monitoring * Availability of neonatal intensive care * Skilled obstetric and anesthetic support --- ## **12. Postpartum Care** * Active management of third stage * Monitoring for postpartum hemorrhage * Lactation support * Neonatal care for prematurity --- ## **13. Prognosis** * Improved outcomes with early diagnosis * Chorionicity is the strongest predictor * Higher neonatal morbidity compared to singleton pregnancy --- ## **14. Key Clinical Pearls** * Early determination of chorionicity is critical * Monochorionic twins require closer surveillance * Preterm birth is the most common complication * Delivery planning should be individualized --- If you want, I can next provide: **25 hard case-based MCQs (HTML CSS JS single file)**, **FAQs for SEO**, or **exam-oriented short notes** for twin pregnancy.

Placenta Accreta Spectrum: Definition, Risk Factors, Diagnosis and Management
Below is a **fully SEO-optimized, image-free, exam-ready and clinically complete** article on **Placenta Accreta Spectrum**, structured exactly in the **H1 → H2 → H3** format that search engines and medical readers prefer. --- ## **SEO Title** **Placenta Accreta Spectrum: Definition, Risk Factors, Diagnosis and Management** --- ## **SEO Meta Description** Comprehensive clinical guide on Placenta Accreta Spectrum covering definition, types, pathophysiology, risk factors, diagnosis, imaging criteria, antenatal planning, surgical management, complications, and maternal outcomes. --- ## **SEO Keywords** placenta accreta spectrum, placenta accreta, placenta increta, placenta percreta, morbidly adherent placenta, placenta accreta diagnosis, placenta accreta ultrasound signs, placenta accreta MRI, placenta accreta management, cesarean hysterectomy accreta, postpartum hemorrhage accreta --- # **Placenta Accreta Spectrum** ## **1. Definition** Placenta Accreta Spectrum (PAS) refers to a group of abnormal placental attachment disorders characterized by **pathological adherence of the placenta to the myometrium due to partial or complete absence of decidua basalis**, resulting in failure of normal placental separation after delivery. --- ## **2. Classification of Placenta Accreta Spectrum** ### **2.1 Placenta Accreta** * Chorionic villi attach **directly to the myometrium** * Most common and least severe form ### **2.2 Placenta Increta** * Chorionic villi **invade into the myometrium** ### **2.3 Placenta Percreta** * Chorionic villi **penetrate through the myometrium and serosa** * May invade adjacent organs (bladder most commonly) --- ## **3. Epidemiology** * Incidence: ~1 in 300–500 pregnancies * Rapidly increasing due to rising cesarean section rates * Major cause of **severe obstetric hemorrhage and maternal morbidity** --- ## **4. Etiopathogenesis and Pathophysiology** ### **4.1 Underlying Mechanism** * Defective or absent decidua basalis * Inadequate Nitabuch’s layer * Direct trophoblastic invasion into myometrium ### **4.2 Contributing Factors** * Prior uterine surgery leads to **endometrial scarring** * Implantation over scar tissue promotes abnormal placental adherence --- ## **5. Risk Factors** ### **5.1 Major Risk Factors** * Previous cesarean delivery (risk increases with number) * Placenta previa with prior cesarean section ### **5.2 Additional Risk Factors** * Previous myomectomy * Dilatation and curettage * Asherman syndrome * Advanced maternal age * Multiparity * Assisted reproductive techniques --- ## **6. Clinical Features** ### **6.1 Antenatal Period** * Often asymptomatic * Frequently associated with placenta previa * May present with painless antepartum bleeding ### **6.2 Intrapartum and Postpartum** * Failure of placental separation * Massive postpartum hemorrhage * Hypovolemic shock * Disseminated intravascular coagulation --- ## **7. Diagnosis** ### **7.1 Antenatal Diagnosis** Early diagnosis is critical for reducing morbidity. #### **Ultrasound (First Line)** Key grayscale and Doppler findings: * Loss of retroplacental clear zone * Thinning of myometrium (<1 mm) * Placental lacunae (“Swiss cheese” appearance) * Turbulent lacunar blood flow * Bridging vessels to bladder #### **MRI (Adjunct Tool)** Indications: * Posterior placenta * Suspected placenta percreta * Inconclusive ultrasound MRI Findings: * Dark intraplacental bands on T2 * Myometrial thinning * Uterine bulging * Direct invasion of adjacent organs --- ## **8. Differential Diagnosis** * Retained placenta * Uterine atony * Placenta previa without invasion * Uterine inversion --- ## **9. Antenatal Management and Planning** ### **9.1 Multidisciplinary Approach** * Obstetrician * Anesthesiologist * Interventional radiologist * Urologist * Blood bank support ### **9.2 Timing of Delivery** * Planned delivery at **34–36 weeks** * After corticosteroids for fetal lung maturity ### **9.3 Place of Delivery** * Tertiary care center with massive transfusion capability --- ## **10. Intrapartum Management** ### **10.1 Preferred Surgical Approach** * **Planned cesarean hysterectomy without attempting placental removal** * Placenta left in situ to prevent catastrophic hemorrhage ### **10.2 Surgical Principles** * Vertical uterine incision away from placenta * Avoid placental manipulation * Early hysterectomy following fetal delivery --- ## **11. Conservative Management Options** Reserved for highly selected cases desiring fertility. ### **11.1 Methods** * Placenta left in situ * Uterine artery embolization * Methotrexate use (controversial) ### **11.2 Risks** * Severe infection * Delayed hemorrhage * Secondary hysterectomy --- ## **12. Complications** ### **12.1 Maternal Complications** * Massive hemorrhage * Blood transfusion reactions * Bladder or ureteric injury * Sepsis * Thromboembolism * Maternal mortality ### **12.2 Fetal Complications** * Prematurity * Low birth weight * NICU admission --- ## **13. Prognosis** * Prognosis improves significantly with **antenatal diagnosis** * Planned surgery reduces maternal mortality * Future fertility usually lost with definitive surgery --- ## **14. Prevention** * Rational use of cesarean sections * Avoid unnecessary uterine curettage * Early risk stratification in placenta previa cases --- ## **15. Key Exam and Clinical Pearls** * Placenta previa with previous cesarean = **PAS until proven otherwise** * Never attempt manual placental removal if accreta suspected * Cesarean hysterectomy is the gold standard management * MRI complements ultrasound, not a replacement --- If you want, I can next provide: * **Case-based MCQs (HTML CSS JS single file)** * **PAS vs Placenta Previa comparison table** * **FAQ section for SEO** * **Schema-ready JSON-LD medical article** Just tell me 👍

Antepartum Hemorrhage (APH): Causes, Symptoms, Diagnosis, Management & Complications
--- # **Antepartum Hemorrhage (APH): Causes, Symptoms, Diagnosis, Management and Complications** --- ## **What Is Antepartum Hemorrhage?** ### **Definition of Antepartum Hemorrhage** Antepartum hemorrhage (APH) is defined as **bleeding from or into the genital tract occurring after 20 weeks of gestation and before the delivery of the fetus**. ### **Meaning of APH in Pregnancy** APH is a **major obstetric emergency** associated with significant **maternal morbidity, fetal hypoxia, preterm birth, and perinatal mortality**. --- ## **Epidemiology of Antepartum Hemorrhage** ### **Incidence of APH** * Occurs in **3–5% of all pregnancies** * Accounts for a large proportion of **emergency obstetric admissions** ### **Maternal and Perinatal Impact** * Major cause of: * Maternal anemia * Hemorrhagic shock * Stillbirth * Neonatal intensive care admission --- ## **Classification of Antepartum Hemorrhage** ### **Placental Causes of Antepartum Hemorrhage** Placental causes account for **approximately 70% of APH cases**. #### **Placenta Previa** Placenta implanted in the **lower uterine segment**, partially or completely covering the internal cervical os. #### **Placental Abruption (Abruptio Placentae)** Premature separation of a **normally situated placenta** after 20 weeks of gestation. #### **Vasa Previa** Fetal blood vessels traverse the membranes over the cervical os, unprotected by placenta or Wharton’s jelly. --- ### **Non-Placental Causes of Antepartum Hemorrhage** #### **Cervical Causes** * Cervical ectropion * Cervicitis * Cervical polyps * Cervical carcinoma #### **Vaginal Causes** * Trauma * Infection * Varicosities --- ### **Unexplained Antepartum Hemorrhage** * No identifiable cause * Occurs in **10–15%** of cases * Still associated with adverse fetal outcomes --- ## **Risk Factors for Antepartum Hemorrhage** ### **Risk Factors for Placenta Previa** * Previous cesarean section * Previous placenta previa * Multiparity * Advanced maternal age * Smoking ### **Risk Factors for Placental Abruption** * Hypertension and preeclampsia * Abdominal trauma * Smoking and cocaine use * Polyhydramnios * Sudden uterine decompression --- ## **Pathophysiology of Antepartum Hemorrhage** ### **Pathophysiology of Placenta Previa** * Placenta in lower uterine segment * Stretching and thinning cause **placental separation** * Results in **painless bleeding** ### **Pathophysiology of Placental Abruption** * Rupture of maternal vessels in decidua basalis * Formation of retroplacental hematoma * Leads to **uterine hypertonicity and fetal hypoxia** ### **Pathophysiology of Vasa Previa** * Rupture of fetal vessels * Rapid fetal blood loss * Can cause **acute fetal demise** --- ## **Clinical Features of Antepartum Hemorrhage** ### **General Symptoms of APH** * Vaginal bleeding * Reduced fetal movements * Abdominal pain (may or may not be present) --- ### **Clinical Features of Placenta Previa** * **Painless**, bright red bleeding * Recurrent episodes * Soft, non-tender uterus * Malpresentation common * Fetal heart sounds usually normal --- ### **Clinical Features of Placental Abruption** * **Painful bleeding** * Dark blood * Tense, tender uterus * Maternal shock may be disproportionate * Fetal distress or absent heart sounds --- ### **Clinical Features of Vasa Previa** * Sudden bleeding after rupture of membranes * Fetal bradycardia * Maternal condition relatively stable --- ## **Initial Assessment of Antepartum Hemorrhage** ### **Primary Survey (ABC Approach)** * Airway, Breathing, Circulation * Oxygen supplementation * Two large-bore IV cannulae * Monitor vitals and urine output ### **Important Clinical Rule** ⚠️ **Digital vaginal examination is contraindicated until placenta previa is excluded** --- ## **Investigations in Antepartum Hemorrhage** ### **Laboratory Investigations** * Complete blood count * Blood group and Rh typing * Cross-match blood * Coagulation profile (especially in abruption) * Renal function tests --- ### **Imaging in Antepartum Hemorrhage** * **Ultrasound** for placental localization * Doppler ultrasound for suspected vasa previa * Continuous CTG for fetal monitoring --- ## **Differential Diagnosis of Antepartum Hemorrhage** * Placenta previa * Placental abruption * Vasa previa * Preterm labor with show * Cervical malignancy * Uterine rupture (rare) --- ## **Management of Antepartum Hemorrhage** ### **General Management Principles** * Hospital admission * Bed rest * IV fluids * Blood transfusion if required * Anti-D immunoglobulin for Rh-negative mothers * Corticosteroids if gestation <34 weeks --- ## **Management of Placenta Previa** ### **Expectant Management** Indicated when: * Bleeding is mild * Gestation is preterm * Mother and fetus stable Includes: * Close monitoring * Avoid vaginal exams * Steroids for fetal lung maturity --- ### **Definitive Management** * **Cesarean section** is the mode of delivery for: * Major placenta previa * Heavy or recurrent bleeding * Fetal distress * Term pregnancy --- ## **Management of Placental Abruption** ### **Mild Abruption** * Conservative management * Close maternal and fetal monitoring ### **Severe Abruption** * Immediate delivery * Blood products * Correction of coagulopathy ### **Mode of Delivery** * Vaginal if fetus dead and labor progressing * Cesarean if fetus alive with distress --- ## **Management of Vasa Previa** * Emergency cesarean section * Neonatal resuscitation readiness * Planned elective cesarean if diagnosed antenatally --- ## **Complications of Antepartum Hemorrhage** ### **Maternal Complications** * Hemorrhagic shock * Disseminated intravascular coagulation (DIC) * Postpartum hemorrhage * Acute kidney injury * Maternal death --- ### **Fetal Complications** * Prematurity * Intrauterine growth restriction * Fetal hypoxia * Stillbirth * Neonatal anemia --- ## **Prevention of Antepartum Hemorrhage** ### **Preventive Strategies** * Routine antenatal ultrasound * Control of hypertension * Avoid smoking and substance abuse * Planned delivery in high-risk pregnancies --- ## **Prognosis of Antepartum Hemorrhage** ### **Maternal Prognosis** * Good with early diagnosis and prompt management ### **Fetal Prognosis** * Depends on: * Cause of APH * Gestational age * Speed of intervention --- ## **Exam-Oriented Key Points** * **Painless bleeding → Placenta previa** * **Painful bleeding + tender uterus → Abruption** * **Shock out of proportion → Concealed abruption** * **Never perform PV exam before ruling out placenta previa** --- ## **Frequently Asked Questions (SEO Boost)** ### **Is antepartum hemorrhage dangerous?** Yes. APH is a **medical emergency** that can threaten both maternal and fetal life. ### **What is the most common cause of APH?** **Placenta previa** is the most common cause. ### **Can APH be prevented?** Some causes can be reduced with proper antenatal care and risk factor control. ---
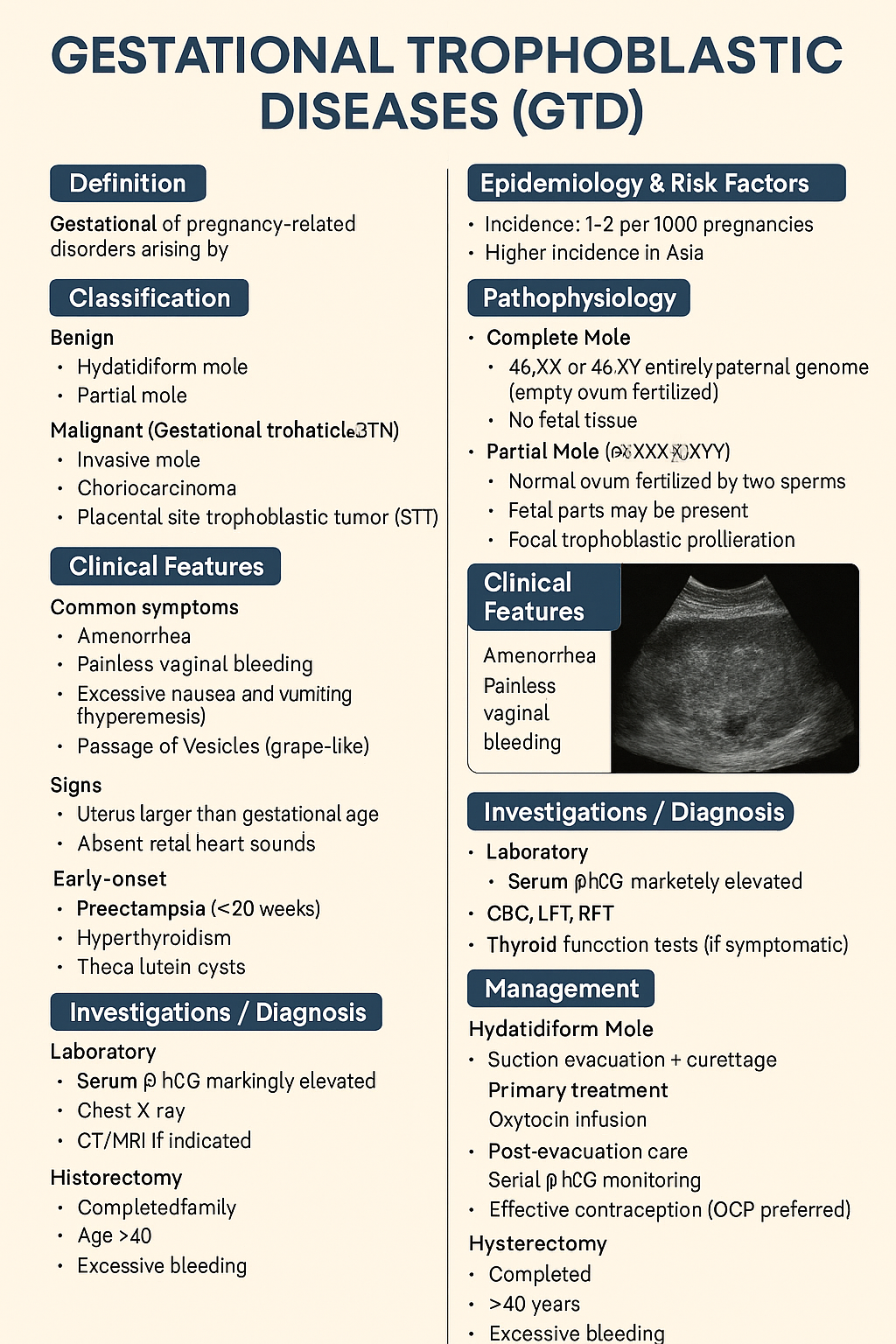
Gestational Trophoblastic Diseases (GTD): Types, Diagnosis, Management & Prognosis – Complete Medical Guide 2025
Below is a **single-place, exam-ready, clinically complete reference** on **Gestational Trophoblastic Diseases (GTD)**, structured exactly for **medical learning, exams, and clinical use**. --- # **Gestational Trophoblastic Diseases (GTD)** ## **1. Definition** Gestational trophoblastic diseases are a **spectrum of pregnancy-related disorders** arising from **abnormal proliferation of trophoblastic tissue** following conception. They range from **benign molar pregnancy** to **malignant gestational trophoblastic neoplasia (GTN)**. --- ## **2. Classification** ### **A. Benign** 1. **Hydatidiform mole** * Complete mole * Partial mole ### **B. Malignant (Gestational Trophoblastic Neoplasia – GTN)** 1. **Invasive mole** 2. **Choriocarcinoma** 3. **Placental site trophoblastic tumor (PSTT)** 4. **Epithelioid trophoblastic tumor (ETT)** --- ## **3. Epidemiology & Risk Factors** * Incidence: **1–2 per 1000 pregnancies** * Higher incidence in **Asia** * Risk factors: * Extremes of maternal age (<20, >35 years) * Previous molar pregnancy * Nutritional deficiency (low carotene, folate) * History of miscarriage --- ## **4. Pathophysiology** ### **Complete Mole** * **46,XX or 46,XY** * Entirely paternal genome (empty ovum fertilized) * No fetal tissue * Diffuse trophoblastic hyperplasia ### **Partial Mole** * **Triploid (69,XXX/XXY/XYY)** * Normal ovum fertilized by two sperms * Fetal parts may be present * Focal trophoblastic proliferation --- ## **5. Clinical Features** ### **Common Symptoms** * Amenorrhea * **Painless vaginal bleeding** * Excessive nausea and vomiting (hyperemesis) * Passage of vesicles (grape-like) ### **Signs** * Uterus larger than gestational age (complete mole) * Absent fetal heart sounds * Early-onset: * Preeclampsia (<20 weeks) * Hyperthyroidism * Theca lutein cysts --- ## **6. Investigations / Diagnosis** ### **Laboratory** * **Serum β-hCG**: markedly elevated * CBC, LFT, RFT * Thyroid function tests (if symptomatic) ### **Imaging** * **Ultrasound** * Complete mole: *“Snowstorm / cluster of grapes”* * Partial mole: gestational sac + abnormal fetus ### **Histopathology** * Confirms diagnosis after evacuation ### **Baseline Metastatic Work-up (GTN)** * Chest X-ray * CT/MRI if indicated --- ## **7. Differential Diagnosis** * Missed abortion * Ectopic pregnancy * Placenta accreta * Degenerating fibroid --- ## **8. Management** ### **A. Hydatidiform Mole** #### **Primary Treatment** * **Suction evacuation + curettage** (treatment of choice) * Oxytocin infusion after evacuation #### **Post-Evacuation Care** * Serial β-hCG monitoring * Effective contraception (OCP preferred) #### **Hysterectomy** * Completed family * Age >40 years * Excessive bleeding --- ### **B. Gestational Trophoblastic Neoplasia (GTN)** #### **Diagnosis of GTN (FIGO criteria)** * Plateauing β-hCG * Rising β-hCG * Persistent β-hCG >6 months * Histologic choriocarcinoma #### **Risk Stratification (WHO Score)** * Low risk: ≤6 * High risk: ≥7 --- ## **9. Chemotherapy** ### **Low-Risk GTN** #### **Methotrexate** * **Mechanism**: Folate antagonist → inhibits DNA synthesis * **Dose**: * 50 mg IM weekly OR * 1 mg/kg on days 1,3,5,7 + folinic acid * **Adverse effects**: * Stomatitis * Hepatotoxicity * Bone marrow suppression * **Monitoring**: * CBC * LFTs * β-hCG weekly * **Contraindications**: * Liver disease * Renal failure #### **Actinomycin-D (Alternative)** * **Mechanism**: DNA intercalation * **Dose**: 1.25 mg/m² IV every 2 weeks * **Adverse effects**: * Alopecia * Myelosuppression --- ### **High-Risk GTN** #### **EMA-CO Regimen** * **Etoposide** * **Methotrexate** * **Actinomycin-D** * **Cyclophosphamide** * **Vincristine** **Indication**: WHO score ≥7 or metastatic disease --- ## **10. Special Types** ### **Choriocarcinoma** * Highly malignant * Early hematogenous spread (lungs, brain) * Very high β-hCG * Responds excellently to chemotherapy ### **PSTT & ETT** * Low β-hCG * Less chemosensitive * **Primary treatment: hysterectomy** --- ## **11. Follow-Up** * β-hCG: * Weekly until negative ×3 * Monthly for 6–12 months * Contraception mandatory during follow-up * Next pregnancy allowed after surveillance completion --- ## **12. Prognosis** * Cure rate: * **>98% in low-risk GTN** * **>85–90% in high-risk GTN** * Future fertility usually preserved --- ## **13. Key Exam Pearls** * Early preeclampsia → think **molar pregnancy** * β-hCG is the **tumor marker** * Choriocarcinoma follows **any pregnancy** * PSTT → **hysterectomy**, not chemo * OCPs are **safe** during follow-up --- If you want next: * **SEO title + keywords** * **25 hard case-based MCQs (HTML/CSS/JS – single file)** * **Flowcharts / tables only** * **Separate GTN chemotherapy comparison** * **Image-free exam revision notes** Just tell me what you want next.
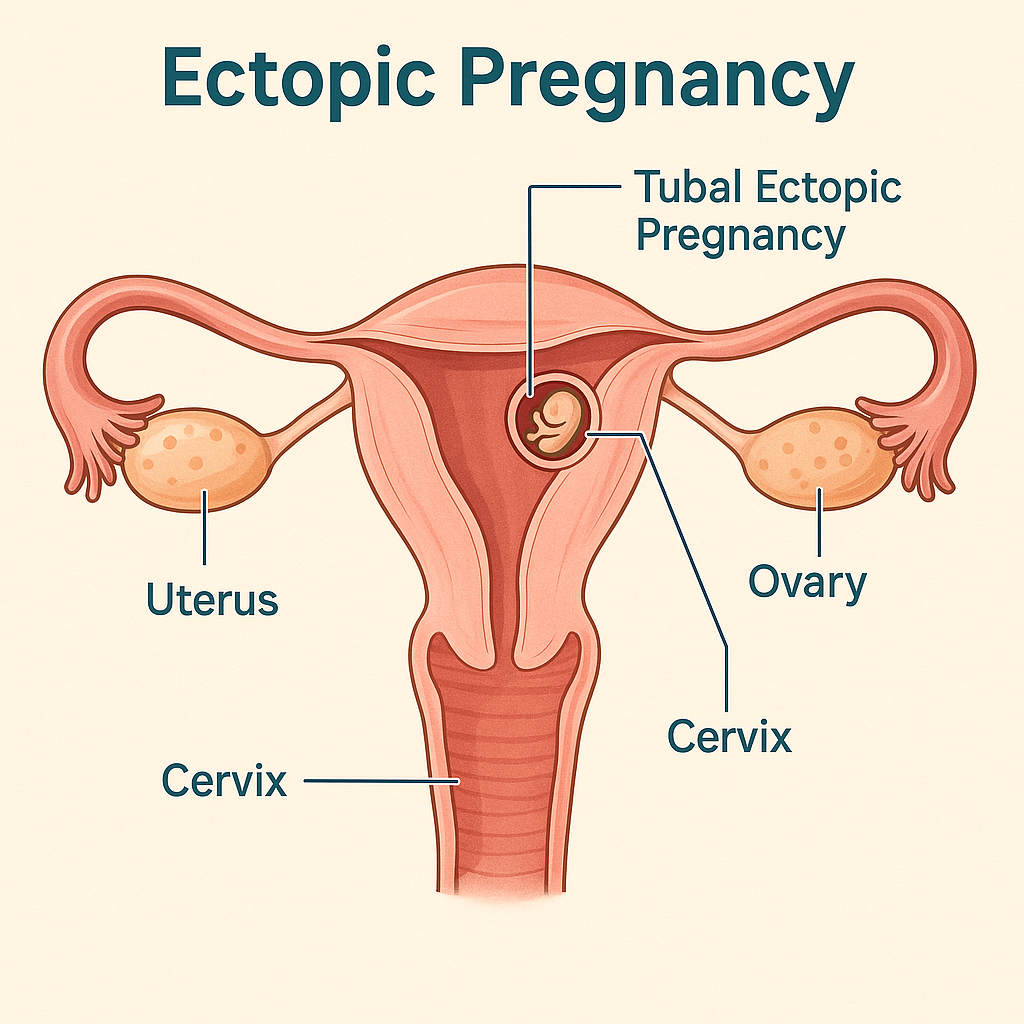
Ectopic Pregnancy: Causes, Symptoms, Diagnosis, Treatment Options & Management Guidelines (2025 Complete Guide)
Below is a **single-place, exam-ready + clinical-practice detailed reference** on **Ectopic Pregnancy**, written in the **structured pattern you prefer** and suitable for your medical hub. ✔️ **No images included** ✔️ **Includes authoritative external links** --- # **Ectopic Pregnancy – Complete Clinical & Management Guide (2025)** --- ## **1. Definition** **Ectopic pregnancy** is implantation of a fertilized ovum **outside the endometrial cavity**. > > 95% occur in the **fallopian tube**. It is a **life-threatening obstetric emergency** if ruptured. --- ## **2. Epidemiology** * Incidence: **1–2% of all pregnancies** * Leading cause of **maternal mortality in first trimester** * Rising incidence due to: * Assisted reproductive techniques (ART) * Pelvic inflammatory disease (PID) --- ## **3. Common Sites of Ectopic Pregnancy** | Site | Approx. % | | ---------------------- | ---------- | | Ampullary tube | 70% | | Isthmic tube | 12% | | Fimbrial | 11% | | Interstitial (cornual) | 2–4% | | Ovarian | <1% | | Cervical | <1% | | Caesarean scar | Increasing | --- ## **4. Pathophysiology** Normal embryo transport is impaired due to: * **Tubal damage** * **Altered tubal motility** * **Delayed ovum transport** → Implantation occurs before reaching uterus → Trophoblastic invasion erodes vessels → **Tubal rupture → hemorrhage** --- ## **5. Risk Factors** ### High-risk * Previous ectopic pregnancy * Tubal surgery / sterilization * PID (especially *Chlamydia*) * Assisted reproduction (IVF) ### Moderate risk * IUCD in situ * Smoking * Endometriosis ### No identifiable risk factor in ~50% --- ## **6. Clinical Features** ### Classical Triad (only ~50%) 1. **Amenorrhea** 2. **Lower abdominal pain** 3. **Vaginal bleeding** ### Other symptoms * Shoulder tip pain (diaphragmatic irritation) * Syncope * Dizziness ### Signs of Rupture * Hypotension * Tachycardia * Pallor * Abdominal guarding * Cervical motion tenderness * Full, tender pouch of Douglas --- ## **7. Investigations / Diagnosis** ### 1. Urine Pregnancy Test * Positive ### 2. Serum β-hCG (Quantitative) * **Discriminatory zone**: ~1500–2000 IU/L * If no intrauterine gestational sac → suspect ectopic * Plateauing or suboptimal rise (<66% in 48 hrs) ### 3. Transvaginal Ultrasound (TVS) **Suggestive findings** * Empty uterus * Adnexal mass * Tubal ring sign * Free fluid in pelvis ### 4. Culdocentesis (obsolete) ### 5. Diagnostic Laparoscopy (gold standard if uncertain) --- ## **8. Differential Diagnosis** * Threatened / incomplete abortion * Corpus luteum cyst * Acute PID * Ovarian torsion * Appendicitis * Renal colic --- ## **9. Management (Stepwise)** ### A. Expectant Management **Criteria** * Asymptomatic * β-hCG <200 IU/L and declining * No adnexal mass * Reliable follow-up --- ### B. Medical Management – **Methotrexate** #### Indications * Hemodynamically stable * Unruptured ectopic * β-hCG ≤5000 IU/L * No fetal cardiac activity #### Contraindications * Hemodynamic instability * Liver, renal disease * Breastfeeding * Blood dyscrasias #### Regimens **Single-dose** * Methotrexate **50 mg/m² IM** * Check β-hCG on day 4 & 7 **Multi-dose** * MTX 1 mg/kg on days 1,3,5,7 * Leucovorin rescue --- ### C. Surgical Management #### Indications * Ruptured ectopic * Hemodynamic instability * Failed medical treatment * Contraindications to methotrexate #### Procedures * **Salpingectomy** (preferred if tube severely damaged) * **Salpingostomy** (fertility preservation) * Laparoscopy preferred over laparotomy (if stable) --- ## **10. Special Types** ### Interstitial (Cornual) * Late rupture * Massive hemorrhage * Managed surgically ± MTX ### Cervical Ectopic * Painless bleeding * Managed with MTX, uterine artery embolization ### Caesarean Scar Pregnancy * Increasing incidence * High risk of placenta accreta * Early MTX or surgical excision --- ## **11. Complications** * Hemorrhagic shock * Infertility * Recurrent ectopic pregnancy * Maternal death (if delayed) --- ## **12. Prognosis** * Future fertility preserved in many * Recurrence risk: **10–25%** * Early diagnosis improves outcomes --- ## **13. Counselling & Follow-Up** * Avoid pregnancy for **3 months after MTX** * Early ultrasound in next pregnancy * Discuss recurrence risk * Rh-negative women → **Anti-D immunoglobulin** --- ## **14. Prevention** * Prompt treatment of PID * Smoking cessation * Safe reproductive practices * Early antenatal booking --- ## **15. Authoritative External Links** * **WHO – Ectopic Pregnancy Overview** [https://www.who.int](https://www.who.int) * **ACOG Practice Bulletin: Tubal Ectopic Pregnancy** [https://www.acog.org](https://www.acog.org) * **RCOG Green-top Guideline No. 21** [https://www.rcog.org.uk](https://www.rcog.org.uk) * **UpToDate – Ectopic Pregnancy (Clinician Reference)** [https://www.uptodate.com](https://www.uptodate.com) * **NICE Guideline: Ectopic pregnancy and miscarriage** [https://www.nice.org.uk](https://www.nice.org.uk) --- If you want, I can next: * Create **SEO title, meta description & keywords** * Convert this into **HTML (single-file)** for your site * Generate **case-based MCQs** * Add **internal links** to abortion, PID, β-hCG interpretation, or early pregnancy bleeding Just tell me 👍
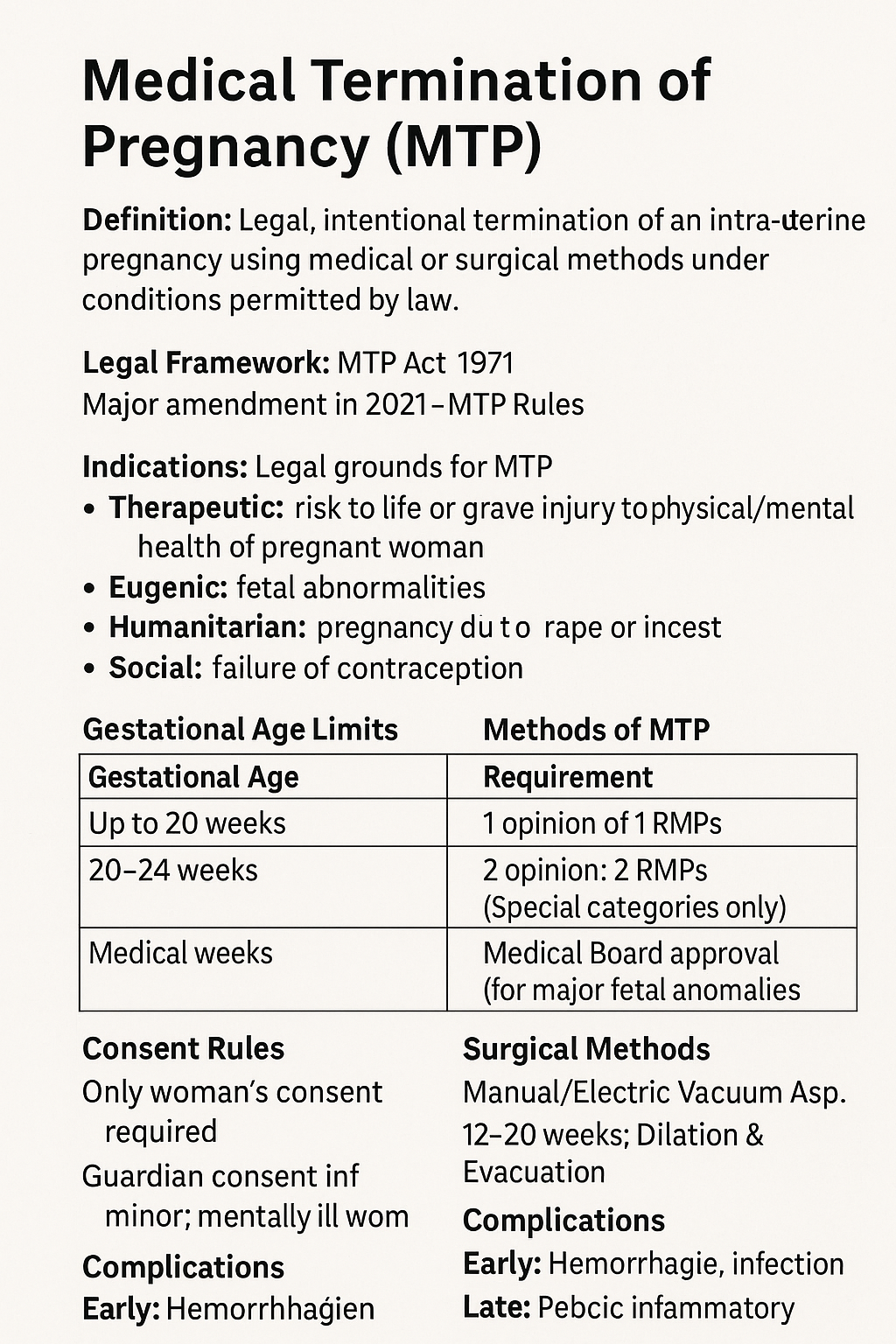
Medical Termination of Pregnancy (MTP): MTP Act, Indications, Methods, Gestational Limits & Complete Guide 2025
Below is a **complete, exam-ready, clinically exhaustive detail note on MTP (Medical Termination of Pregnancy)** with **reliable external reference links**. *(Text only, no images — as you prefer.)* --- # **Medical Termination of Pregnancy (MTP): Complete Detailed Note (India-Focused, 2025)** --- ## **1. Definition** **Medical Termination of Pregnancy (MTP)** is the **legal, intentional termination of an intra-uterine pregnancy** using **medical or surgical methods**, performed **under conditions permitted by law** to safeguard the woman’s physical, mental, and social well-being. --- ## **2. Legal Framework in India** ### **MTP Act** * **MTP Act, 1971** * **Amended in 2002** * **Major Amendment in 2021** * **MTP Rules & Regulations, 2003 & 2021** ### **Key Objectives** * Reduce **unsafe abortions** * Protect **reproductive rights** * Reduce **maternal mortality** --- ## **3. Indications for MTP (Legal Grounds)** ### **A. Therapeutic** * Risk to **life of the pregnant woman** * Grave injury to **physical or mental health** ### **B. Eugenic** * Substantial risk of **serious fetal abnormalities** * Includes **lethal anomalies, chromosomal disorders** ### **C. Humanitarian** * Pregnancy due to **rape or incest** ### **D. Social** * **Failure of contraception** (Applicable to **married & unmarried women** after 2021 amendment) --- ## **4. Gestational Age Limits & Medical Opinion** | Gestational Age | Requirement | | --------------- | ------------------------------------------------------ | | **≤ 20 weeks** | Opinion of **1 Registered Medical Practitioner (RMP)** | | **20–24 weeks** | Opinion of **2 RMPs** (Special categories only) | | **> 24 weeks** | **Medical Board approval** (for major fetal anomalies) | ### **Special Categories (20–24 weeks)** * Survivors of rape/incest * Minors * Differently-abled women * Mentally ill women * Disaster/emergency situations --- ## **5. Who Can Perform MTP?** Only a **Registered Medical Practitioner (RMP)** with: * Recognized qualification * Training in **obstetrics & gynecology** * Performed at **approved facilities only** --- ## **6. Approved Places for MTP** * Government hospitals * Approved private hospitals/clinics * Facilities meeting **MTP Rules infrastructure criteria** --- ## **7. Methods of MTP** --- ### **A. Medical Abortion** **Used up to 9 weeks (63 days)** #### **Drugs & Regimen** 1. **Mifepristone 200 mg orally** 2. After 24–48 hrs → **Misoprostol 800 mcg** * Oral / Buccal / Vaginal #### **Mechanism** * Mifepristone: Progesterone antagonist → decidual breakdown * Misoprostol: Prostaglandin → uterine contractions #### **Contraindications** * Ectopic pregnancy * Chronic adrenal failure * Long-term steroid therapy * Bleeding disorders --- ### **B. Surgical Methods** #### **Up to 12 weeks** * **Manual Vacuum Aspiration (MVA)** * **Electric Vacuum Aspiration (EVA)** #### **12–20 weeks** * **Dilation & Evacuation (D&E)** #### **>20 weeks (selected cases)** * Medical induction using **misoprostol ± mifepristone** * Rarely hysterotomy --- ## **8. Pre-Procedure Evaluation** * Confirm **intrauterine pregnancy** * Gestational age (USG) * Hb, blood group & Rh * Rule out **ectopic pregnancy** * Informed **written consent** * **Guardian consent** for minors/mentally ill women --- ## **9. Consent Rules** * **Only woman’s consent required** * **Husband’s consent NOT required** * Guardian consent mandatory for: * Minor (<18 years) * Mentally ill woman --- ## **10. Confidentiality** * Identity of woman **must not be disclosed** * Breach punishable under law --- ## **11. Post-Abortion Care** * Monitor bleeding, infection * **Anti-D immunoglobulin** for Rh-negative women * Pain management * Antibiotics if indicated * **Contraceptive counselling before discharge** --- ## **12. Complications of MTP** ### **Early** * Hemorrhage * Infection * Incomplete abortion * Uterine perforation (surgical) ### **Late** * Pelvic inflammatory disease * Asherman syndrome (rare) * Psychological distress --- ## **13. Failure of MTP** * Ongoing pregnancy * Incomplete evacuation * Requires repeat evacuation or surgery --- ## **14. MTP vs Illegal Abortion** | Legal MTP | Unsafe Abortion | | -------------- | ----------------------- | | Done by RMP | Untrained person | | Approved place | Unsafe location | | Sterile | Septic | | Low mortality | High maternal mortality | --- ## **15. Ethical & Social Aspects** * Women’s **reproductive autonomy** * Balancing fetal rights & maternal health * Public health importance --- ## **16. Important Exam & Clinical Pearls** * MTP **≠ abortion on demand** * 2021 Act includes **unmarried women** * Husband consent **not required** * Medical Board mandatory **>24 weeks** --- ## **17. Reliable External Reference Links** * **Ministry of Health & Family Welfare (India)** [https://www.mohfw.gov.in](https://www.mohfw.gov.in) * **MTP Act 1971 (Bare Act)** [https://legislative.gov.in/actsofparliamentfromtheyear/medical-termination-pregnancy-act-1971](https://legislative.gov.in/actsofparliamentfromtheyear/medical-termination-pregnancy-act-1971) * **MTP Amendment Act 2021** [https://prsindia.org/billtrack/medical-termination-of-pregnancy-amendment-bill-2020](https://prsindia.org/billtrack/medical-termination-of-pregnancy-amendment-bill-2020) * **WHO – Abortion Care Guideline** [https://www.who.int/publications/i/item/9789240039483](https://www.who.int/publications/i/item/9789240039483) * **ACOG – Induced Abortion** [https://www.acog.org/clinical/clinical-guidance/practice-bulletin](https://www.acog.org/clinical/clinical-guidance/practice-bulletin) * **FIGO Safe Abortion Guidelines** [https://www.figo.org/resources/safe-abortion](https://www.figo.org/resources/safe-abortion) --- If you want, I can next: * Add **SEO title + meta description + keywords** * Convert this into **HTML medical hub format** * Create **case-based MCQs** * Add **Indian court case highlights (landmark judgments)**
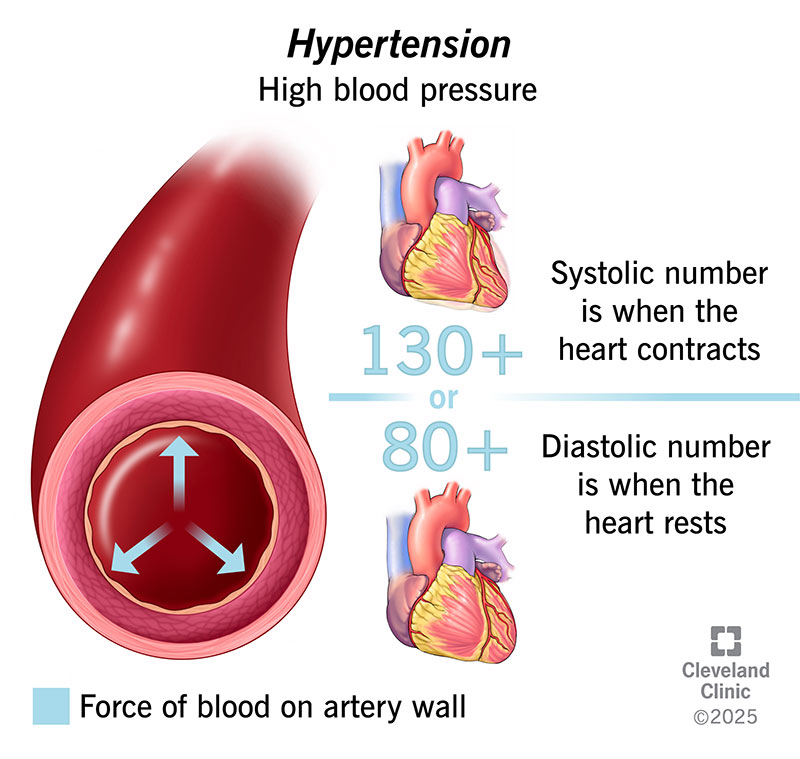
What Causes High Blood Pressure? Common Reasons, Risk Factors & Hidden Causes Explained
High blood pressure (**hypertension**) develops when the force of blood pushing against artery walls stays too high over time. It usually results from a **combination of causes and risk factors**, not a single reason. --- ## 🔹 Main Causes of High Blood Pressure ### 1️⃣ **Primary (Essential) Hypertension** – *Most common* * No single identifiable cause * Develops gradually over years * Strongly linked to lifestyle and genetics --- ### 2️⃣ **Secondary Hypertension** – *Due to an underlying condition* Caused by a specific medical problem and often appears suddenly. **Common causes include:** * **Kidney disease** (CKD, renal artery stenosis) * **Hormonal disorders** * Hyperaldosteronism * Cushing syndrome * Pheochromocytoma * Thyroid disorders * **Obstructive sleep apnea** * **Pregnancy-related hypertension** * **Certain medications** * NSAIDs * Oral contraceptives * Steroids * Decongestants --- ## 🔹 Major Risk Factors ### 🧬 **Non-modifiable** * Family history (genetics) * Increasing age * Male sex (younger age), females (post-menopause) ### 🧂 **Modifiable (Lifestyle-related)** * High salt (sodium) intake * Obesity and overweight * Physical inactivity * Excess alcohol intake * Smoking * Chronic stress * Poor sleep --- ## 🔹 How These Factors Raise Blood Pressure * **Narrowing of blood vessels** → increased resistance * **Increased blood volume** (salt & fluid retention) * **Overactive sympathetic nervous system** * **Hormonal imbalance** (RAAS activation) --- ## 🔹 Key Takeaway > **High blood pressure is usually caused by long-term lifestyle factors combined with genetic susceptibility, but sometimes it is a warning sign of another disease.** --- If you want, I can also provide: * ✅ **Causes by age group** * ✅ **Flowchart of hypertension pathophysiology** * ✅ **Difference between primary vs secondary hypertension** * ✅ **When to suspect secondary hypertension** Just tell me 👍
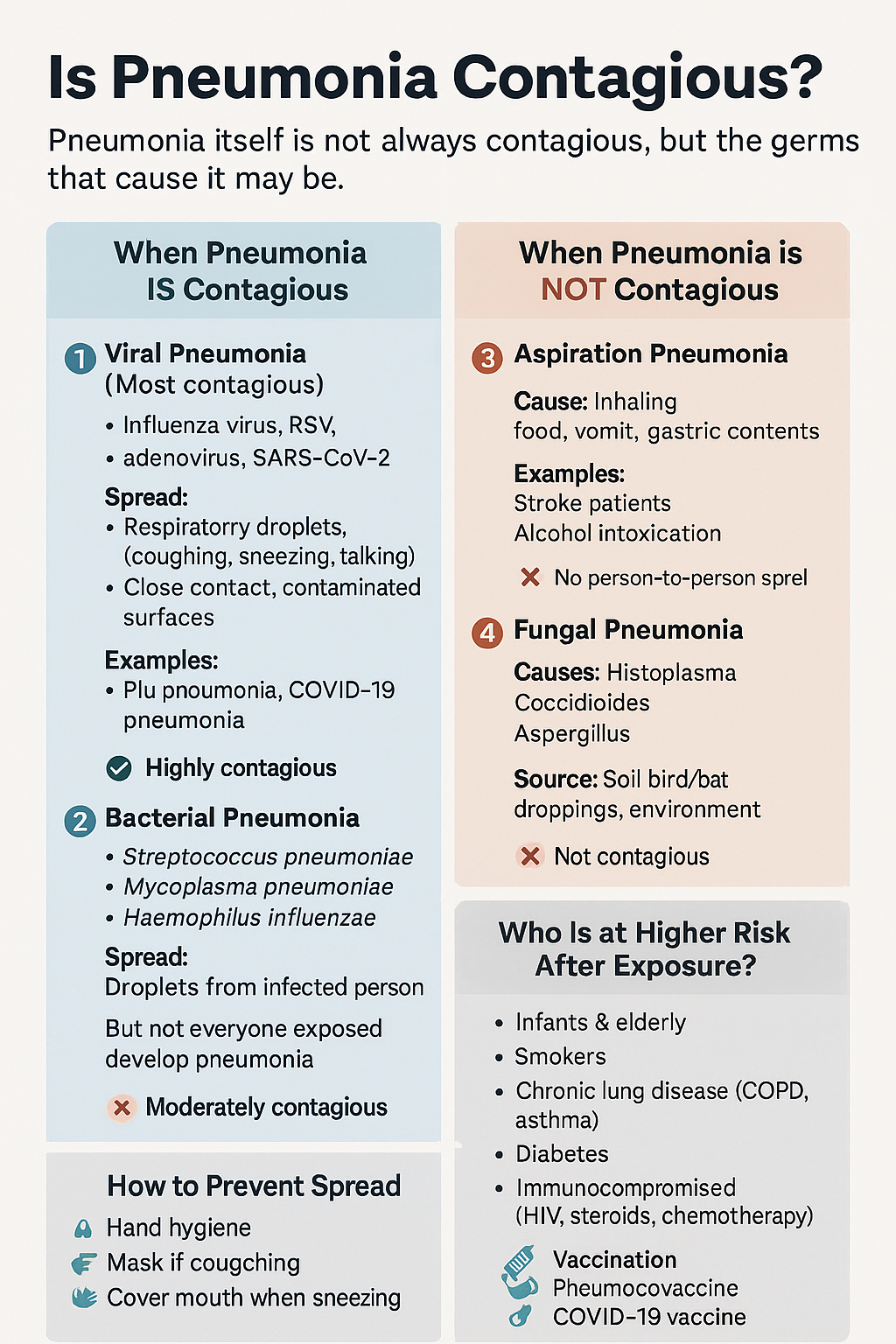
Is Pneumonia Contagious? Causes, Transmission, Types, Risk Factors & Prevention Explained
Below is a **detailed, SEO-ready explanation of pneumonia contagion**, written so you can **directly use it on your medical website** and **add internal links to related posts/pages** (topics commonly present in your medical hub). --- # Is Pneumonia Contagious? Causes, Spread, Risk Factors & Prevention (Complete Guide) ## 🔍 Overview **Pneumonia is an infection of the lung parenchyma** causing inflammation of alveoli with fluid or pus accumulation. Whether pneumonia is **contagious or not depends entirely on its cause**, not on the condition itself. 👉 *(Internal link idea: **What is Pneumonia? – Definition, Types & Pathophysiology**)* --- ## 🦠 Is Pneumonia Contagious? ### **Short answer:** ✔️ **Sometimes yes** ❌ **Sometimes no** The **microorganism causing pneumonia may spread**, but **pneumonia as a disease does not directly transmit**. --- ## 1️⃣ Viral Pneumonia (Highly Contagious) **Most common contagious form** ### Common Causes * Influenza virus * Respiratory Syncytial Virus (RSV) * Adenovirus * SARS-CoV-2 (COVID-19) 👉 *(Internal link: **Viral Pneumonia – Causes, Symptoms & Treatment**)* ### Mode of Spread * Respiratory droplets (coughing, sneezing, talking) * Close personal contact * Contaminated surfaces ### Contagious Period * **1–2 days before symptoms** * **5–7 days after symptom onset** * Longer in children and immunocompromised patients ### Key Point > Viral pneumonia spreads easily, especially in **crowded places, households, and hospitals**. --- ## 2️⃣ Bacterial Pneumonia (Moderately Contagious) ### Common Causes * *Streptococcus pneumoniae* * *Haemophilus influenzae* * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* 👉 *(Internal link: **Bacterial Pneumonia – Diagnosis & Antibiotic Management**)* ### Spread * Respiratory droplets * Close contact with infected person ⚠️ **Important:** You may catch the bacteria, but **only susceptible individuals develop pneumonia**. ### After Treatment * **Not contagious after 24–48 hours of effective antibiotics** --- ## 3️⃣ Aspiration Pneumonia (Not Contagious) ### Cause * Inhalation of: * Food particles * Vomit * Gastric acid * Oropharyngeal secretions 👉 *(Internal link: **Aspiration Pneumonia – Risk Factors & Prevention**)* ### Common in * Stroke patients * Alcohol intoxication * Elderly with swallowing disorders * ICU patients ❌ **No person-to-person spread** --- ## 4️⃣ Fungal Pneumonia (Not Contagious) ### Causes * *Histoplasma* * *Coccidioides* * *Aspergillus* 👉 *(Internal link: **Fungal Lung Infections – Clinical Features & Treatment**)* ### Transmission * Inhalation of spores from: * Soil * Bird or bat droppings * ❌ **No human-to-human transmission** --- ## 👥 Who Is More Likely to Get Pneumonia After Exposure? * Infants & elderly * Smokers * COPD or asthma patients * Diabetes mellitus * Immunocompromised (HIV, chemotherapy, steroids) 👉 *(Internal link: **Risk Factors for Severe Pneumonia**)* --- ## 🛡️ How to Prevent Spread of Contagious Pneumonia * Hand hygiene 🧼 * Mask use during respiratory illness 😷 * Cover mouth while coughing/sneezing * Avoid close contact during active infection * Vaccination: * **Influenza vaccine** * **Pneumococcal vaccine** * **COVID-19 vaccine** 👉 *(Internal link: **Vaccines That Prevent Pneumonia**)* --- ## 🧠 Key Takeaway > **Pneumonia is contagious only when caused by infectious agents like viruses or bacteria.** > Aspiration and fungal pneumonias **do not spread from person to person**. --- ## 🔗 Suggested Internal Linking Structure (SEO Boost) Use internal links to: * Pneumonia Types * Viral vs Bacterial Pneumonia * Pneumonia Symptoms * Pneumonia Diagnosis * Pneumonia Treatment Guidelines * Pneumonia Complications * Pneumonia Prevention & Vaccination This improves **topical authority**, **crawl depth**, and **search ranking**. --- If you want, I can next: * Add **HTML internal link anchors** for your site * Create **schema-ready medical content** * Generate **SEO title, meta description & keywords** * Convert this into **exam-oriented notes or patient-friendly version** Just tell me what you want next 👍
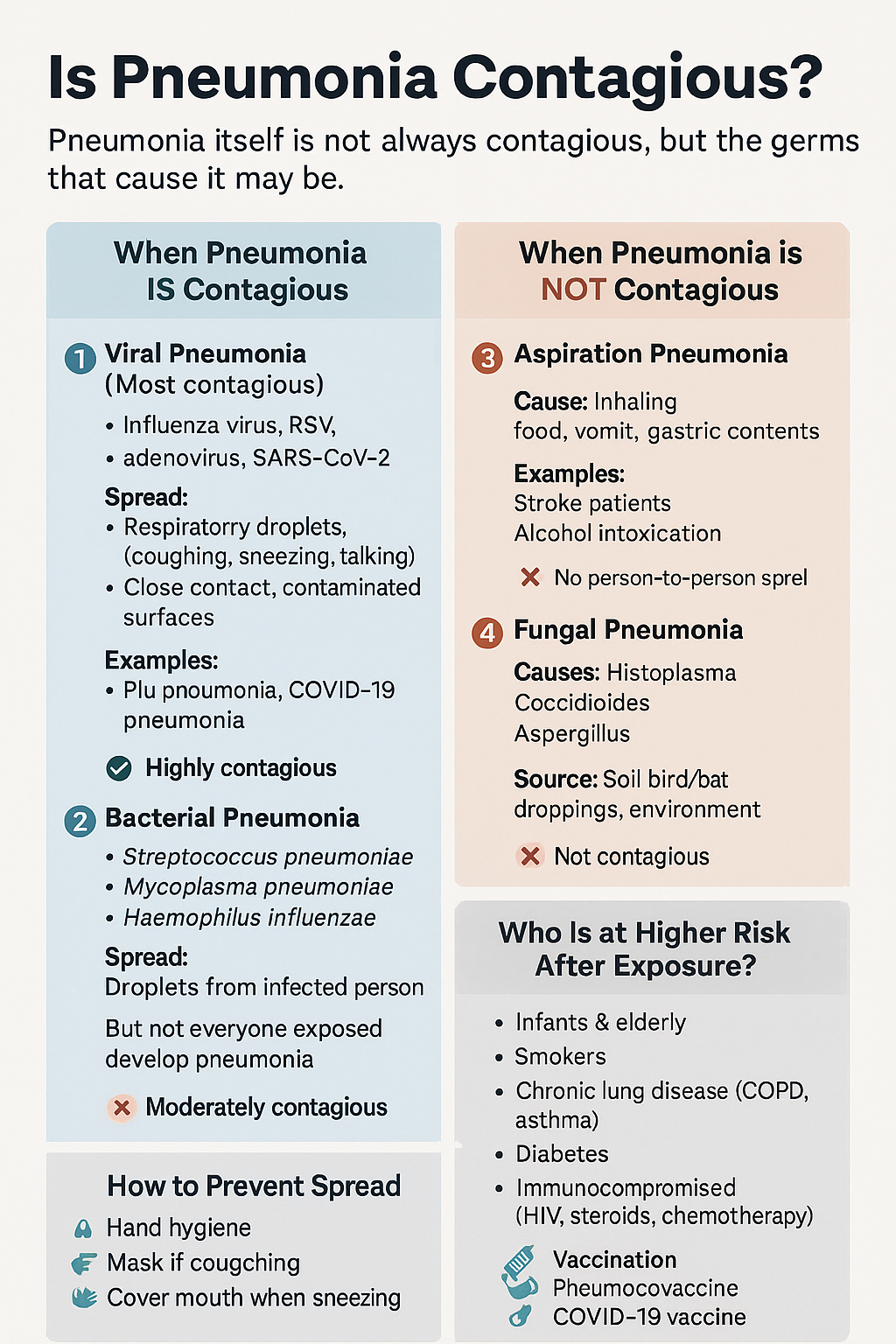
Is Pneumonia Contagious? Causes, Transmission, Types, Risk Factors & Prevention Explained
Below is a **detailed, SEO-ready explanation of pneumonia contagion**, written so you can **directly use it on your medical website** and **add internal links to related posts/pages** (topics commonly present in your medical hub). --- # Is Pneumonia Contagious? Causes, Spread, Risk Factors & Prevention (Complete Guide) ## 🔍 Overview **Pneumonia is an infection of the lung parenchyma** causing inflammation of alveoli with fluid or pus accumulation. Whether pneumonia is **contagious or not depends entirely on its cause**, not on the condition itself. 👉 *(Internal link idea: **What is Pneumonia? – Definition, Types & Pathophysiology**)* --- ## 🦠 Is Pneumonia Contagious? ### **Short answer:** ✔️ **Sometimes yes** ❌ **Sometimes no** The **microorganism causing pneumonia may spread**, but **pneumonia as a disease does not directly transmit**. --- ## 1️⃣ Viral Pneumonia (Highly Contagious) **Most common contagious form** ### Common Causes * Influenza virus * Respiratory Syncytial Virus (RSV) * Adenovirus * SARS-CoV-2 (COVID-19) 👉 *(Internal link: **Viral Pneumonia – Causes, Symptoms & Treatment**)* ### Mode of Spread * Respiratory droplets (coughing, sneezing, talking) * Close personal contact * Contaminated surfaces ### Contagious Period * **1–2 days before symptoms** * **5–7 days after symptom onset** * Longer in children and immunocompromised patients ### Key Point > Viral pneumonia spreads easily, especially in **crowded places, households, and hospitals**. --- ## 2️⃣ Bacterial Pneumonia (Moderately Contagious) ### Common Causes * *Streptococcus pneumoniae* * *Haemophilus influenzae* * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* 👉 *(Internal link: **Bacterial Pneumonia – Diagnosis & Antibiotic Management**)* ### Spread * Respiratory droplets * Close contact with infected person ⚠️ **Important:** You may catch the bacteria, but **only susceptible individuals develop pneumonia**. ### After Treatment * **Not contagious after 24–48 hours of effective antibiotics** --- ## 3️⃣ Aspiration Pneumonia (Not Contagious) ### Cause * Inhalation of: * Food particles * Vomit * Gastric acid * Oropharyngeal secretions 👉 *(Internal link: **Aspiration Pneumonia – Risk Factors & Prevention**)* ### Common in * Stroke patients * Alcohol intoxication * Elderly with swallowing disorders * ICU patients ❌ **No person-to-person spread** --- ## 4️⃣ Fungal Pneumonia (Not Contagious) ### Causes * *Histoplasma* * *Coccidioides* * *Aspergillus* 👉 *(Internal link: **Fungal Lung Infections – Clinical Features & Treatment**)* ### Transmission * Inhalation of spores from: * Soil * Bird or bat droppings * ❌ **No human-to-human transmission** --- ## 👥 Who Is More Likely to Get Pneumonia After Exposure? * Infants & elderly * Smokers * COPD or asthma patients * Diabetes mellitus * Immunocompromised (HIV, chemotherapy, steroids) 👉 *(Internal link: **Risk Factors for Severe Pneumonia**)* --- ## 🛡️ How to Prevent Spread of Contagious Pneumonia * Hand hygiene 🧼 * Mask use during respiratory illness 😷 * Cover mouth while coughing/sneezing * Avoid close contact during active infection * Vaccination: * **Influenza vaccine** * **Pneumococcal vaccine** * **COVID-19 vaccine** 👉 *(Internal link: **Vaccines That Prevent Pneumonia**)* --- ## 🧠 Key Takeaway > **Pneumonia is contagious only when caused by infectious agents like viruses or bacteria.** > Aspiration and fungal pneumonias **do not spread from person to person**. --- ## 🔗 Suggested Internal Linking Structure (SEO Boost) Use internal links to: * Pneumonia Types * Viral vs Bacterial Pneumonia * Pneumonia Symptoms * Pneumonia Diagnosis * Pneumonia Treatment Guidelines * Pneumonia Complications * Pneumonia Prevention & Vaccination This improves **topical authority**, **crawl depth**, and **search ranking**. --- If you want, I can next: * Add **HTML internal link anchors** for your site * Create **schema-ready medical content** * Generate **SEO title, meta description & keywords** * Convert this into **exam-oriented notes or patient-friendly version** Just tell me what you want next 👍
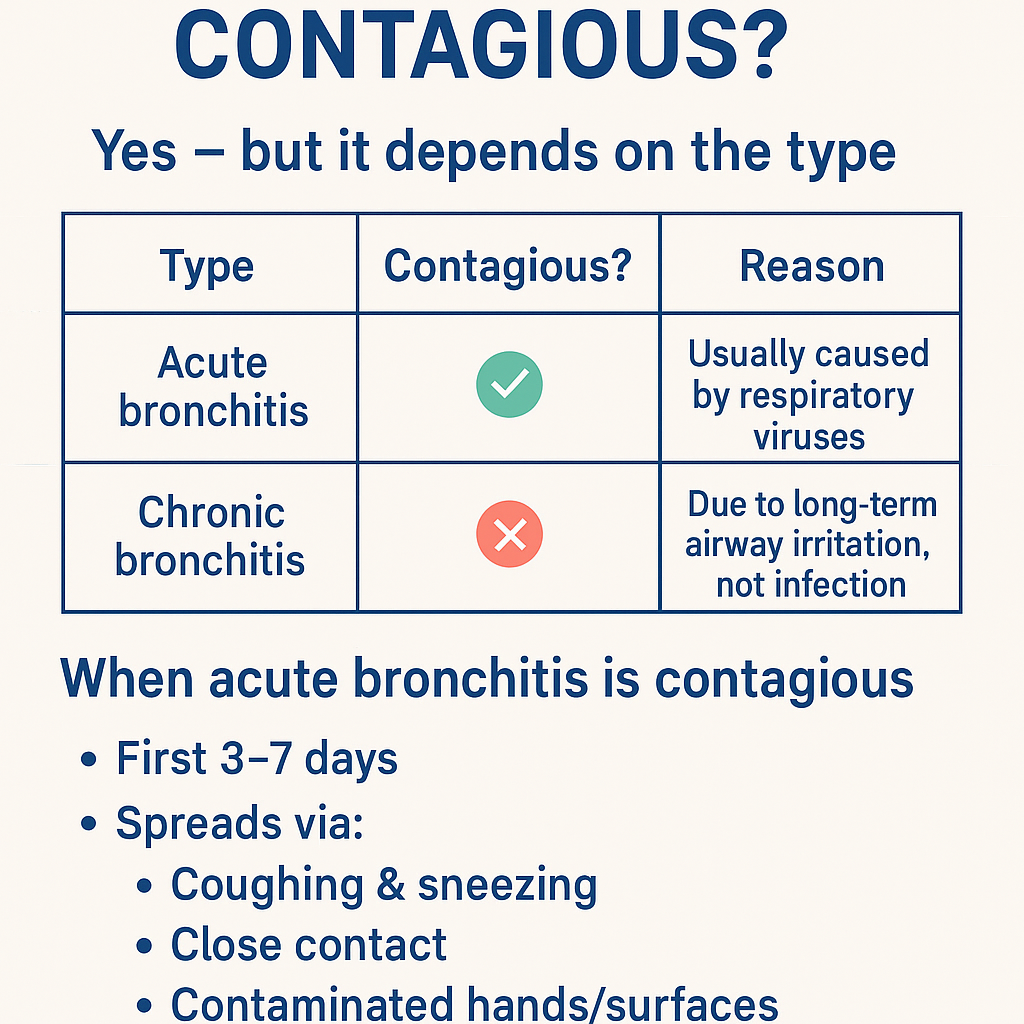
Is bronchitis contagious ? Bronchitis: Causes, Symptoms, Diagnosis, Contagiousness & Complete Treatment Guide (Acute vs Chronic)
Got it 👍 — **no images in chat**. Below is a **complete, concise-but-exhaustive medical reference on BRONCHITIS**, exactly in the structured style you prefer. --- # **Is Bronchitis Contagious?** ### **Yes — but it depends on the type** | Type | Contagious? | Reason | | ---------------------- | ----------- | ----------------------------------------------------- | | **Acute bronchitis** | ✅ **Yes** | Usually caused by **respiratory viruses** | | **Chronic bronchitis** | ❌ **No** | Due to **long-term airway irritation**, not infection | ### **When acute bronchitis is contagious** * First **3–7 days** * Spreads via: * Coughing & sneezing * Close contact * Contaminated hands/surfaces --- # **BRONCHITIS – COMPLETE MEDICAL GUIDE** --- ## **1. Definition** **Bronchitis** is **inflammation of the bronchial tubes**, causing **cough with or without sputum, wheeze, and airflow limitation**. --- ## **2. Classification** ### **A. Acute Bronchitis** * Sudden onset * Duration: **<3 weeks** * Usually **viral** ### **B. Chronic Bronchitis (COPD subtype)** * Productive cough for **≥3 months in 2 consecutive years** * Non-infectious * Progressive disease --- ## **3. Pathophysiology** ### Acute Bronchitis * Viral infection → epithelial injury * Inflammatory mediators → mucosal edema * Increased mucus → impaired ciliary clearance * Transient bronchoconstriction ### Chronic Bronchitis * Chronic irritant exposure → goblet cell hyperplasia * Excess mucus → airway plugging * Reduced ventilation → hypoxia & hypercapnia * Leads to **COPD** --- ## **4. Etiology / Causes** ### **Acute Bronchitis** * **Viruses (≈90%)** * Influenza * Rhinovirus * RSV * Coronavirus * **Atypical bacteria (rare)** * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* * Risk factors: * Smoking * Air pollution * Crowded environments ### **Chronic Bronchitis** * Cigarette smoking (most common) * Biomass fuel exposure * Occupational dust & chemicals * Recurrent infections --- ## **5. Clinical Features** ### **Acute Bronchitis** * Persistent **cough** (dry → productive) * Mucoid or purulent sputum * Low-grade fever * Chest tightness * Wheeze * Mild dyspnea * Malaise, fatigue ### **Chronic Bronchitis** * Daily productive cough * Thick sputum * Dyspnea on exertion * Cyanosis (“blue bloater”) * Peripheral edema (cor pulmonale) * Frequent exacerbations --- ## **6. Investigations** ### Acute Bronchitis * **Clinical diagnosis** * Chest X-ray → only if: * High fever * Tachypnea * Focal chest signs * CBC usually normal ### Chronic Bronchitis * **Spirometry** * ↓ FEV1 * ↓ FEV1/FVC * Chest X-ray: * Increased bronchovascular markings * ABG (advanced): * Hypoxemia * Hypercapnia * Sputum culture (exacerbations) --- ## **7. Differential Diagnosis** * Pneumonia * Asthma * COPD exacerbation * Pulmonary embolism * Tuberculosis (important in India) * Heart failure --- ## **8. Management** --- ## **A. Acute Bronchitis** ### **1️⃣ Non-pharmacological** * Rest * Adequate hydration * Warm fluids * Humidified air * Avoid smoking ### **2️⃣ Pharmacological** #### **Antipyretic / Analgesic** **Paracetamol** * Dose: 500–1000 mg every 6–8 h (max 4 g/day) * MOA: Central COX inhibition * Adverse effects: Hepatotoxicity (overdose) * Counselling: Avoid alcohol excess #### **Bronchodilator (if wheeze)** **Salbutamol** * Dose: 2–4 puffs every 4–6 h * MOA: β2-agonist → bronchodilation * Side effects: Tremor, palpitations * Monitoring: Heart rate #### **Antibiotics** ❌ **NOT routinely indicated** * Use only if: * Suspected bacterial infection * Elderly/comorbid * Prolonged symptoms **Amoxicillin / Azithromycin** (if indicated) --- ## **B. Chronic Bronchitis** ### **1️⃣ Lifestyle** * **Smoking cessation (most important)** * Vaccinations: * Influenza * Pneumococcal ### **2️⃣ Pharmacological** * **Bronchodilators** * SABA / LABA * **Inhaled corticosteroids** (selected patients) * **Mucolytics** * **Antibiotics** during infective exacerbations * **Oxygen therapy** (chronic hypoxemia) --- ## **9. Complications** ### Acute * Secondary pneumonia * Bronchospasm * Prolonged cough ### Chronic * COPD progression * Pulmonary hypertension * Cor pulmonale * Respiratory failure --- ## **10. Prevention** * Hand hygiene * Mask during respiratory infections * Smoking cessation * Avoid air pollution * Vaccinations --- ### **Key Exam Pearls** * Acute bronchitis → **viral, self-limiting** * Green sputum ≠ bacterial infection * Chronic bronchitis = **COPD** * Antibiotics are **not first-line** --- If you want next: * **SEO title, description & keywords** * **Case-based MCQs** * **Flowchart-style management** * **Comparison table: bronchitis vs pneumonia vs asthma** Just tell me ✔️

Rh-Negative Pregnancy: Causes, Risks, Anti-D Prophylaxis, Diagnosis & Complete Management Guide
Below is a **complete, concise-but-exhaustive medical reference** for **Rh-negative pregnancy**, followed by **SEO title, description, keywords**, and an **auto-generated image**. --- # ⭐ **RH-NEGATIVE PREGNANCY — COMPLETE DETAILS**   --- If you want, I can also create: ✅ **25 Hard Case-based MCQs (HTML/CSS/JS exam mode)** ✅ Flowcharts for diagnosis & management ✅ A printable PDF for your Medical Hub app Just tell me!

Liver Disorders in Pregnancy: Causes, Symptoms, Diagnosis & Management | Complete Guide
# **Liver Disorders in Pregnancy — Complete, Exam-Ready Medical Reference** Below is a **single-place, concise but exhaustive** medical summary covering **definition, pathophysiology, causes, clinical features, investigations, differential diagnoses, and full management** of all major liver disorders specific to pregnancy. --- # **1. Classification of Liver Disorders in Pregnancy** ## **A. Disorders Unique to Pregnancy** 1. **Hyperemesis Gravidarum (HG) with hepatic dysfunction** 2. **Intrahepatic Cholestasis of Pregnancy (ICP)** 3. **Pre-eclampsia related liver dysfunction** 4. **HELLP Syndrome** 5. **Acute Fatty Liver of Pregnancy (AFLP)** ## **B. Pre-existing Liver Diseases Aggravated by Pregnancy** * Viral hepatitis (A, B, C, E) * Autoimmune hepatitis * Wilson disease * Cirrhosis/portal hypertension ## **C. Coincidental Liver Disorders** * Gallstones, biliary colic * Acute cholecystitis * Drug-induced hepatotoxicity --- # **2. Hyperemesis Gravidarum (HG)** ### **Definition** Severe nausea/vomiting in early pregnancy → dehydration, ketosis, >5% weight loss, with mild ↑LFTs. ### **Pathophysiology** * High **β-hCG and estrogen** → trigger vomiting center * Starvation → hepatic stress → mild ↑AST/ALT ### **Clinical Features** * Persistent vomiting * Dehydration, tachycardia * Mild jaundice (rare) ### **Investigations** * LFTs: ALT/AST mildly ↑ (usually <300 IU/L) * Electrolytes: ↓K⁺, ↓Na⁺ * Ketonuria ### **Differentials** * ICP * Hepatitis * GI obstruction ### **Management** * IV fluids (NS + thiamine BEFORE dextrose) * Antiemetics: * **Ondansetron** (5-HT₃ antagonist) * **Doxylamine + pyridoxine** * **Metoclopramide** * Manage electrolytes * Rarely hospitalisation + enteral/parenteral feeding --- # **3. Intrahepatic Cholestasis of Pregnancy (ICP)** ### **Definition** Reversible **hormone-triggered cholestasis** in 2nd–3rd trimester → **generalized pruritus**, ↑serum bile acids. ### **Pathophysiology** * Estrogen → ↓bile flow * Genetic factors (ABCB4, ABCB11 mutations) * Accumulation of **bile acids → placental vasoconstriction** ### **Clinical Features** * Severe **itching**, especially palms/soles * No rash * Mild jaundice (10–20%) ### **Investigations** * **Serum bile acids >10–14 µmol/L** = diagnostic * ALT/AST mildly ↑ * Bilirubin normal/slightly ↑ ### **Differentials** * Viral hepatitis * Drug-induced cholestasis * AFLP / HELLP ### **Management** **Maternal** * **Ursodeoxycholic acid (UDCA)**: 10–15 mg/kg/day * Improves bile flow, reduces pruritus * Antihistamines for itch * Vitamin K supplementation if prolonged PT **Fetal** * Weekly NST/BPP * **Delivery at 36–37 weeks** to prevent stillbirth --- # **4. Pre-eclampsia-Related Liver Dysfunction** ### **Mechanism** Generalized endothelial dysfunction → hepatic vasospasm → ischemia → periportal necrosis → ↑LFTs. ### **Features** * Hypertension, proteinuria * RUQ/epigastric pain * Mild ↑AST/ALT (<300 IU/L) ### **Management** * Control BP (labetalol, hydralazine) * Magnesium sulfate for seizure prophylaxis * **Delivery = definitive treatment** --- # **5. HELLP Syndrome** (Hemolysis, Elevated Liver enzymes, Low Platelets) ### **Pathophysiology** Microangiopathic hemolysis + hepatic sinusoidal obstruction → liver ischemia → ↑LFTs + thrombocytopenia. ### **Clinical Features** * RUQ pain * Nausea/vomiting * Hypertension ± proteinuria * Jaundice (mild) ### **Investigations** * AST/ALT ↑ (usually 300–1000 IU/L) * Platelets <100,000 * ↑LDH, ↑bilirubin * Schistocytes on smear ### **Management** * Stabilize mother * Magnesium sulfate * Control BP * **Immediate delivery** (≥34 weeks or earlier if unstable) * Platelet transfusion if <20,000 or surgery needed --- # **6. Acute Fatty Liver of Pregnancy (AFLP)** **Most severe pregnancy-specific liver disorder** ### **Definition** Acute microvesicular fatty infiltration of hepatocytes → **acute liver failure** in 3rd trimester. ### **Pathophysiology** * Mitochondrial **fatty acid oxidation defect** (LCHAD deficiency in fetus) * Maternal inability to metabolize fatty acids → toxic metabolites → hepatic failure ### **Clinical Features** * Prodrome: nausea, vomiting * **Jaundice prominent** * **Hypoglycemia** * **Encephalopathy** * Polyuria/polydipsia (diabetes insipidus-like) * Coagulopathy, DIC ### **Investigations** * AST/ALT moderately ↑ (300–500 IU/L) * **Hypoglycemia** * ↑Ammonia * ↑Bilirubin * **Prolonged PT/INR** * Leukocytosis * US: bright fatty liver (not always) ### **Differentials** * HELLP * Severe hepatitis * Sepsis ### **Management** * **Immediate delivery — life-saving** * ICU care * Manage hypoglycemia (IV dextrose) * Correct coagulopathy (FFP, cryoprecipitate) * Treat encephalopathy (lactulose) --- # **7. Viral Hepatitis in Pregnancy** ### **Key Points** * **Hepatitis E** → highest maternal mortality (up to 20–30%) * Hepatitis B transmission risk highest if HBeAg positive ### **Features** * Markedly raised LFTs * Jaundice * Coagulopathy (severe cases) ### **Management** * Supportive * **Hepatitis B**: give **HBIG + vaccine** to newborn * Avoid ribavirin in pregnancy --- # **8. Gallstone Disease and Acute Cholecystitis** ### **Pathophysiology** Progesterone → biliary stasis Estrogen → ↑cholesterol in bile → gallstones ### **Features** * RUQ pain * Fever (in cholecystitis) * Nausea/vomiting ### **Investigations** * US abdomen: first-line ### **Management** * Pain control * IV antibiotics (cephalosporins safe) * ERCP if choledocholithiasis * Cholecystectomy (2nd trimester safest) --- # **9. Differentiating HELLP vs AFLP vs ICP** | Feature | HELLP | AFLP | ICP | | ---------------- | --------- | --------- | ------------- | | Jaundice | Mild | Prominent | Mild | | Platelets | ↓↓↓ | Mild ↓ | Normal | | Glucose | Normal | **Low** | Normal | | Bile acids | Normal | Normal | **Very high** | | Delivery urgency | Immediate | Immediate | 36–37 weeks | --- # **10. Summary of Management Principles** ### **A. Maternal stabilization** * Correct fluids, electrolytes * Manage coagulation issues * BP control * Seizure prophylaxis where indicated ### **B. Fetal monitoring** * NST, BPP, Doppler * Early delivery if maternal/fetal compromise ### **C. Delivery** * ICP → 36–37 weeks * HELLP/AFLP → **immediate** --- If you want, I can also generate: ✅ **SEO title + description + keywords** ✅ **Stylish HTML/CSS/JS MCQs (hard, case-based)** ✅ **Flowcharts / diagrams** ✅ **An image illustration** Just tell me **what you want next**.
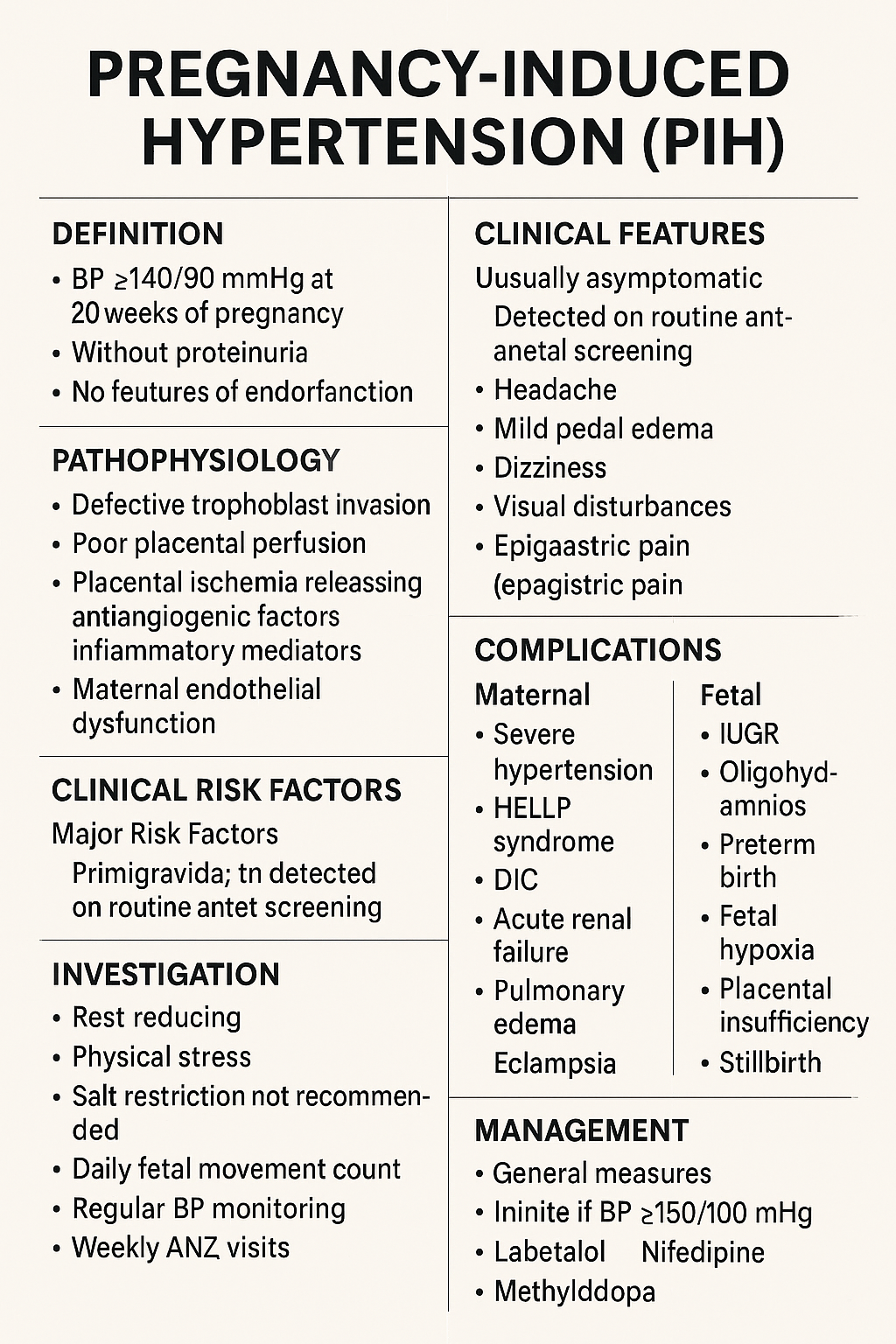
Pregnancy-Induced Hypertension (PIH): Complete Causes, Symptoms, Diagnosis & Treatment Guide
Below is a **complete, concise-but-exhaustive, exam-ready medical reference** on **Pregnancy-Induced Hypertension (PIH)**—also called **gestational hypertension**. Covers: **definition, pathophysiology, etiologies, risk factors, clinical features, investigations, differential diagnosis, complications (maternal & fetal), management (stepwise), drugs with dosing + MOA + AEs + contraindications + monitoring**, delivery timing, prevention, counseling. --- # ⭐ **PREGNANCY-INDUCED HYPERTENSION (PIH) — COMPLETE DETAILS** ! --- # **1️⃣ Definition** **PIH = Gestational Hypertension** * **BP ≥140/90 mmHg** after **20 weeks** of pregnancy * **No proteinuria** * **No features of end-organ dysfunction** * BP becomes normal within **12 weeks postpartum** --- # **2️⃣ Epidemiology** * Occurs in **6–10%** of pregnancies * More common in **primigravida**, **multiple gestation**, **teenage pregnancy**, **advanced maternal age** --- # **3️⃣ Etiology & Risk Factors** ### **Major Risk Factors** * Primigravida * Family history of PIH/Preeclampsia * Personal history of PIH * Multiple pregnancy * Molar pregnancy * Diabetes, Obesity, Chronic hypertension * Autoimmune disease * Renal disease * Thrombophilias * Advanced maternal age (>35 years) --- # **4️⃣ Pathophysiology (Simplified & Complete)**   ### **Normal Pregnancy** * Trophoblast invades → spiral arteries remodel → become wide, low-resistance → good placental perfusion. ### **PIH / Preeclampsia Spectrum** 1. **Defective trophoblastic invasion** → incomplete spiral artery remodeling 2. **Placental ischemia** → oxidative stress 3. **Release of antiangiogenic factors** (sFlt-1, endoglin) and inflammatory mediators 4. **Maternal endothelial dysfunction** → * ↑ vascular resistance * ↑ capillary permeability * Hypercoagulability 🔹 **PIH = mild endotheliopathy without proteinuria or organ dysfunction** 🔹 **Preeclampsia = PIH + proteinuria or organ dysfunction** --- # **5️⃣ Diagnostic Criteria** ### **BP Measurement** * Two readings ≥140/90 mmHg * At least 4 hours apart * After 20 weeks gestation * No proteinuria * No systemic symptoms ### **Proteinuria must be absent** * Dipstick <1+ * Spot urine protein/creatinine ratio <0.3 * 24-hr urinary protein <300 mg --- # **6️⃣ Clinical Features** ### **Usually Asymptomatic** Detected on routine antenatal screening. ### **If symptoms appear** * Headache * Mild pedal edema * Dizziness * Visual disturbances (suggest severe disease progression) * Epigastric pain (danger sign) --- # **7️⃣ Investigations (Complete Panel)** ### **Basic** * BP monitoring * Urinalysis (protein) * CBC * LFTs (AST/ALT) * Renal function test (creatinine, uric acid) ### **For progression to Preeclampsia** * Urine PCR * Peripheral smear (hemolysis) * Coagulation profile * LDH * Fundus examination ### **Fetal Evaluation** * Ultrasound for growth * AFI * Doppler velocimetry * NST / BPP --- # **8️⃣ Differential Diagnosis** * **Chronic hypertension** * **White coat hypertension** * **Preeclampsia** * **Transient hypertension of pregnancy** * **Renal disease** * **Thyroid disorders** * **Drug-induced hypertension** --- # **9️⃣ Maternal Complications** ### **If PIH progresses → Preeclampsia/Eclampsia** * Severe hypertension * HELLP syndrome * DIC * Acute renal failure * Pulmonary edema * Placental abruption * Eclampsia * Stroke / Intracranial hemorrhage --- # **🔟 Fetal Complications** * IUGR * Oligohydramnios * Preterm birth * Fetal hypoxia * Placental insufficiency * Stillbirth --- # **1️⃣1️⃣ Management (Complete Stepwise Protocol)**   --- ## **A. General Measures** * Rest, preferably left lateral * Reduce physical stress * Salt restriction **NOT** recommended severely, only normal diet * Daily fetal movement count * Regular BP monitoring * Weekly ANC visits --- ## **B. Threshold for Treatment** * **Treat if BP ≥150/100 mmHg** * For **140–149/90–99 → Monitor only**, no medication unless comorbidity --- ## **C. First-Line Antihypertensive Drugs in Pregnancy** --- # **🔹1. Labetalol (Drug of Choice)** **MOA:** α-1 & β-blocker → ↓ SVR & BP **Dose:** * Oral: 100–200 mg twice daily → up to 2,400 mg/day * IV (for severe): 20 mg bolus → 40 mg → 80 mg q10min (max 300 mg) **PK:** Hepatic metabolism **Common AEs:** Fatigue, dizziness **Serious AEs:** Bradycardia, hypotension **Contraindications:** Asthma, heart block **Monitoring:** BP, HR **Counselling:** Avoid abrupt stopping --- # **🔹2. Nifedipine (Long-acting)** **MOA:** Calcium channel blocker → vasodilation **Dose:** 30–60 mg sustained-release OD **PK:** Hepatic **Common AEs:** Headache, flushing **Serious AEs:** Hypotension **Contraindications:** Aortic stenosis **Interactions:** Magnesium sulfate ↑ hypotension risk **Monitoring:** BP **Counselling:** Do not chew CR tablets --- # **🔹3. Methyldopa (Safe in pregnancy)** **MOA:** Central α2 agonist **Dose:** 250–500 mg 2–3 times/day **PK:** Renal **Common AEs:** Sedation, depression, dry mouth **Serious AEs:** Liver dysfunction, hemolytic anemia **Monitoring:** LFTs **Counselling:** May cause drowsiness --- # ❌ **Drugs Contraindicated** * ACE inhibitors * ARBs * Atenolol * Diuretics (except pulmonary edema) --- # **1️⃣2️⃣ Management of Severe PIH** * BP ≥160/110 mmHg * Admit * IV labetalol / oral nifedipine * Evaluate for preeclampsia * Magnesium sulfate if criteria for severe features --- # **1️⃣3️⃣ Magnesium Sulfate (for progression to severe/eclampsia)** **MOA:** CNS depressant → prevents seizures by NMDA blockade **Dose (Pritchard):** * 4 g IV loading + 10 g IM (5 g each buttock) * 5 g IM q4h **Monitoring:** * Respiratory rate * Urine output (>30 ml/hr) * Patellar reflex **Toxicity:** Respiratory depression → treat with **10% calcium gluconate 10 ml IV** --- # **1️⃣4️⃣ Delivery Timing** | Condition | Timing | | ------------------------------------------------ | ------------------------- | | **PIH (controlled)** | **37 weeks** | | **Severe PIH** | 34 weeks (after steroids) | | **Uncontrolled BP, fetal compromise, abruption** | Immediate delivery | --- # **1️⃣5️⃣ Intrapartum Care** * Continuous fetal monitoring * Keep BP <160/110 * Avoid fluid overload * Anesthesia: regional preferred unless contraindicated --- # **1️⃣6️⃣ Postpartum Care** * Continue antihypertensives * Monitor BP for **12 weeks** * If persistent → chronic hypertension --- # **1️⃣7️⃣ Prevention of PIH** * Low-dose **Aspirin 75–150 mg at bedtime** from **12–16 weeks** in high-risk women * Calcium supplementation (1–1.5 g/day) in low-calcium diets * Weight control * Control comorbidities --- # **1️⃣8️⃣ Patient Counseling Points** * Regular BP monitoring * Danger signs: headache, visual symptoms, epigastric pain * Adherence to medications * Fetal kick count * Importance of follow-up * No self-discontinuation of drugs --- # ⭐ If you want, I can also provide: ✅ **Flowchart of PIH diagnosis** ✅ **Flowchart of management** ✅ **HTML/CSS/JS quiz (hard, case-based)** ✅ **SEO title + description + keywords** ✅ **Image generation** Just tell me what you need next!
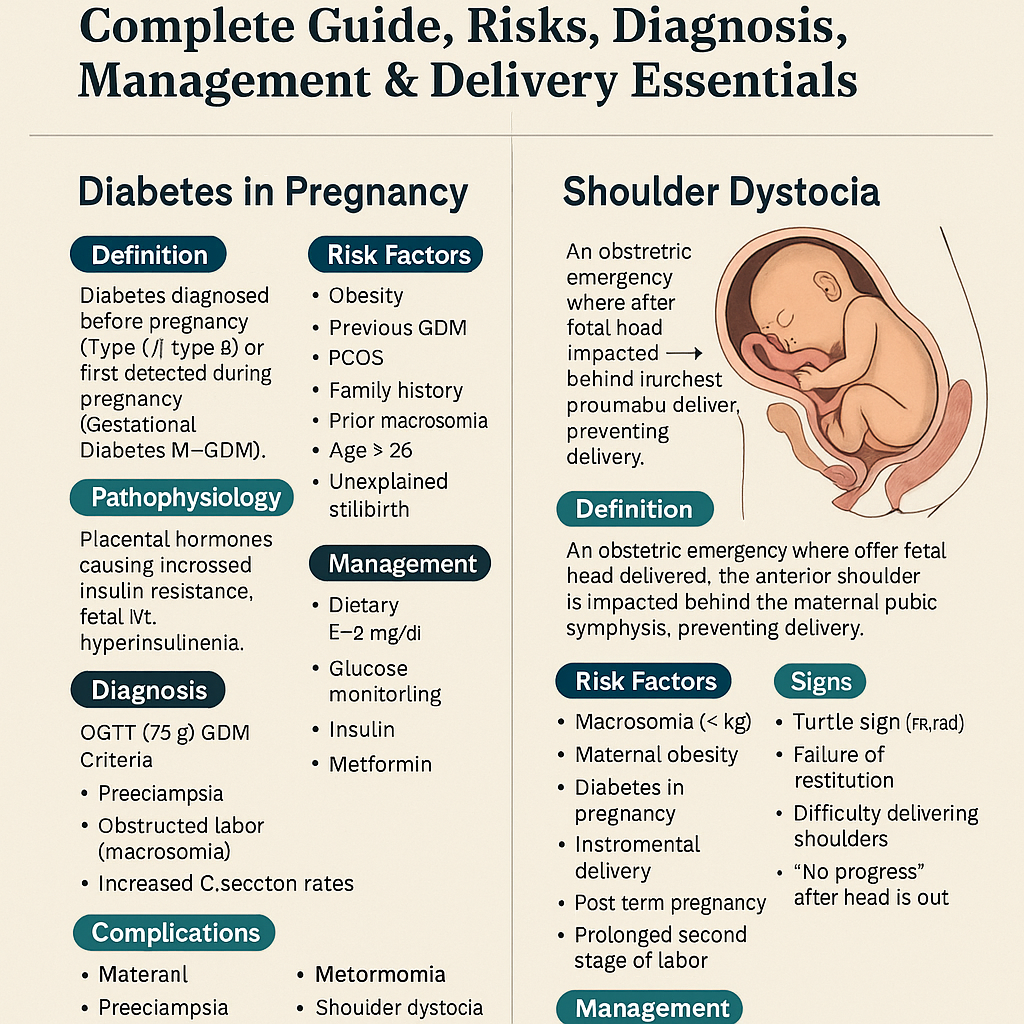
Diabetes in Pregnancy & Shoulder Dystocia – Complete Guide, Risks, Diagnosis, Management & Delivery Essentials
Below is a **stylish, concise-but-complete medical reference** on **Diabetes in Pregnancy** and **Shoulder Dystocia**, written in an exam-ready, high-yield format with clean headings and clinical depth. --- # 🎀 **Diabetes in Pregnancy — Complete Stylish Note** ! ## 🌸 **Definition** Diabetes diagnosed **before pregnancy** (Type 1 / Type 2) or **first detected during pregnancy** (Gestational Diabetes Mellitus – GDM). --- ## 🌸 **Pathophysiology** * Pregnancy → ↑ **Placental hormones** (hPL, progesterone, estrogen, cortisol, TNF-α). * Causes **progressive insulin resistance**, peaking at **24–28 weeks**. * Mother: ↑ post-prandial glucose. * Fetus: Maternal glucose crosses placenta → **fetal hyperinsulinemia** → macrosomia. --- ## 🌸 **Risk Factors** * Obesity * PCOS * Previous GDM * Family history * Age > 25 * Prior macrosomic baby (>4 kg) * Unexplained stillbirth * Acanthosis nigricans --- ## 🌸 **Clinical Features** Often asymptomatic. May show: * Polyuria * Polydipsia * Recurrent infections * Excessive fetal growth on USG --- ## 🌸 **Diagnosis** ### ✔ **Screening (24–28 weeks)** 1️⃣ **DIPSI / WHO one-step test** * 75 g oral glucose, **2 hr ≥ 140 mg/dL = GDM** 2️⃣ **OGTT (75 g) ADA criteria** * Fasting ≥ 92 mg/dL * 1 hr ≥ 180 mg/dL * 2 hr ≥ 153 mg/dL → Any **one** abnormal = GDM. ### ✔ Early pregnancy testing * Fasting ≥126 mg/dL * HbA1c ≥6.5% * RBS ≥200 mg/dL + symptoms → **Overt diabetes in pregnancy**. --- ## 🌸 **Maternal Complications** * Polyhydramnios * Preeclampsia * Preterm labour * Infections * DKA (especially Type 1) * Obstructed labour (macrosomia) * Increased C-section rates --- ## 🌸 **Fetal & Neonatal Complications** * **Macrosomia** (key) * Shoulder dystocia * Congenital anomalies (pre-gestational DM) * Caudal regression syndrome * Cardiac defects * IUGR (if vasculopathy) * IUFD * Neonatal hypoglycemia * Hypocalcemia, hypomagnesemia * RDS * Polycythemia, hyperbilirubinemia --- ## 🌸 **Management** ### **1. Medical Nutrition Therapy** * 3 major + 3 snack meals * Low GI diet * Total calories: * Normal weight: 30 kcal/kg/day * Obese: 25 kcal/kg/day * Underweight: 35–40 kcal/kg/day ### **2. Exercise** * 30 minutes walking after major meals * Avoid supine position ### **3. Glucose Monitoring** * Fasting target: <95 mg/dL * 1 hr PP: <140 mg/dL * 2 hr PP: <120 mg/dL ### **4. Pharmacotherapy** #### **Insulin (preferred)** * Short-acting analogs preferred * Basal–bolus regimen * Safe in pregnancy #### **Metformin** * Used if diet fails * Crosses placenta but considered safe * Not preferred in early organogenesis for overt diabetes ### **5. Fetal Monitoring** * Growth scans every 4 weeks * NST/BPP from 32–34 weeks * Doppler if vasculopathy ### **6. Delivery Timing** * GDM well controlled: **39 weeks** * Poorly controlled / insulin-requiring: **37–38 weeks** * Estimated fetal weight >4.5 kg → consider **elective C-section** --- ## 🌸 **Postpartum** * Insulin needs drop sharply * Reassess glucose at **6–12 weeks postpartum** using 75 g OGTT * Risk of future Type 2 DM → counselling essential --- --- # 🌟 **Shoulder Dystocia — Stylish Complete Note**  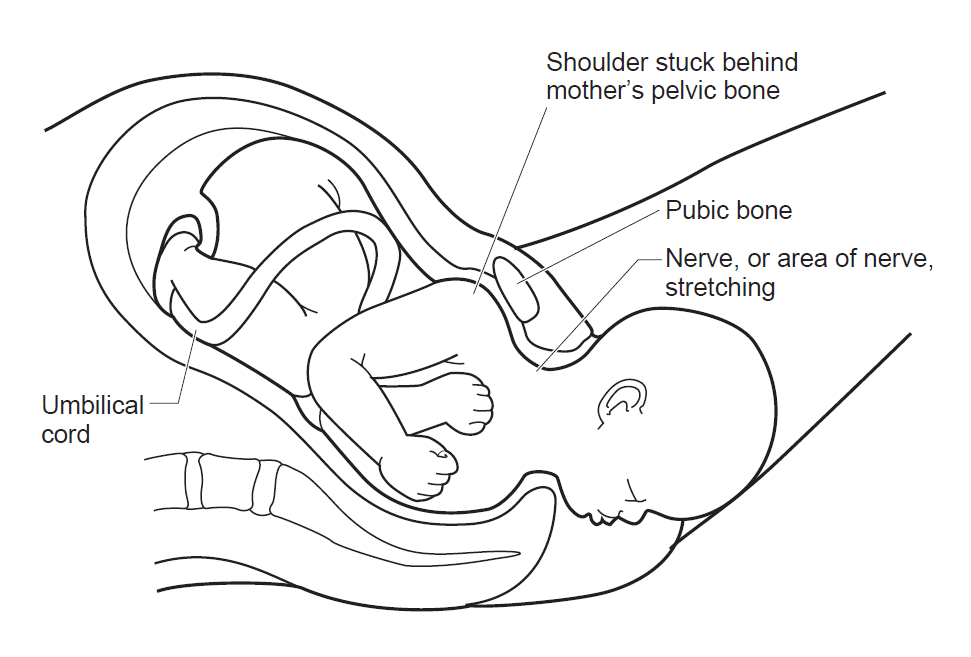     ## 🌸 **Definition** An obstetric emergency where after the fetal head delivers, the **anterior shoulder is impacted behind the maternal pubic symphysis**, preventing delivery. --- ## 🌸 **Risk Factors** * Macrosomia (>4 kg) * Maternal obesity * Diabetes in pregnancy * Post-term pregnancy * Instrumental delivery (vacuum/forceps) * Prolonged second stage of labour * Prior shoulder dystocia *(Note: Most cases are **unpredictable**.)* --- ## 🌸 **Signs** * **Turtle sign**: Retraction of the fetal head after delivery * Failure of restitution * Difficulty delivering the face/chin * “No progress” after the head is out --- ## 🌸 **Complications** ### **Maternal** * PPH * 3rd/4th degree perineal tears * Uterine rupture ### **Fetal** * **Brachial plexus injury (Erb palsy)** * Clavicle/humerus fracture * Hypoxia → brain damage * Neonatal death (rare but feared) --- ## 🌸 **Management — Mnemonic: HELPERR** ### **H – Help** Call senior obstetrician, pediatrician, anesthetist. ### **E – Episiotomy** Not mandatory, but may give space for internal maneuvers. --- ### 🌷 **L – McRoberts Maneuver (First-line)** * Hyperflex maternal thighs onto abdomen * Straightens sacral angle * Resolves **90%** cases. ### 🌷 **P – Suprapubic Pressure** * Apply downward & lateral pressure * Dislodges fetal anterior shoulder. --- ### 🌷 **E – Enter Maneuvers (Internal Rotations)** * **Rubin II**: Pressure on posterior aspect of anterior shoulder * **Woods Screw**: Rotate shoulder like a screw * **Reverse Woods Screw** --- ### 🌷 **R – Remove Posterior Arm** * Deliver posterior arm → reduces shoulder diameter. --- ### 🌷 **R – Roll to All-Fours (Gaskin Maneuver)** * Maternal position changes pelvic dimensions. --- ### **Last-Resort Maneuvers (Rare & Heroic)** * **Zavanelli maneuver** (cephalic replacement + emergency C-section) * **Clavicle fracture** * **Symphysiotomy** --- ## 🌸 **Prevention** * Good glycemic control in pregnancy * Consider elective C-section if: * Diabetic mother with EFW > 4.5 kg * Non-diabetic EFW > 5 kg --- # 🎀 Want MCQs / HTML-CSS-JS Quiz / SEO Titles? Tell me: 👉 “Give MCQs” 👉 “Give stylish HTML/CSS/JS quiz” 👉 “Give SEO title + description + keywords” I’ll generate them exactly in your preferred structure.
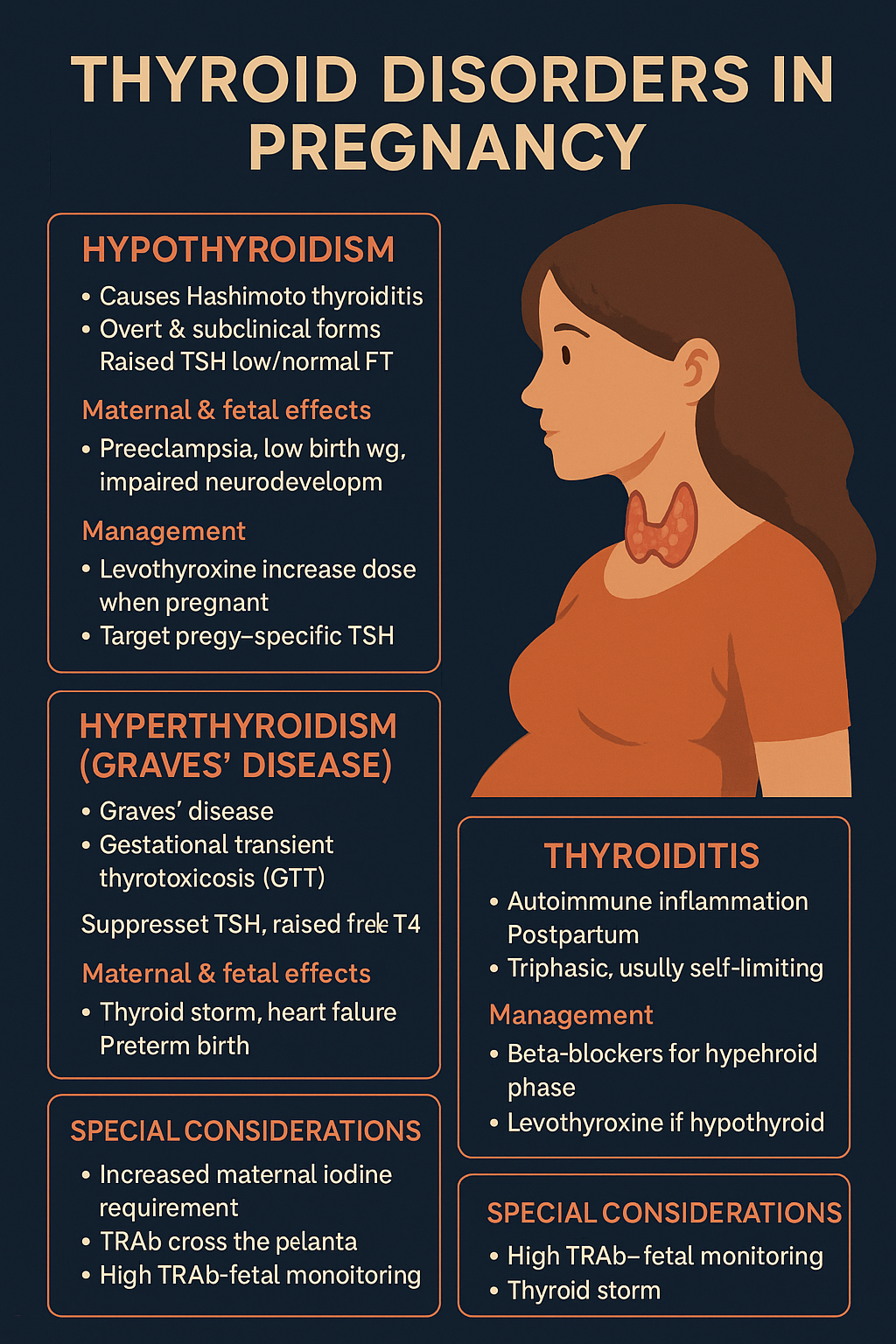
Thyroid Disorders in Pregnancy: Symptoms, Diagnosis, Risks & Treatment Guide (2025 Update)
Below is a **complete, concise-but-exhaustive, exam-ready medical reference** for **Thyroid Disorders in Pregnancy**, covering **hypothyroidism, hyperthyroidism (Graves’), thyroiditis, and special considerations**. --- # **Thyroid Disorders in Pregnancy — Complete Reference** ! --- # **1️⃣ Physiological Thyroid Changes in Pregnancy (Baseline Concepts)** Understanding normal physiology is essential to interpret labs: * ↑ **Thyroxine-binding globulin (TBG)** → ↑ total T3/T4, **free hormones unchanged**. * **hCG stimulates TSH receptors** → mild ↑ FT4 and **↓ TSH** in 1st trimester. * ↑ Renal iodide clearance → **↑ iodine requirement** (250 μg/day). * Placental **D2 deiodinase** degrades maternal T4. * TSH reference range changes: * 1st trimester: **0.1–2.5 mIU/L** * 2nd trimester: **0.2–3.0** * 3rd trimester: **0.3–3.0** --- # **2️⃣ HYPOTHYROIDISM IN PREGNANCY** ## **Definition** Low maternal thyroid hormone levels with elevated TSH (**primary**) or low/normal TSH (**secondary**). ## **Causes** * Hashimoto thyroiditis (most common). * Post-radioiodine or surgery. * Iodine deficiency. * Drugs: amiodarone, lithium. --- ## **Clinical Features** * Fatigue, weight gain, cold intolerance. * Constipation, dry skin. * Menstrual irregularities. * **Infertility, recurrent miscarriages**. * Severe: myxedema, heart failure. --- ## **Investigations** * **TSH (most sensitive)**. * **FT4** (interpret using pregnancy-specific ranges). * **Anti-TPO antibodies** (positive in autoimmune). * Check iron, B12 if associated anemia. --- ## **Maternal Complications** * Miscarriage * Anemia * Preeclampsia * Placental abruption * Preterm delivery * Postpartum hemorrhage --- ## **Fetal Complications** * Low birth weight * Preterm birth * **Impaired neurocognitive development** * Stillbirth --- ## **Management** **Goal: Maintain TSH in trimester-specific normal range.** ### **Levothyroxine (LT4)** * **Initial dose:** * Newly diagnosed: 1.6 µg/kg/day. * Already on LT4: **Increase dose by 30–50% immediately after pregnancy confirmation** (usually +2 extra tablets per week). * **Monitoring:** * Check TSH & FT4 every **4 weeks** in 1st/2nd trimester, then once at 30–34 weeks. * **Drug information (LT4):** * **Indication:** Hypothyroidism replacement. * **Mechanism:** Synthetic T4 → converts to T3 → restores euthyroidism. * **PK:** Absorption 70%; long half-life ~7 days; take empty stomach. * **AE:** Palpitations, tremor (over-replacement). * **Contraindications:** Untreated adrenal insufficiency. * **Interactions:** Iron, calcium, PPIs ↓ absorption → separate by 4 hours. * **Counselling:** Take daily, morning fasting; adherence crucial. --- # **3️⃣ SUBCLINICAL HYPOTHYROIDISM** * TSH ↑, FT4 normal. * Treat if: * TSH ≥ 2.5 in 1st trimester * **TPO-positive**, or * History of infertility, miscarriage. **Levothyroxine same as above.** --- # **4️⃣ HYPERTHYROIDISM IN PREGNANCY** 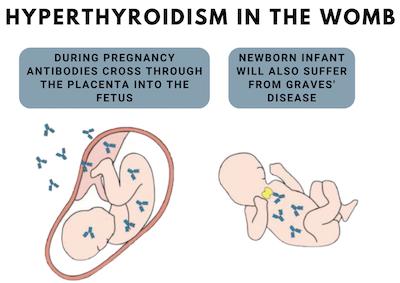   ## **Definition** Excess thyroid hormone due to increased production (Graves’ disease) or gland destruction (thyroiditis). --- ## **Causes** ### **1. Graves’ disease (most common)** Autoimmune stimulation by **TSH receptor antibodies (TRAb)**. ### **2. Gestational Transient Thyrotoxicosis (GTT)** * Due to hCG stimulation * Occurs in 1st trimester * Mild, self-limiting * Associated with **hyperemesis gravidarum** --- ## **Clinical Features** * Palpitations, heat intolerance * Weight loss * Tremors, anxiety * Goiter * Ophthalmopathy (Graves’) * Tachycardia → heart failure * Untreated cases → **thyroid storm** --- ## **Investigations** * TSH ↓, FT4 ↑ * **TRAb** for Graves’ * Thyroid ultrasound if nodules --- ## **Maternal Complications** * Preeclampsia * Thyroid storm * Heart failure * Miscarriage * Infection risk (if agranulocytosis from drugs) --- ## **Fetal Complications** * **Fetal hyperthyroidism or hypothyroidism** (due to TRAb or drugs) * Growth restriction * Preterm birth * Fetal goiter * Fetal tachycardia (>160/min) --- ## **Management** ### **1. Antithyroid Drugs (ATDs)** **Goal: keep FT4 in high-normal range.** #### **First trimester:** * **Propylthiouracil (PTU)** preferred * Lower teratogenicity vs. methimazole (MMI) * Dose: **50–150 mg TID** #### **Second & third trimesters:** * Switch to **Methimazole (MMI)** * Dose: **5–20 mg/day** ### **Drug information (ATDs)** #### **Propylthiouracil (PTU)** * **MOA:** inhibits TPO + peripheral T4→T3 conversion * **AE:** hepatotoxicity, rash, agranulocytosis * **Counselling:** Fever/sore throat → stop drug → urgent CBC. #### **Methimazole (MMI)** * **MOA:** inhibits TPO * **AE:** Aplasia cutis, choanal/esophageal atresia (1st trimester), cholestasis * **Monitoring:** FT4 every 4 weeks --- ### **2. Beta-blockers (Symptomatic control)** * **Propranolol 10–20 mg TID** short-term (2–6 weeks) * Avoid long-term due to fetal growth restriction. --- ### **3. Surgery** * Indications: * Drug intolerance * Large goiter * Very high TRAb * **Timing:** **Second trimester** --- # **5️⃣ POSTPARTUM THYROIDITIS** * Autoimmune inflammation after delivery * Phases: 1. Hyperthyroid (1–3 months) 2. Hypothyroid (4–6 months) 3. Recovery (1 year) ### Management * Hyperthyroid: **Beta-blockers** only * Hypothyroid: temporary **Levothyroxine** if symptomatic * Recurrence in future pregnancies: **70%** --- # **6️⃣ THYROID STORM IN PREGNANCY (EMERGENCY)**   ## **Features** * Fever, tachycardia, vomiting * Delirium, heart failure * Precipitated by labor, infection, surgery ## **Management Protocol** 1. **PTU 600–1000 mg loading dose**, then 200–300 mg Q6h 2. **Iodine solution** after 1 hour 3. **Propranolol** IV/oral 4. **Hydrocortisone 100 mg IV Q8h** 5. Treat precipitating cause 6. ICU care --- # **7️⃣ MONITORING SUMMARY** | Disorder | Follow-up | | ----------------------- | ---------------------------------------------------- | | Hypothyroidism | TSH every 4 weeks | | Hyperthyroidism on ATDs | FT4 every 4 weeks | | TRAb-positive Graves’ | TRAb at 24–28 weeks, fetal US for tachycardia/goiter | | Postpartum | Re-check thyroid at 6 weeks postpartum | --- # **8️⃣ FETAL SURVEILLANCE** * Fetal heart rate (tachycardia → hyperthyroid) * Fetal goiter on ultrasound * Growth assessment * Amniotic fluid volume * Doppler if growth restriction suspected --- # **9️⃣ KEY DIFFERENTIATION TABLE** | Condition | TSH | FT4 | TRAb | Treatment | | ----------- | --- | ------ | ------------ | ------------- | | Graves’ | ↓ | ↑ | ↑ | PTU → MMI | | GTT | ↓ | Mild ↑ | Normal | Supportive | | Hypothyroid | ↑ | ↓ | TPO+ | Levothyroxine | | Subclinical | ↑ | Normal | TPO variable | Treat if TPO+ | --- # **Would you like an SEO title, description, keywords, or an infographic for this topic?**
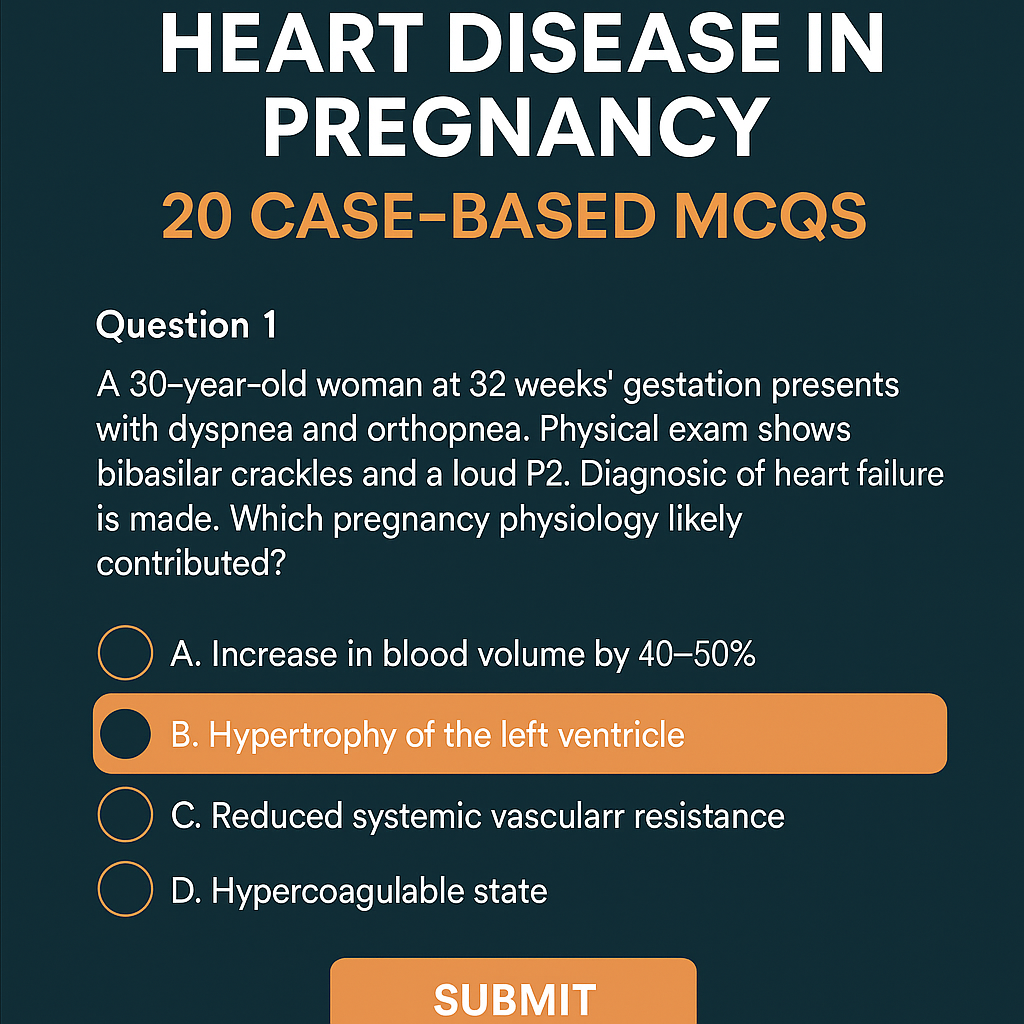
Heart Disease in Pregnancy: Causes, Risks, Management & 20 Case-Based MCQs (With Answers & Explanations)
Below is a **complete, exam-ready, concise-but-exhaustive reference** for **Heart Disease in Pregnancy** — covering definition, physiology, classification, clinical features, investigations, management (stepwise), drug details, labor/delivery planning, postpartum care, and contraindications. --- # **Heart Disease in Pregnancy – Complete Overview** ! --- ## **1. Definition** Heart disease in pregnancy refers to **pre-existing cardiac disorders** (congenital or acquired) or **pregnancy-induced cardiac dysfunction** (e.g., peripartum cardiomyopathy) that complicate pregnancy, labor, or postpartum period. --- ## **2. Why Pregnancy Worsens Heart Disease (Physiological Changes)** Pregnancy causes major hemodynamic changes that peak at **28–32 weeks**: * **↑ Blood volume by 40–50%** * **↑ Cardiac output by 30–50%** * **↑ Heart rate by 10–20 bpm** * **↓ Systemic vascular resistance** * **Hypercoagulable state** * **During labor:** CO ↑ 20–30% more * **Immediately postpartum:** Autotransfusion ↑ CO up to 80% These changes may **unmask latent heart disease** or **worsen existing cardiac failure**. --- ## **3. Types of Heart Diseases Seen in Pregnancy** ### **A. Congenital Heart Disease (CHD)** * Atrial septal defect (ASD) * Ventricular septal defect (VSD) * Patent ductus arteriosus (PDA) * Tetralogy of Fallot (repaired/unrepaired) * Eisenmenger syndrome (very high-risk) ### **B. Acquired Heart Disease** * Rheumatic heart disease * Mitral stenosis (most common serious lesion in pregnancy) * Mitral regurgitation * Aortic stenosis * Cardiomyopathies * **Peripartum cardiomyopathy** * Ischemic heart disease * Arrhythmias * Hypertensive heart disease --- ## **4. WHO Classification of Maternal Cardiovascular Risk** ### **WHO Class I – Low Risk** * Small ASD/VSD * PDA * Mitral valve prolapse * Successfully repaired simple CHD ### **WHO Class II – Moderate Risk** * Unrepaired ASD/VSD * Repaired TOF * Mild LV dysfunction ### **WHO Class III – High Risk** * Mechanical valves * Cyanotic congenital heart disease * Moderate LV dysfunction * Previous peripartum cardiomyopathy with normal EF now ### **WHO Class IV – Extremely High Risk (Pregnancy Contraindicated)** * **Pulmonary hypertension / Eisenmenger syndrome** * **Severe LV dysfunction (EF < 30%)** * **Severe mitral stenosis or aortic stenosis** * **Marfan syndrome with aorta > 45 mm** * **Previous peripartum cardiomyopathy with persistent dysfunction** --- ## **5. Clinical Features** ### **Symptoms** * Dyspnea (especially NYHA III–IV) * Orthopnea / PND * Fatigue * Palpitations * Chest pain * Syncope ### **Warning Features of Cardiac Decompensation** * Dyspnea at rest * Hemoptysis * Cyanosis * Loud P2 / RV heave * Basal crepitations * New arrhythmias --- ## **6. Investigations** ### **Basic** * CBC * ECG * **Echocardiography – Most important** * BNP (optional) ### **Advanced** * Cardiac MRI (safe without gadolinium) * Holter monitoring * Exercise testing (pre-pregnancy only) ### **Avoid** * CT angiography unless life-saving * ACE inhibitors / ARBs history to be checked --- ## **7. Complications** * **Maternal:** Heart failure, arrhythmias, thromboembolism, endocarditis, cardiac arrest * **Fetal:** IUGR, preterm birth, fetal hypoxia, congenital heart disease (3–5% risk) --- # **8. Management of Heart Disease in Pregnancy (Stepwise)**   --- ## **A. Preconception Counselling** * Risk assessment + WHO classification * Optimize cardiac status (e.g., balloon valvotomy for MS) * Stop teratogenic drugs (ACE inhibitors, ARBs, statins, warfarin if possible) --- ## **B. Antenatal Management** ### **1. Lifestyle** * Adequate rest * Left lateral position * Avoid anemia (treat aggressively) * Avoid excessive weight gain * Salt restriction if HF symptoms ### **2. Drugs Used** Below are the major drug classes **with indications, mechanism, dosing, adverse effects, contraindications, interactions, and counselling.** --- ## **i. Diuretics (Furosemide)** **Indication:** Heart failure, pulmonary edema **MOA:** Loop diuretic → inhibits Na-K-2Cl in loop of Henle **Dose:** 20–40 mg PO/IV, repeat as required **PK:** Rapid onset, renal excretion **AEs:** Hypokalemia, dehydration **Contra:** Severe electrolyte imbalance **Interactions:** Digoxin ↑ toxicity if hypokalemia **Counselling:** Monitor weight, urine output, electrolytes --- ## **ii. Beta-blockers (Metoprolol preferred)** **Indication:** Rate control, arrhythmias, ischemic heart disease **MOA:** Blocks β1 receptors → ↓ HR & contractility **Dose:** 25–100 mg/day **AEs:** IUGR (minimal), bradycardia **Contra:** Severe asthma **Interactions:** Calcium channel blockers → heart block risk **Counselling:** Do not stop suddenly --- ## **iii. Anticoagulants** ### **a. LMWH (Enoxaparin) – Preferred** **Indication:** Mechanical valves, AF, thromboembolism **MOA:** Enhances antithrombin III → inhibits Xa **Dose:** 1 mg/kg twice daily **Monitoring:** Anti-Xa levels **AEs:** Bleeding **Contra:** Active bleeding ### **b. Warfarin – Teratogenic (avoid 6–12 weeks)** Used only when valve thrombosis risk is very high. --- ## **iv. Vasodilators (Hydralazine, Nitrates)** **Indication:** HF with hypertension **AEs:** Headache, hypotension --- ## **v. Digoxin** **Indication:** HF with atrial fibrillation **MOA:** Na-K ATPase inhibition → ↑ Ca → ↑ contractility **Dose:** 0.125–0.25 mg daily **AEs:** Toxicity (nausea, vision changes) **Monitor:** Serum levels --- ## **Drugs Contraindicated in Pregnancy** * **ACE inhibitors / ARBs** → renal failure, skull defects * **Amiodarone** → fetal thyroid dysfunction * **Warfarin (first trimester)** unless essential * **Statins** --- ## **C. Follow-up Schedule** * Monthly (WHO I–II) * Fortnightly (WHO III) * Weekly (WHO IV — pregnancy discouraged) --- # **9. Labor and Delivery Management**   ### **Preferred Mode:** **Vaginal delivery with epidural anesthesia** ### **Indications for Caesarean Section** * Severe aortic stenosis * Marfan with aortic root dilation * Eisenmenger * Severe HF * Anticoagulation not stopped ### **Intrapartum Measures** * Continuous ECG + pulse oximetry * Avoid fluid overload * Slow, assisted second stage (forceps/vacuum) ### **Anesthesia** * Epidural preferred * Avoid general anesthesia (↑ cardiac stress) --- # **10. Postpartum Care** * Highest risk of heart failure in **first 24–72 hours** * Gradual mobilization * Restart anticoagulation after 6 hours (if needed) * Contraception counselling * **Avoid estrogen pills** * Prefer: IUCD, progestin-only methods --- # **11. High-Risk Specific Conditions** ## **A. Mitral Stenosis** * Most dangerous RHD lesion in pregnancy * Tachycardia → ↑ LA pressure → pulmonary edema * Management: β-blockers + diuretics * Balloon valvotomy if severe --- ## **B. Eisenmenger Syndrome** * **Pregnancy contraindicated (WHO IV)** * Maternal mortality 30–50% * No effective treatment → counselling for termination --- ## **C. Peripartum Cardiomyopathy** * Heart failure in last month of pregnancy or 5 months postpartum * EF < 45% * Treatment: * Diuretics * Beta-blockers * Bromocriptine (stops prolactin → improves function) * Avoid future pregnancy if EF not normalized --- # **12. Fetal Risks** * Prematurity * Growth restriction * Neonatal asphyxia * Congenital heart disease (if mother has CHD) --- # **13. Key Prevention Strategies** * Early diagnosis * Control anemia * Avoid excessive fluids * Use cardiac medications judiciously * Multidisciplinary care (obstetrician + cardiologist) --- # **Would you like a SEO-optimized title & description for this topic, or a high-ranking blog article version?**
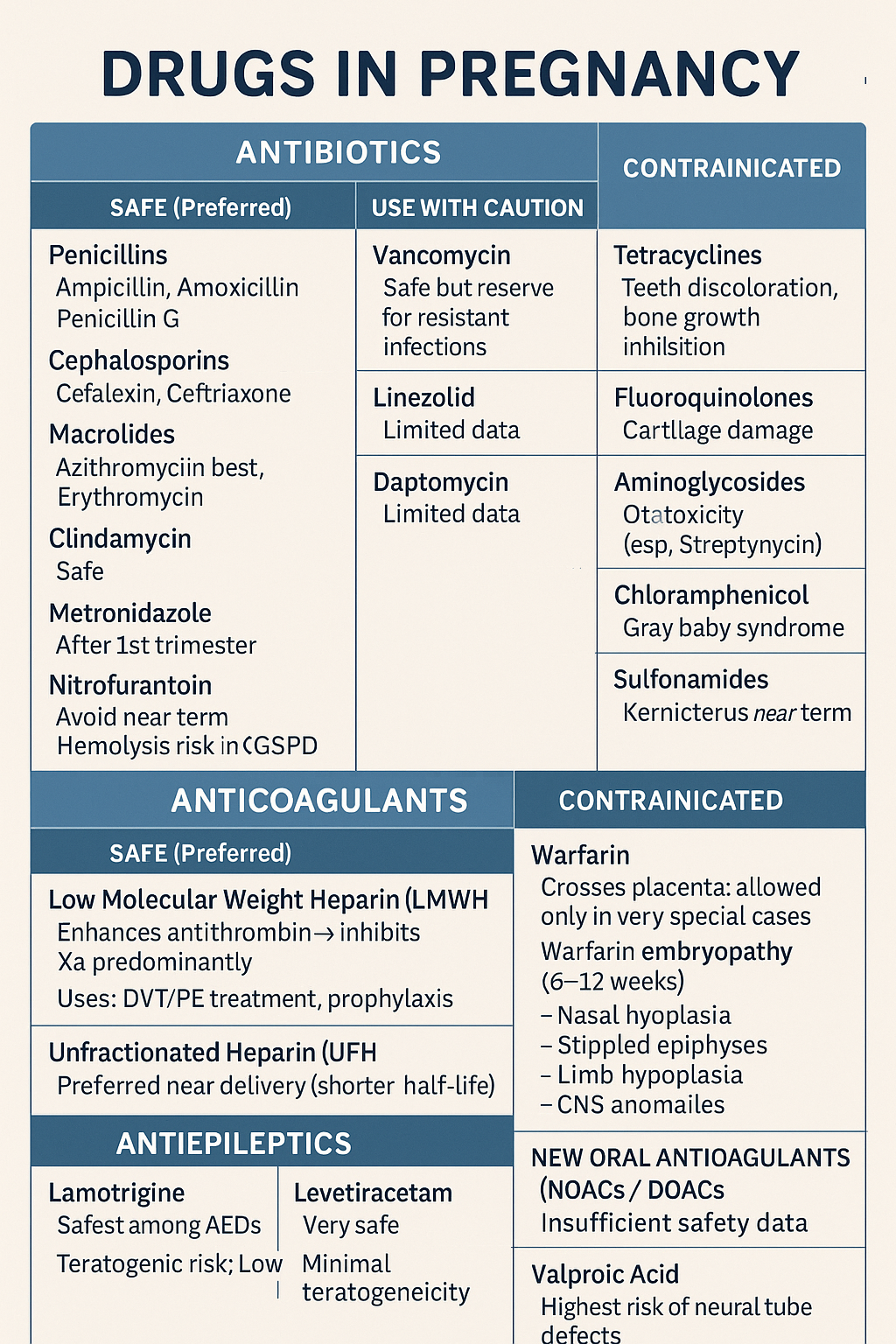
Comprehensive guide on safe and unsafe drugs in pregnancy including antibiotics, anticoagulants, and antiepileptics. Covers risks, teratogenicity, and clinical management
Below is a **concise but complete, exam-ready note** on **Drugs in Pregnancy – Antibiotics, Anticoagulants, Antiepileptics**. Structured for **quick revision + maximum coverage**. --- # ⭐ **DRUGS IN PREGNANCY – DETAILED NOTE (ANTIBIOTICS, ANTICOAGULANTS, ANTIEPILEPTICS)**    ## ✔ **SAFE (Preferred)** ### **Low Molecular Weight Heparin (LMWH)** * **Examples:** Enoxaparin, Dalteparin * **Mechanism:** Enhances antithrombin → inhibits **Xa** predominantly * **Does NOT cross placenta → safest anticoagulant** * **Uses:** DVT/PE treatment, prophylaxis, thrombophilia, APS * **Monitoring:** Anti-Xa levels in special cases (obesity, renal disease) ### **Unfractionated Heparin (UFH)** * Safe (does not cross placenta) * Preferred **near delivery** (shorter half-life, reversible with protamine) --- ## ❌ **CONTRAINDICATED** ### **Warfarin** * Crosses placenta → **warfarin embryopathy** (6–12 weeks): * Nasal hypoplasia * Stippled epiphyses * Limb hypoplasia * CNS anomalies * **Fetal hemorrhage** anytime * **Allowed only in very special cases:** mechanical heart valves when LMWH fails. --- ## ⚠ **NEW ORAL ANTICOAGULANTS (NOACs / DOACs)** Apixaban, Rivaroxaban, Dabigatran * **Avoid in pregnancy** → insufficient safety, crosses placenta --- # 3️⃣ **ANTIEPILEPTICS IN PREGNANCY**  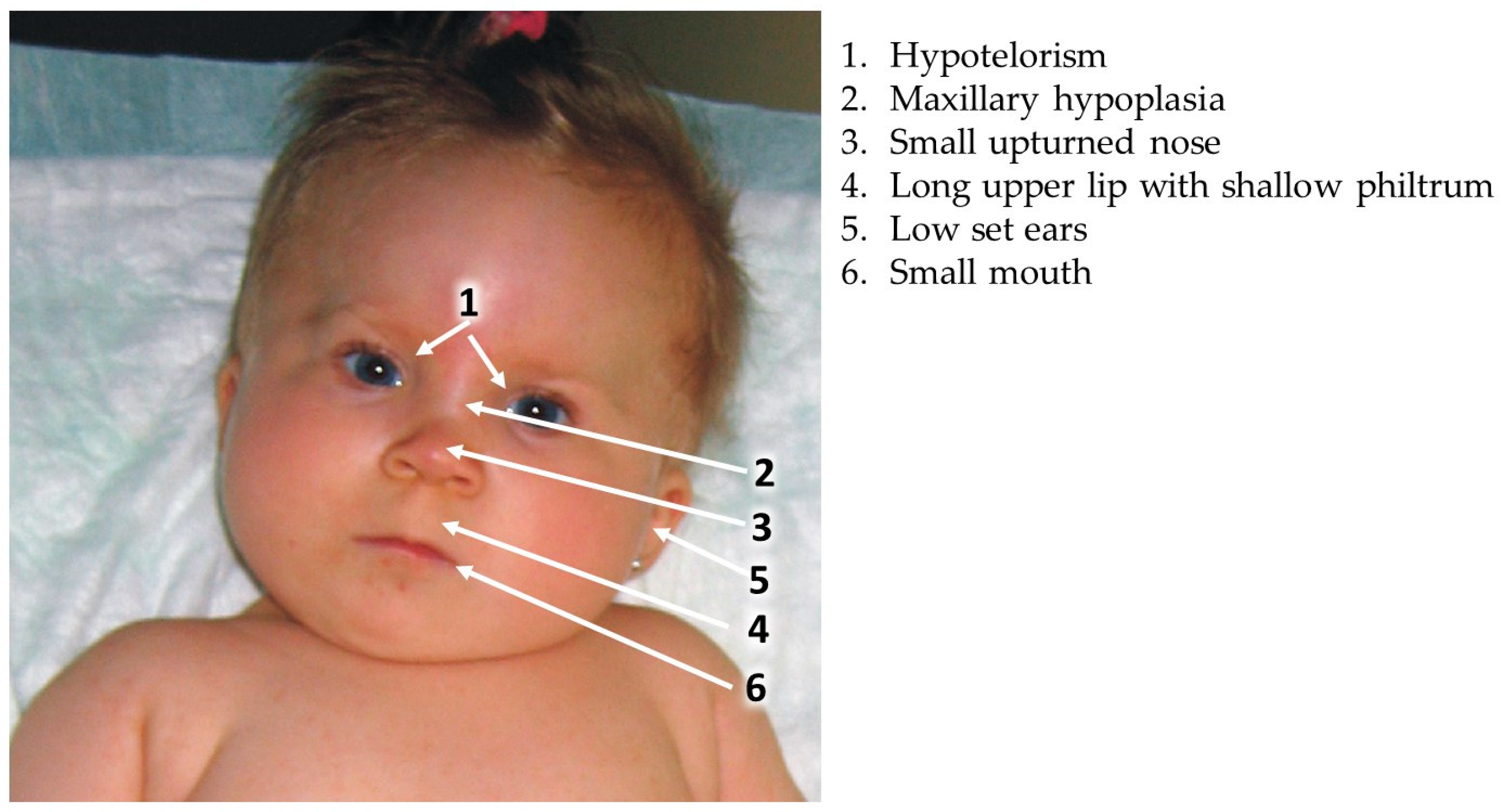   ## ⭐ **KEY PRINCIPLES** * Goal: **Seizure control** (maternal seizures are more harmful than drug risk) * Use **monotherapy** at **lowest effective dose** * Supplement **Folic acid 4–5 mg/day preconception → 1st trimester** * Check drug levels in pregnancy (pharmacokinetics change) --- ## ✔ **RELATIVELY SAFE ANTIEPILEPTICS (Preferred)** ### **1. Lamotrigine** * Safest among AEDs * **Teratogenic risk:** Low * **PK:** Increased clearance → dose adjustment needed * **Adverse:** Rash (SJS risk) ### **2. Levetiracetam** * Very safe * Minimal teratogenicity * Well-tolerated ### **3. Carbamazepine (with caution)** * Moderate teratogenic risk * Associated with **neural tube defects (NTD)** (~1%) * Give **high-dose folic acid** --- ## ⚠ **USE WITH CAUTION** | AED | Risk | | ----------------- | ---------------------------------------------------------------------- | | **Phenytoin** | Fetal hydantoin syndrome: growth delay, facial anomalies, limb defects | | **Topiramate** | Cleft lip/palate | | **Phenobarbital** | Cognitive defects, withdrawal | --- ## ❌ **AVOID / HIGHLY TERATOGENIC** ### **Valproic Acid** * **Highest risk of neural tube defects (5–10%)** * Cognitive impairment * Cardiac defects * Dose-dependent teratogenicity * **Avoid in pregnancy unless no alternative** --- # 4️⃣ **IMPORTANT COMPARISON TABLES** ## **A. Safe vs Unsafe Antibiotics** | Safe | Unsafe | | ------------------------------ | -------------------------- | | Penicillins | Tetracycline | | Cephalosporins | Fluoroquinolones | | Azithromycin | Aminoglycosides (ototoxic) | | Metronidazole (after 1st tri) | Chloramphenicol | | Nitrofurantoin (not near term) | Sulfonamides (near term) | --- ## **B. Safe vs Unsafe Anticoagulants** | Safe | Unsafe | | ---- | -------- | | LMWH | Warfarin | | UFH | NOACs | --- ## **C. Safe vs High-Risk Antiepileptics** | Safer | Moderate | High-risk | | ------------- | ------------- | ------------- | | Lamotrigine | Carbamazepine | Valproate | | Levetiracetam | Phenytoin | Phenobarbital | | — | Topiramate | — | --- # 5️⃣ **MANAGEMENT SUMMARY IN PREGNANCY** ### 🔹 **Infection** * Prefer beta-lactams * Avoid teratogenic antibiotics * Treat aggressively because **maternal sepsis harms fetus more** ### 🔹 **Thromboembolism** * **LMWH first-line** * Switch to UFH close to delivery * Avoid warfarin except mechanical valves requiring high-intensity anticoagulation ### 🔹 **Epilepsy** * Continue AEDs (never stop abruptly) * Choose **Lamotrigine or Levetiracetam** * Avoid **Valproate** * High-dose folic acid (4–5 mg/day) --- If you want, I can also generate: ✅ **25 MCQs (HTML/CSS/JS exam mode)** ✅ **Case scenarios with management** ✅ **SEO title + description + keywords** ✅ **Infographics / images for notes** Just tell me!
Complete guide on anaemia in pregnancy including causes, WHO definition, diagnosis, iron requirements, IFA tablets, NIAP, Anemia Mukt Bharat, treatment & management.
Great — I made **30 concise, high-yield case scenarios** on anaemia in pregnancy. Each case includes: brief history/exam, key labs, working diagnosis, immediate management, definitive treatment plan, and follow-up. I kept dosing and practical steps clear so you can paste these into teaching slides, case banks or clinical notes. --- # 30 Case Scenarios — Anaemia in Pregnancy (with management) > Legend: FS 325 mg ≈ 65 mg elemental Fe; typical oral treatment: **60–120 mg elemental Fe/day** (commonly 1 FS 325 mg once–three times daily depending on severity/tolerance). IV iron options: **iron sucrose** (commonly 100–200 mg per infusion repeated to calculated total) or **ferric carboxymaltose (FCM)** (single doses up to 750–1000 mg per product guidance). Transfusion generally considered for **Hb ≤7.0 g/dL** or symptomatic/hemodynamically unstable patient; tailor to obstetric context. --- ### Case 1 — Mild IDA, first trimester * Presentation: 24 y, G1P0, 10 wks, fatigue. Exam: pallor only. * Labs: Hb 10.2 g/dL, MCV 74 fL, ferritin 8 ng/mL, Mentzer >13. Smear: microcytic hypochromic. * Dx: Iron deficiency anaemia (mild). * Immediate mgmt: Start oral iron — **FS 325 mg once daily** (≈65 mg elemental) + folic acid 400 µg; counsel on absorption and side effects. * Definitive plan: Check Hb at 4 weeks; if Hb rising by ~1 g/dL, continue 3 months after normalization to replete stores. Diet & deworm if indicated. --- ### Case 2 — Moderate IDA, second trimester, poor diet * Presentation: 29 y, 20 wks, progressive exertional dyspnea. * Labs: Hb 8.3 g/dL, MCV 68 fL, ferritin 9 ng/mL. * Dx: Moderate IDA. * Immediate mgmt: Oral iron **FS 325 mg twice daily** (≈130 mg elemental/day) + folic acid; start vitamin C with dose. Consider adherence issues. * Definitive plan: Reassess Hb in 2–3 weeks. If poor response or intolerance → switch to IV iron (calculate total deficit; consider FCM 1000 mg single or iron sucrose series). --- ### Case 3 — Severe symptomatic anaemia late pregnancy * Presentation: 31 y, 36 wks, chest tightness, syncope history. Exam: tachycardia, low BP. * Labs: Hb 5.8 g/dL, MCV 75 fL, ferritin 5 ng/mL. * Dx: Severe IDA with hemodynamic compromise. * Immediate mgmt: Resuscitate (IV fluids as needed), **blood transfusion** (matched PRBCs) — aim to stabilise; crossmatch and transfuse per obstetric transfusion protocol. * Definitive plan: After stabilization, give IV iron (iron sucrose/FCM) to replete stores; counsel for delivery planning and postpartum follow-up. --- ### Case 4 — Late presentation, intolerance to oral iron * Presentation: 26 y, 34 wks, vomiting with oral iron causing severe nausea. * Labs: Hb 9.0 g/dL, ferritin 10 ng/mL. * Dx: IDA with oral intolerance. * Immediate mgmt: Stop oral iron; offer **IV iron** (iron sucrose series or FCM depending on availability) to correct quickly pre-delivery. Monitor vitals during infusion. * Follow-up: Hb/ferritin 2–4 weeks post-infusion; resume oral prophylaxis postpartum. --- ### Case 5 — Refractory anaemia despite oral iron * Presentation: 28 y, 22 wks, on FS 325 mg TID x 6 weeks, minimal Hb rise. * Labs: Hb 9.2 g/dL, ferritin 6 ng/mL, reticulocyte low-normal. * Dx: Non-response to oral iron (malabsorption, non-adherence, ongoing loss). * Immediate mgmt: Evaluate adherence, check for parasites/GI blood loss. If adherence OK → **IV iron**. Consider stool testing for hookworm. Screen for celiac if suspicion. * Definitive plan: Treat underlying cause; calculate iron deficit and give IV iron. --- ### Case 6 — Microcytosis suspicious for thalassaemia trait * Presentation: 21 y, 12 wks, mild pallor. Labs: Hb 10.8 g/dL, MCV 65 fL, RBC count high, Mentzer <13, ferritin normal 50 ng/mL. * Dx: Likely β-thalassaemia trait. * Mgmt: Confirm with **Hb electrophoresis (elevated HbA₂)**. Do **not** give high-dose iron if ferritin normal. Genetic counselling and partner screening. Provide routine antenatal care; avoid unnecessary iron. --- ### Case 7 — Anaemia of chronic disease (ACD) * Presentation: 34 y, known lupus, 28 wks, fatigue. Labs: Hb 9.6 g/dL, ferritin 180 ng/mL, low serum iron, low TIBC. CRP high. * Dx: ACD due to chronic inflammation. * Mgmt: Treat underlying disease flare; iron supplementation only if true iron deficiency coexists (assess transferrin saturation). Consider erythropoiesis-stimulating agents only in specialist settings; consult rheumatology/hematology. --- ### Case 8 — Folate deficiency plus iron deficiency * Presentation: 30 y, 18 wks, glossitis, neural tube risk concern. Labs: Hb 9.4 g/dL, MCV 102 fL, low folate. Smear: macro-ovalocytes. Ferritin low-normal. * Dx: Mixed folate deficiency ± iron deficiency. * Mgmt: Start **folic acid 5 mg daily** (treatment dose) + oral iron (if ferritin low). Investigate diet, malabsorption. Reassess CBC after 2–4 weeks. --- ### Case 9 — B12 deficiency in pregnancy * Presentation: 27 y, 24 wks, paresthesia, macrocytic indices. Labs: Hb 8.9 g/dL, MCV 108 fL, low B12. * Dx: B12 deficiency. * Mgmt: **IM/SC cyanocobalamin** replacement (e.g., 1000 µg IM weekly × several doses then monthly) depending on cause; treat concurrently with folate if needed. Neurologic signs may take months to improve. --- ### Case 10 — Postpartum haemorrhage with acute blood loss * Presentation: 35 y, day 1 postpartum after PPH, tachycardic, Hb 6.1 g/dL. * Dx: Acute severe anaemia from blood loss. * Mgmt: Immediate resuscitation; **urgent transfusion** (PRBCs), manage bleeding source (surgical/medical). After stabilization consider IV iron for repletion. --- ### Case 11 — Twin pregnancy with increased iron need * Presentation: 32 y, twin gestation 28 wks, fatigue. Labs: Hb 9.0 g/dL, ferritin 12 ng/mL. * Dx: IDA in multiple pregnancy. * Mgmt: Start **oral iron** at treatment dose (FS 325 mg twice daily) and consider early IV iron if inadequate response or near-term to optimize Hb before delivery. Close monitoring. --- ### Case 12 — Hyperemesis gravidarum causing iron deficiency * Presentation: 22 y, 10 wks, severe vomiting; poor intake. Labs: Hb 9.8 g/dL, ferritin 15 ng/mL. * Dx: IDA from poor intake. * Mgmt: Correct dehydration, antiemetics + start **oral iron** when tolerated (consider IV iron if vomiting prevents oral intake). Nutritional support and folate. --- ### Case 13 — Hookworm infection causing chronic blood loss * Presentation: 25 y, 26 wks, pica, eosinophilia. Labs: Hb 8.7 g/dL, ferritin 7 ng/mL. Stool: ova consistent with hookworm. * Dx: IDA due to helminthiasis. * Mgmt: Treat hookworm per local protocol (deworming timing per antenatal policy; e.g., single-dose albendazole often after first trimester in many settings), start oral iron or IV iron if severe; public-health measures. --- ### Case 14 — Malaria-associated anaemia in pregnancy * Presentation: 28 y, febrile 30 wks, pallor, splenomegaly. Labs: Hb 7.9 g/dL, smear positive for Plasmodium. * Dx: Malaria-related anaemia. * Mgmt: Treat malaria urgently with pregnancy-safe antimalarial per local guideline; transfuse if severe/symptomatic; start iron only after clearing infection and per clinician judgment. --- ### Case 15 — HIV with anaemia of multifactorial cause * Presentation: 29 y, known HIV on ART, 20 wks, fatigue. Labs: Hb 9.0 g/dL, ferritin 90 ng/mL, MCV variable. * Dx: Multifactorial (ACD, drug-related, nutritional). * Mgmt: Review ART (e.g., zidovudine can cause anaemia), treat nutritional deficiencies, consider IV iron if IDA confirmed and oral therapy fails; coordinate with HIV care. --- ### Case 16 — Renal disease with anemia in pregnancy * Presentation: 36 y, CKD stage 3, 24 wks, low energy. Labs: Hb 8.6 g/dL, ferritin 150 ng/mL, low reticulocyte. * Dx: Anaemia of CKD/ACD. * Mgmt: Nephrology consult; consider IV iron if iron-deficient; consider erythropoiesis stimulating agents in specialist setting; optimise dialysis/renal care. --- ### Case 17 — Recurrent anemia after oral iron completion * Presentation: 27 y, previously treated IDA, returns 3 months postpartum with Hb 9.5 g/dL. Ferritin low 12 ng/mL. * Dx: Recurrent iron deficiency. * Mgmt: Reassess for ongoing bleeding; restart iron therapy; investigate heavy menstrual bleeding; counsel on compliance and diet; consider long-term iron strategy until cause fixed. --- ### Case 18 — Anaemia with allergic reaction to IV iron history * Presentation: 30 y, history of anaphylaxis to IV iron dextran. Now 30 wks, Hb 7.5 g/dL. * Dx: Severe IDA with prior IV iron allergy. * Mgmt: Avoid offending agent; use non-dextran formulations (iron sucrose or FCM) under monitored conditions with resuscitation available; consider transfusion if urgent and risk high. --- ### Case 19 — Mixed thalassaemia trait + iron deficiency * Presentation: 23 y, MCV 68 fL, Mentzer borderline, ferritin low 10 ng/mL. * Dx: Mixed iron deficiency + thalassaemia trait. * Mgmt: Treat iron deficiency (oral/IV as needed) — correct iron first and reassess indices; refer to hematology/genetic counselling for thalassaemia. --- ### Case 20 — Severe anaemia with cardiac compromise * Presentation: 38 y, 34 wks, signs of high-output cardiac failure (orthopnea), Hb 6.5 g/dL. * Dx: Severe anaemia causing cardiac strain. * Mgmt: Urgent transfusion and cardiac support; plan delivery in appropriate setting once stabilized; consider IV iron after haemodynamic stability. --- ### Case 21 — Antenatal screening finds microcytic anaemia in partner/partner screening scenario * Presentation: 26 y, first visit, Hb 11.1 g/dL but MCV 72 fL. Ferritin 40 ng/mL. RBC count high. Mentor index <13. * Dx: Possible thalassaemia trait carrier. * Mgmt: Do Hb electrophoresis; if positive, offer partner testing and genetic counselling; avoid unnecessary iron if iron stores adequate. --- ### Case 22 — Severe anaemia in adolescent pregnant patient * Presentation: 17 y, 18 wks, symptomatic, Hb 7.2 g/dL. * Dx: Severe IDA. * Mgmt: Consider transfusion if symptomatic; otherwise start IV iron if available; add nutritional counselling, address social determinants (poverty/diet), involve adolescent health services. --- ### Case 23 — Anaemia discovered during labour * Presentation: 30 y, in labor, known Hb 8.0 g/dL on admission. * Dx: Moderate IDA at delivery. * Mgmt: Plan for blood availability if bleeding risk high; give IV iron postpartum if Hb fails to improve and prolonged recovery expected; active management of third stage of labour to avoid PPH. --- ### Case 24 — Severe IDA with late booking and need for rapid correction before c-section * Presentation: 33 y, booked at 38 wks, Hb 8.0 g/dL, scheduled c-section next week. * Dx: IDA needing rapid optimization. * Mgmt: Give **IV iron (FCM 1000 mg if available)** to increase Hb/iron stores quickly pre-op; if immediate correction required and Hb very low → transfuse perioperatively. --- ### Case 25 — Anaemia in pregnancy with concurrent sepsis * Presentation: 29 y, fever, Hb 8.4 g/dL, high CRP. * Dx: Anaemia with infective/inflammatory component. * Mgmt: Treat infection promptly; avoid confounding ferritin interpretation; if iron deficiency coexists and severe → consider IV iron once infection controlled; transfuse if hemodynamically unstable. --- ### Case 26 — Peripartum transfusion reaction risk scenario * Presentation: 35 y, urgent PPH, requires transfusion; prior transfusion history with antibodies. * Dx: Acute blood loss anaemia with alloimmunisation risk. * Mgmt: Coordinate blood bank for phenotype-matched units; transfuse as required; consider tranexamic acid and uterotonics; document antibody and counsel for future pregnancies. --- ### Case 27 — Anaemia with hemolysis (autoimmune) * Presentation: 31 y, jaundice, Hb 7.6 g/dL, elevated LDH, indirect bilirubin, positive direct Coombs. * Dx: Autoimmune hemolytic anemia (AIHA) in pregnancy. * Mgmt: Hematology consult; treat (corticosteroids first-line), transfusion if needed (with crossmatch); avoid IV iron while active hemolysis unless iron deficient; monitor fetus for hydrops if severe. --- ### Case 28 — Iron overload concern (hemochromatosis suspicion) * Presentation: 34 y, elevated ferritin 500 ng/mL, high transferrin saturation, mild anemia. Family history of hemochromatosis. * Dx: Possible iron overload or inflammation. * Mgmt: Evaluate for hereditary hemochromatosis outside pregnancy (genetic testing, specialist input); avoid unnecessary iron; treat underlying cause of high ferritin (inflammation vs overload). --- ### Case 29 — Antenatal prophylaxis non-adherence with borderline anaemia * Presentation: 28 y, missed many ANC visits, Hb 10.6 g/dL, ferritin 22 ng/mL. * Dx: Borderline anemia/early IDA. * Mgmt: Reinforce routine prophylaxis (30–60 mg elemental iron + folic acid), provide education, address barriers (side effects, access), recheck Hb in 4 weeks and treat if progresses. --- ### Case 30 — Severe postpartum anaemia with breastfeeding * Presentation: 27 y, 2 weeks postpartum, Hb 6.8 g/dL, symptomatic (dizziness), breastfeeding. * Dx: Severe postpartum anaemia (likely iron deficient). * Mgmt: Consider transfusion if symptomatic/severe; give IV iron if breastfeeding and stable (IV iron safe in lactation); if oral is chosen, counsel on adherence and side effects; follow-up Hb and ferritin, continue iron 3 months after repletion. --- # Quick management reminders (pasteable) * **Screening**: Hb at booking and at 28 wks. * **Oral iron**: FS 325 mg ≈ 65 mg elemental; treatment = **60–120 mg elemental/day** until stores replete. Take on empty stomach with vitamin C; separate from antacids. * **IV iron**: Use for intolerance, non-response, late pregnancy needing rapid correction, malabsorption, or severe anaemia when oral not feasible. Iron sucrose (100–200 mg per dose) or FCM (single large dose 750–1000 mg). Monitor for reactions. * **Transfusion**: Individualise. Usually **Hb ≤7.0 g/dL** or symptomatic/hemodynamic compromise → transfuse. In obstetrics, clinical scenario dictates threshold. * **Follow-up**: Check Hb 2–4 weeks after therapy start and continue iron for 3 months after normalization. --- If you want, I can now: * Convert these into a **printable PDF** or a **spreadsheet** for easy use; * Expand any selected cases into **full exam-style long cases** (history prompts, viva questions, stepwise management) or **MCQs** derived from these cases; * Produce the **25 MCQs in stylish exam mode** (single HTML file with CSS/JS) instead — tell me which format you prefer next and I’ll produce it immediately. # Anaemia in pregnancy — complete, stylish clinical note > Compact, exam-friendly, evidence-backed reference you can paste into notes or teaching slides. Sources for the most important guideline facts are cited inline. --- ## 1) Definition (WHO) Anaemia = low haemoglobin (Hb) or red-cell mass causing reduced O₂-carrying capacity. **WHO threshold in pregnancy:** **Hb < 110 g/L (11.0 g/dL)** = anaemia; **severe** = **< 70 g/L (7.0 g/dL)**. ([World Health Organization][1]) --- ## 2) Pathophysiology (short) * Pregnancy → plasma volume ↑ ≈ 30–50% while red-cell mass ↑ less → physiologic haemodilution (lower Hb). * Pathologic anaemia results when iron supply (diet + stores) cannot meet increased maternal/fetal demands → reduced haemoglobin synthesis → microcytic hypochromic RBCs (longstanding). * Other mechanisms: haemoglobinopathy, folate/B12 deficiency, chronic inflammation (anemia of chronic disease, ACD), hemolysis, acute blood loss. --- ## 3) Iron requirements in pregnancy & prophylaxis (practical) * Pregnancy increases iron need substantially (for maternal RBC mass, placenta and fetus). Guidelines recommend **daily oral iron 30–60 mg elemental iron + 400 µg folic acid** for routine antenatal prophylaxis (start early, usually from 12 weeks or at first contact per local policy). For treatment, higher elemental doses are used (see below). ([World Health Organization][2]) --- ## 4) Public-health: Anemia Mukt Bharat & IFA logistics (India) * **Anemia Mukt Bharat (NHM)** emphasises six strategic actions including IFA supplementation, deworming, food fortification, testing & treatment, behaviour change and special management of severe cases. Weekly IFA formulations for adolescents/adults vary by group (e.g., 45–60 mg elemental iron + folic acid 400–500 µg for weekly program tablets); pregnant women receive daily IFA through ANC (tablet composition and supply per NHM/ANC). ([National Health Mission][3]) > Note about **“I-NIAP”**: I searched for a standard term “I-NIAP” and could not find an established definition. In obstetric literature you’ll see **AIP / NAIP** (Anemia In Pregnancy / Non-Anemic In Pregnancy) used in studies. If you meant a specific program/term, tell me and I’ll fetch it. ([sid.ir][4]) --- ## 5) Clinical history (what to ask) * Symptoms: fatigue, exertional dyspnoea, palpitations, syncope, orthopea, pica (pagophagia), restless legs, diminished exercise tolerance. * Obstetric: prior PPH, multiple pregnancies, short interpregnancy interval, hyperemesis, dietary restrictions, bleeding (menorrhagia pre-pregnancy), parasites, recent infections. * Drugs: antacids, calcium, tetracyclines (interfere with iron). * Family history: haemoglobinopathies (thalassaemia trait). --- ## 6) Physical examination (key findings) * Pallor (conjunctiva, palmar crease), tachycardia, glossitis, koilonychia (severe chronic), systolic flow murmur, signs of heart failure if severe. Look for hepatosplenomegaly (hemolysis/thalassaemia), lymphadenopathy (chronic disease). --- ## 7) Investigations — how to approach & interpretation **First-line tests** * CBC with RBC indices (Hb, Hct, MCV, MCH, MCHC), reticulocyte count, peripheral smear. * Ferritin (best single test for iron stores unless inflammation present), serum iron, TIBC/transferrin, transferrin saturation. ([MSD Manuals][5]) **Key numbers** * **MCV normal** ≈ 80–100 fL (microcytic <80 fL). (Use lab reference ranges.) ([MSD Manuals][5]) **Mentzer index** (practical discriminator) * **Mentzer = MCV (fL) / RBC count (10^6/µL)**. * **>13 → likely Iron Deficiency Anaemia (IDA)**. * **<13 → likely β-thalassaemia trait**. ([PMC][6]) **Peripheral smear** * IDA: microcytic hypochromic RBCs, anisopoikilocytosis, pencil cells. * ACD: often normocytic or mildly microcytic with low serum iron but low TIBC. Ferritin is normal or high in ACD (acute phase reactant). **Hb electrophoresis** * Indication: to detect β-thalassaemia trait or other hemoglobinopathies when indices suggest trait (normal/high RBC count, low MCV, Mentzer <13). Confirm with HbA₂ levels. ([PMC][7]) **Ferritin interpretation** * Low ferritin confirms iron deficiency; ferritin is raised in inflammation — interpret with CRP/ESR. WHO/technical guidance gives ferritin cutoffs and handling when inflammation present. ([World Health Organization][8]) --- ## 8) IDA vs Anaemia of Chronic Disease (ACD) — key contrasts * **IDA:** low ferritin, low serum iron, high TIBC (or normal), low transferrin saturation; microcytic hypochromic RBCs. * **ACD:** low serum iron, **low/normal TIBC**, normal/high ferritin, low transferrin saturation; usually occurs with infection/inflammation/chronic disease. Treatment targets underlying disease + careful iron management. ([World Health Organization][8]) --- ## 9) Differential diagnoses to consider * Iron deficiency, haemoglobinopathies (thalassaemia trait), folate/B12 deficiency, ACD, hemolytic anaemias, blood loss (antepartum/PPH), bone marrow disorders. --- ## 10) Complications & adverse effects of anaemia in pregnancy **Maternal effects** * Fatigue, reduced work capacity, increased risk of cardiac failure if severe, increased risk of peripartum transfusion and infection, poor wound healing, higher maternal mortality in severe anaemia. ([World Health Organization][9]) **Fetal/neonatal effects** * Preterm birth, low birth weight, intrauterine growth restriction, perinatal mortality, impaired neurodevelopment if severe/untreated. --- ## 11) Management — overview (prevention → treat → rescue) **Goals:** correct Hb, replete iron stores (ferritin), prevent recurrence, avoid transfusion when possible. ### A. Prevention (policy/antenatal) * Diet counselling (iron-rich foods + vitamin C to increase absorption; avoid tea/coffee with meals). * Routine **daily IFA prophylaxis: 30–60 mg elemental iron + 400 µg folic acid** (WHO). For national programs (India) follow Anemia Mukt Bharat / ANC protocols for supply and deworming. ([World Health Organization][2]) ### B. Oral iron — first-line for mild–moderate IDA and prophylaxis **Common salts & elemental iron content (practical)** * **Ferrous sulfate 325 mg** ≈ **65 mg elemental iron** (varies with hydrate). * **Ferrous fumarate 300 mg** ≈ **99–100 mg elemental iron**. * **Ferrous gluconate 300/325 mg** ≈ **35–39 mg elemental iron**. (Check product label.) ([NCBI][10]) **Indication (pregnancy):** treatment when IDA confirmed (mild–moderate), prophylaxis as above. **Dosing (typical)** * **Prophylaxis:** 30–60 mg elemental iron daily + 400 µg folic acid. ([World Health Organization][2]) * **Treatment (common practice):** many formularies use **60–120 mg elemental iron daily** (often given as 1 tab of ferrous sulfate 325 mg × 1–3 daily depending on severity) or **single daily higher elemental dose**; some guidelines/recent studies favour **lower daily doses (e.g., 60–80 mg elemental once daily)** or alternate-day dosing to improve tolerance and absorption — tailor to local guidance and tolerance. ([ScienceDirect][11]) **Mechanism of action:** provides elemental iron for haemoglobin synthesis; absorbed in duodenum via DMT1 after reduction to ferrous form. **Pharmacokinetics (summary):** oral iron variably absorbed (5–30% depending on iron status, enhancers/inhibitors). Food reduces absorption; vitamin C enhances. **Adverse effects (oral):** GI upset, nausea, abdominal pain, constipation or diarrhoea, black stools; adherence often limited by GI side effects. ([National Health Mission][12]) **Contraindications:** known hypersensitivity; caution with hemochromatosis. Check for haemoglobinopathy before prolonged high-dose therapy. **Key interactions:** antacids, calcium, tetracyclines, some antibiotics — separate dosing by 2–3 hours. Vitamin C coadministration improves absorption. **Monitoring:** Hb every 2–4 weeks until rise (aim Hb ↑ by ~1 g/dL in 2–4 weeks), ferritin at baseline and after repletion; monitor adherence and GI side effects. **Counselling points to patient:** take on empty stomach if tolerated (or with small vitamin-C-rich juice), avoid tea/coffee within 1–2 hours, black stools are common and harmless, constipation can be managed with stool softener/diet. Keep out of reach of children (ingestion is toxic). --- ### C. Parenteral (IV) iron — when to use **Indications in pregnancy** * Severe IDA not corrected by oral iron, intolerance or non-adherence to oral iron, late pregnancy where rapid correction needed, malabsorption, ongoing significant bleeding, or when quick Hb rise needed before delivery/cesarean. Avoid routine use in first trimester when possible. ([Wiley Online Library][13]) **Preparations & dosing (practical)** * **Iron sucrose (Venofer):** repeated doses (e.g., 100–200 mg per infusion; typical cumulative calculated by Ganzoni or dosing tables). Max ~200 mg per infusion commonly used; total depends on deficit. ([transfusionguidelines.org][14]) * **Ferric carboxymaltose (FCM; Injectafer/Ferinject):** allows **larger single doses (up to ~750–1000 mg per infusion, product-specific limits ~15–20 mg/kg, max 1000 mg single dose)** — useful to correct iron deficit quickly in 1–2 visits. ([injectaferhcp.com][15]) **Mechanism:** IV complexes deliver iron directly to reticuloendothelial system for incorporation into ferritin/haemoglobin. **Adverse effects (IV):** infusion reactions (including rare anaphylaxis with older dextran formulations), transient hypotension, nausea, arthralgia, local irritation; hypophosphatemia reported with some agents (e.g., FCM). Monitor for hypersensitivity during infusion. ([PMC][16]) **Monitoring:** vitals during infusion, monitor Hb/ferritin 2–4 weeks post infusion; check phosphate if using FCM and high cumulative dose. **Counselling:** explain need for IV access, possible transient side effects, and post-infusion monitoring. --- ### D. Blood transfusion — when & how (obstetric specifics) **Indications:** individualised — combine clinical state and Hb level. Many guidelines say transfusion is usual when **Hb < 60–70 g/L** or if symptomatic/hemodynamically unstable; rarely needed if Hb > 100 g/L. In obstetrics, clinical context (ongoing bleeding, cardiovascular compromise, labour) is decisive. Cross-match and plan ahead for high-risk women. Use single donor PRBCs, match Rh/K testing, and consider component therapy. ([RCOG][17]) **Risks:** transfusion reactions, alloimmunisation, infection risk (low with modern screening), transfusion-associated circulatory overload; plan restrictive transfusion strategy where safe. --- ## 12) Stepwise treatment algorithm (practical summary) 1. **Screen all pregnant women at booking** (Hb + RBC indices). If Hb <110 g/L → further tests (CBC, ferritin ± iron studies). ([World Health Organization][1]) 2. **If IDA confirmed (low ferritin):** start/optimise oral iron (elemental 60–120 mg/day, adjust to tolerance). Counsel. Monitor Hb rise at 2–4 weeks. If inadequate response or very late pregnancy / urgent correction required → **IV iron** (calculate total deficit; consider FCM or iron sucrose per availability). ([ScienceDirect][11]) 3. **If severe symptomatic anaemia (Hb <70 g/L) or haemodynamic instability:** consider blood transfusion (obstetric judgement). ([RCOG][17]) --- ## 13) Prevention of recurrence & antenatal program tips * Give full course until 3 months postpartum if previously anaemic, ensure deworming (in areas endemic for helminths) per national policy, ensure adequate dietary counselling, consider screening for haemoglobinopathies if family history or persistent microcytosis after iron repletion. Use Anemia Mukt Bharat operational modules to plan community IFA distribution and counselling. ([i4n.in][18]) --- ## 14) Quick bedside pocket facts (copy-paste) * **WHO anaemia in pregnancy:** Hb <11.0 g/dL. ([World Health Organization][1]) * **Routine prophylaxis:** **30–60 mg elemental iron + 400 µg folic acid daily.** ([World Health Organization][2]) * **Oral elemental iron examples:** ferrous sulfate 325 mg ≈ 65 mg Fe; ferrous fumarate 300 mg ≈ 99 mg Fe; ferrous gluconate 300 mg ≈ 35 mg Fe. ([NCBI][10]) * **Mentzer index:** MCV/RBC; **>13 → IDA**, **<13 → thalassaemia trait**. ([PMC][6]) --- ## 15) Practical templates (for your notes) **A. ANC counselling line:** “You have mild iron deficiency. I’m starting oral iron (example: ferrous sulfate 325 mg **once daily** = ~65 mg elemental iron) + folic acid — take on empty stomach or with orange juice, expect black stools; call if severe abdominal pain or fainting.” **B. IV iron note:** “Given poor response/intolerance to oral iron or late pregnancy, plan IV ferric carboxymaltose **(calculate total deficit; often one 1000 mg infusion)** — monitor vitals during infusion, check Hb & ferritin at 2–4 weeks.” --- ## 16) References / further reading (selected, guideline-level) * WHO Anaemia fact sheet & Hb thresholds. ([World Health Organization][9]) * WHO recommendations: daily iron & folic acid supplementation in pregnancy. ([World Health Organization][2]) * Anemia Mukt Bharat training & operational guidance (India/NHM). ([National Health Mission][3]) * Mentzer index & RBC indices literature. ([PMC][6]) * IV iron reviews & product dosing (iron sucrose, ferric carboxymaltose) and obstetric use. ([PMC][16]) * RCOG / Green-top on blood transfusion in obstetrics. ([RCOG][17]) --- If you want, I can now: * Convert this into a **stylish one-page printable handout (PDF)**; * Generate **30 case scenarios with management** (you previously asked for many cases) or **25 MCQs in exam mode** with HTML/CSS/JS; * Produce an **SEO title/description/keywords** and **an illustrative image** (I can generate an image for a teaching slide). Tell me which follow-up you want and I’ll produce it in the same detailed style. [1]: https://cdn.who.int/media/docs/default-source/anaemia-in-women-and-children/hb-methods-for-gather.pdf?sfvrsn=da0fbb5f_11&utm_source=chatgpt.com "WHO methods and data sources for mean haemoglobin ..." [2]: https://www.who.int/tools/elena/interventions/daily-iron-pregnancy?utm_source=chatgpt.com "Daily iron and folic acid supplementation during pregnancy" [3]: https://nhm.gov.in/index1.php?lang=1&level=3&lid=797&sublinkid=1448&utm_source=chatgpt.com "Anaemia Mukt Bharat" [4]: https://www.sid.ir/paper/1056249/en?utm_source=chatgpt.com "Haemoglobin Level of Pregnant Women on First ..." [5]: https://www.msdmanuals.com/professional/multimedia/table/typical-normal-serum-values-for-iron-iron-binding-capacity-ferritin-and-transferrin-saturation?utm_source=chatgpt.com "Table: Typical Normal Serum Values for Iron, Iron-Binding ..." [6]: https://pmc.ncbi.nlm.nih.gov/articles/PMC9121960/?utm_source=chatgpt.com "Role of Mentzer index for differentiating iron deficiency ..." [7]: https://pmc.ncbi.nlm.nih.gov/articles/PMC5467296/?utm_source=chatgpt.com "Iron Deficiency Anemia or β-Thalassemia Trait? - PMC" [8]: https://www.who.int/docs/default-source/micronutrients/ferritin-guideline/ferritin-guidelines-brochure.pdf?sfvrsn=76a71b5a_4&utm_source=chatgpt.com "ferritin-guidelines-brochure.pdf" [9]: https://www.who.int/news-room/fact-sheets/detail/anaemia?utm_source=chatgpt.com "Anaemia" [10]: https://www.ncbi.nlm.nih.gov/books/NBK548214/table/Iron.T1/?utm_source=chatgpt.com "[Table, Concentrations of elemental iron in typical iron tablets]" [11]: https://www.sciencedirect.com/science/article/pii/S0098299720300364?utm_source=chatgpt.com "Oral iron supplementation in iron-deficient women" [12]: https://nhm.gov.in/images/pdf/programmes/wifs/guidelines/icds_operational_guidelines_for_wifs.pdf?utm_source=chatgpt.com "Operational Guidelines for Weekly IFA Supplementation ..." [13]: https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.27220?utm_source=chatgpt.com "Expert consensus guidelines: Intravenous iron uses, ..." [14]: https://www.transfusionguidelines.org/document-library/documents/protocol-for-the-use-of-iv-iron-sucrose/download-file/rtc-eeng_protocol_iv_iron_sucrose.pdf?utm_source=chatgpt.com "IV iron sucrose Venofer protocol v1.0 Jan08" [15]: https://injectaferhcp.com/iron-injection-administration?utm_source=chatgpt.com "Dosing and Administration" [16]: https://pmc.ncbi.nlm.nih.gov/articles/PMC9722303/?utm_source=chatgpt.com "Ferric Carboxymaltose in the Management of Iron ..." [17]: https://www.rcog.org.uk/media/sdqcorsf/gtg-47.pdf?utm_source=chatgpt.com "Blood Transfusion in Obstetrics" [18]: https://www.i4n.in/wp-content/uploads/2023/05/Anemia-Mukt-Bharat-Training-Modules-english.pdf?utm_source=chatgpt.com "ANEMIA MUKT BHARAT"
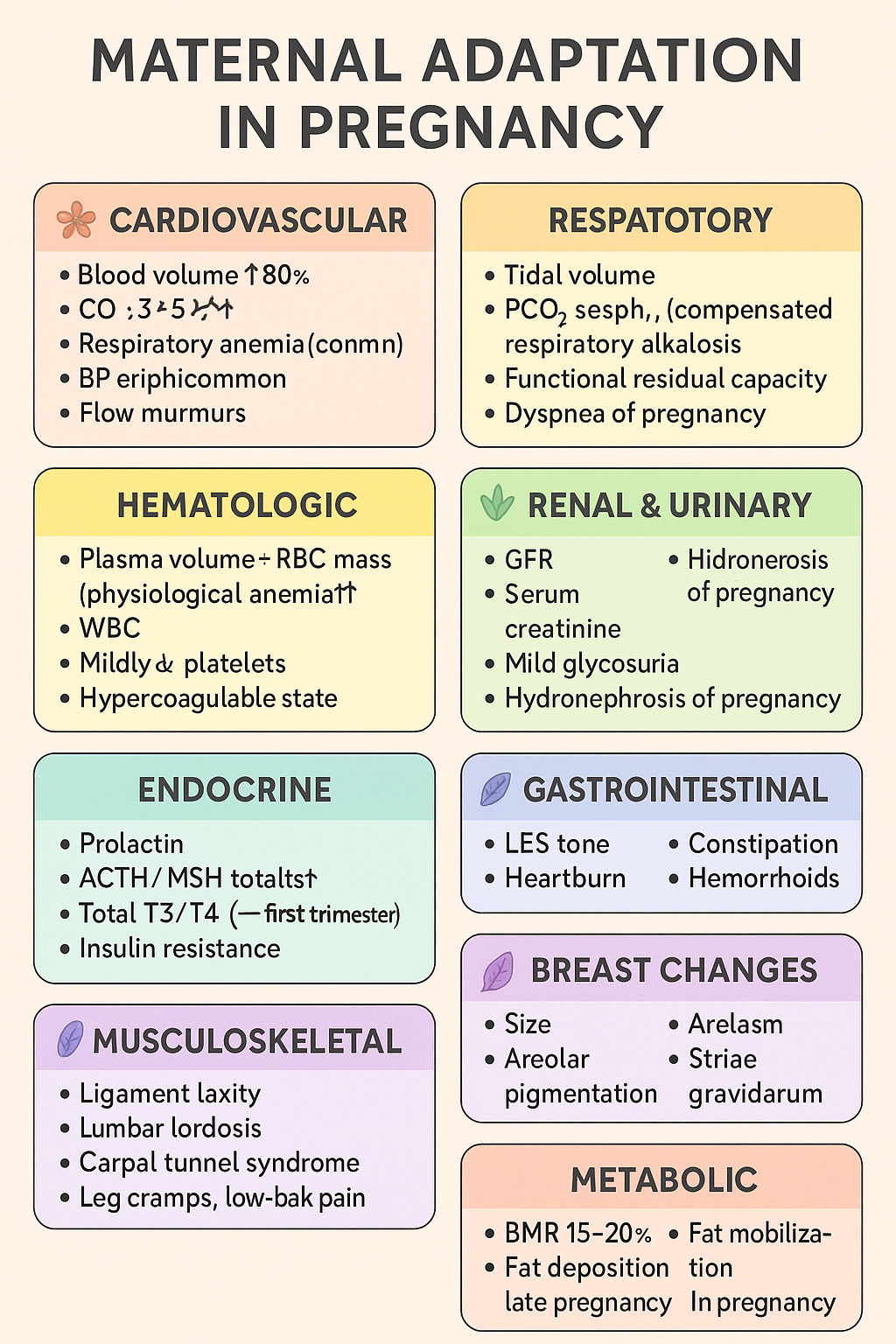
Maternal Adaptations in Pregnancy: Cardiovascular, Respiratory, Renal, Endocrine & Hematologic Changes | Complete Obstetrics Guide 2025
Below is your **complete, crisp but exhaustive stylish note** on **MATERNAL ADAPTATION IN PREGNANCY** — perfect for **NEET PG / INI-CET** and LWT article publishing. Presented in **high-yield, section-boxed format**. --- # ⭐ **MATERNAL ADAPTATIONS IN PREGNANCY — COMPLETE STYLISH NOTE (2025)** Pregnancy induces **multi-system physiologic adaptations** to support fetal growth, prepare for labor, and protect the mother from hemodynamic stresses. --- ## 🌸 **1. Cardiovascular Adaptations** ### 🔹 *Changes* * **Blood volume ↑ 40–50%** (plasma ↑ > RBC mass ↑ → *physiological anemia*). * **CO ↑ 30–50%** → peaks at 20–24 weeks. * **HR ↑ 10–20 bpm**. * **Systemic vascular resistance ↓** (progesterone-mediated vasodilation). * **BP ↓ in 2nd trimester**, returns to baseline in 3rd. * **Peripheral edema common** due to venous compression by gravid uterus. * **Flow murmurs, S3 may appear**. ### 🔹 *Clinical significance* * ↑ preload → protects from blood loss during delivery. * Supine position → **supine hypotension syndrome** (IVC compression). * Murmurs usually benign; still evaluate if symptomatic. --- ## 🌸 **2. Respiratory Adaptations** ### 🔹 *Changes* * **Tidal volume ↑ 30–40%**, minute ventilation ↑. * **PCO₂ ↓ → respiratory alkalosis (compensated)**. * **Functional residual capacity ↓** (diaphragm elevation by 4 cm). * **Dyspnea of pregnancy common** (physiological). ### 🔹 *Clinical significance* * Low PCO₂ → facilitates **placental CO₂ transfer**. * Increased ventilation → improved oxygenation for fetus. --- ## 🌸 **3. Hematologic Adaptations** ### 🔹 *Changes* * **Plasma volume ↑ 50%**, **RBC mass ↑ 20–30%** → dilution → **Hb ↓ (physiologic anemia)**. * **WBC ↑** (can reach 12–16k). * **Platelets mildly ↓** (gestational thrombocytopenia). * **Hypercoagulable state** → fibrinogen ↑, clotting factors ↑. ### 🔹 *Clinical significance* * Protects from postpartum hemorrhage. * ↑ VTE risk — especially postpartum. --- ## 🌸 **4. Renal & Urinary Adaptations** ### 🔹 *Changes* * **GFR ↑ 40–50%** (starts early). * **Serum creatinine ↓ 0.4–0.6 mg/dL**. * **Mild glycosuria** common. * **Hydronephrosis of pregnancy** (right > left) due to progesterone + uterine compression. ### 🔹 *Clinical significance* * Minor proteinuria acceptable (<300 mg/day). * Avoid misinterpreting physiologic glycosuria as diabetes. --- ## 🌸 **5. Endocrine Adaptations** ### 🔹 *Pituitary* * **Prolactin ↑** 10-fold → lactation prep. * **ACTH & MSH ↑** → pigmentation changes. ### 🔹 *Thyroid* * **Estrogen ↑ TBG**, total T3/T4 ↑; **free T4 normal**. * **hCG weak TSH activity → TSH ↓** (first trimester). ### 🔹 *Pancreas* * Early pregnancy: **insulin sensitivity ↑**. * Late pregnancy: **insulin resistance ↑** (placental hormones: hPL, cortisol) → predisposes to **GDM**. --- ## 🌸 **6. Gastrointestinal Adaptations** ### 🔹 *Changes* * **Progesterone ↓ LES tone** → heartburn. * **Gastric emptying ↓** → nausea/vomiting. * **Constipation** from prolonged transit time. * **Hemorrhoids** due to venous congestion. ### 🔹 *Clinical significance* * Morning sickness peaks at 9–10 weeks. * Hyperemesis gravidarum requires electrolyte correction. --- ## 🌸 **7. Musculoskeletal Adaptations** ### 🔹 *Changes* * **Relaxin + progesterone → ligament laxity**. * **Lumbar lordosis ↑** due to uterine weight. * **Carpal tunnel syndrome** possible. * **Leg cramps**, **low-back pain** common. ### 🔹 *Clinical significance* * Risk of falls increases. * Proper posture + exercises advised. --- ## 🌸 **8. Breast Changes** * **Size ↑**, ducts proliferate. * **Areolar pigmentation**, Montgomery tubercles prominent. * **Colostrum secretion** by late pregnancy. --- ## 🌸 **9. Dermatologic Adaptations** * **Linea nigra**, **melasma**, **striae gravidarum**. * **Spider angiomas**, palmar erythema (estrogen related). --- ## 🌸 **10. Metabolic Adaptations** * **Basal metabolic rate ↑ 15–20%**. * **Fat deposition ↑** early pregnancy. * Late pregnancy: catabolic → **fat mobilization** for maternal energy, glucose spared for fetus. --- # ⭐ **ULTRA-SHORT MEMORY HACK TABLE** | System | Key Adaptation | Why it Happens | | --------------- | ---------------------- | ---------------------------------------------------- | | CVS | CO ↑ 50%, plasma ↑ 50% | To meet fetal perfusion & buffer delivery blood loss | | Respiratory | TV ↑, PCO₂ ↓ | Better fetal CO₂ removal | | Renal | GFR ↑ 50% | Remove maternal/fetal waste | | Hematologic | Hypercoagulable | Prevent PPH | | Endocrine | Insulin resistance | Ensure fetal glucose | | GI | ↓ Motility | Progesterone effect | | Musculoskeletal | Ligament laxity | Prepare pelvis for birth | --- If you want, I can generate: ✅ **HTML-CSS-JS formatted article** (like your LWT posts) ✅ **MCQs (20/25/30 hard case-based)** ✅ **SEO title + description + keywords** ✅ **Custom medical diagram for maternal adaptations** Just tell me **which output you want next**.
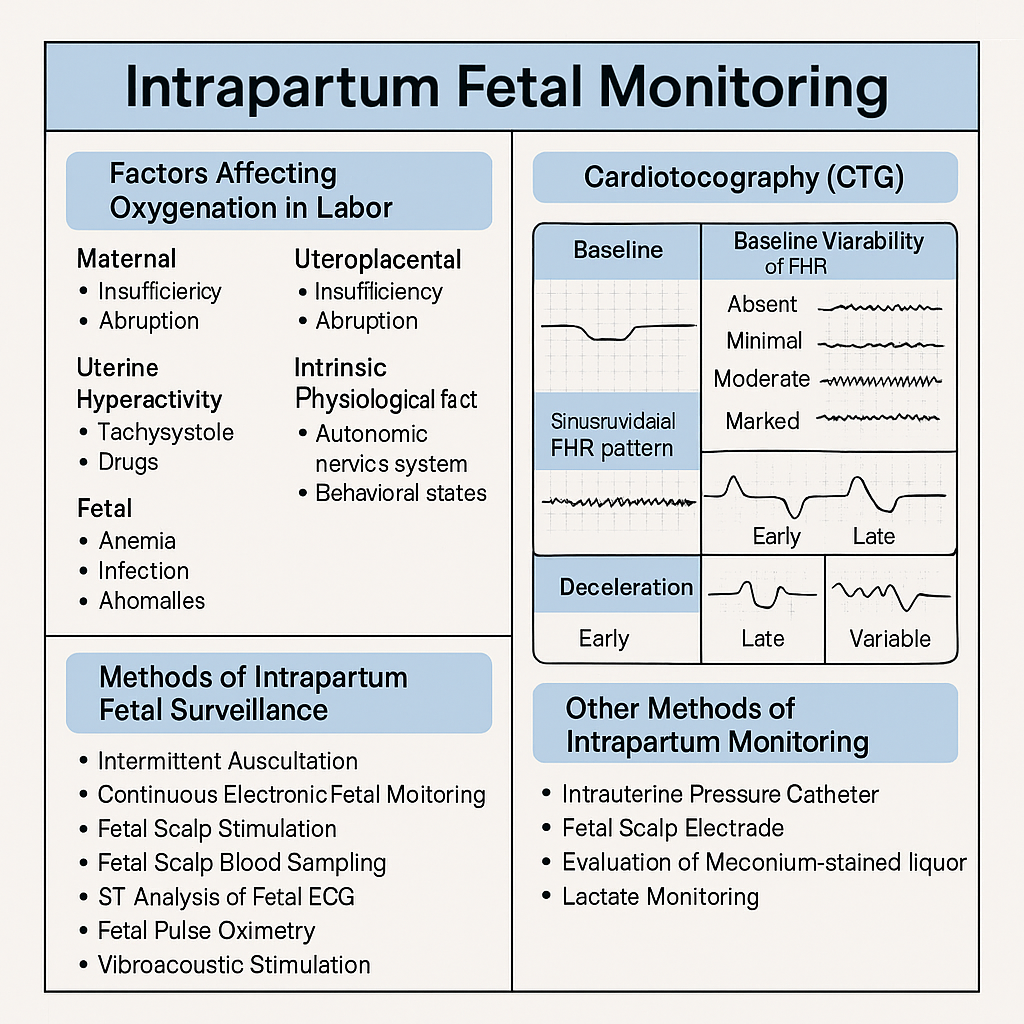
Intrapartum Fetal Monitoring: CTG Interpretation, Decelerations, Sinusoidal Pattern & Complete Management Guide 2025
Below are **30 detailed intrapartum fetal monitoring case scenarios with complete management**, written in **NEET PG / INI-CET exam style**. Each scenario includes **clinical context → CTG finding → diagnosis → step-wise management**. --- # ✅ **30 CASE SCENARIOS WITH DETAILED MANAGEMENT (Intrapartum Fetal Monitoring)** --- ## **1️⃣ Case — Late Decelerations in a Preeclamptic Mother** A 25-year-old primigravida, 4 cm dilated, on oxytocin. CTG shows **recurrent late decelerations**, baseline 150, variability <5 bpm. ### **Diagnosis** Uteroplacental insufficiency from **preeclampsia + hyperstimulation**. ### **Management** 1. Stop oxytocin 2. Left lateral position 3. IV fluids 4. If contraction frequency >5/10 min → **tocolysis (terbutaline 0.25 mg SC)** 5. If no improvement → **FBS** 6. If pH <7.20 or tracing deteriorates → **Emergency LSCS** --- ## **2️⃣ Case — Variable Decelerations with Oligohydramnios** G2P1, term labor, CTG shows **variable decelerations with shoulders**, adequate variability. ### **Diagnosis** Cord compression due to oligohydramnios. ### **Management** 1. Maternal repositioning 2. Amnioinfusion 3. Continue labor if variability normal 4. If severe recurrent variables + loss of variability → expedite delivery --- ## **3️⃣ Case — Sinusoidal Pattern** Rh-negative woman, fetus 38 weeks. CTG: **true sinusoidal pattern**. ### **Diagnosis** Severe fetal anemia. ### **Management** 1. Immediate evaluation (Kleihauer test, ultrasound MCA Doppler if time permits) 2. **Emergency LSCS** 3. Prepare NICU for transfusion --- ## **4️⃣ Case — Prolonged Deceleration from Cord Prolapse** During vaginal exam, a loop of cord felt. CTG shows **bradycardia at 80 bpm** for 4 minutes. ### **Management** 1. Lift presenting part manually 2. Knee–chest position 3. Call for emergency LSCS 4. Warm sterile saline-soaked gauze to prevent vasospasm 5. Deliver within **<30 minutes** --- ## **5️⃣ Case — Tachysystole-Induced Late Decelerations** Oxytocin infusion running, contractions 6/10 min. CTG: recurrent late decels. ### **Management** 1. Stop oxytocin immediately 2. Terbutaline 0.25 mg SC 3. Lateral position 4. Reassess 5. If persists → expedite delivery --- ## **6️⃣ Case — Minimal Variability for 50 Minutes** Primigravida in active labor. CTG: baseline 140, variability <5 bpm for 50 min, no decels. ### **Diagnosis** Non-reassuring CTG, possibly fetal sleep or medication effect. ### **Management** 1. Scalp stimulation 2. If acceleration present → reassuring 3. If absent → FBS or continuous monitoring 4. Continue labor if other parameters normal --- ## **7️⃣ Case — Meconium-Stained Liquor with Abnormal CTG** Thick meconium + variable decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. Amnioinfusion (if available) 3. Prepare for operative delivery 4. NICU standby for Meconium Aspiration Syndrome --- ## **8️⃣ Case — Prolonged Deceleration After Epidural** Immediately after epidural, FHR drops to 90 bpm for 3 minutes. ### **Diagnosis** Maternal hypotension causing decreased uteroplacental flow. ### **Management** 1. Left lateral position 2. IV fluid bolus 3. Vasopressor (phenylephrine preferred) 4. If persists beyond 5 minutes → consider LSCS --- ## **9️⃣ Case — Fetal Tachycardia with Maternal Fever** CTG shows FHR 180 bpm, moderate variability; maternal temp 101°F. ### **Diagnosis** Chorioamnionitis. ### **Management** 1. Broad-spectrum antibiotics 2. Acetaminophen 3. Expedite delivery (not LSCS solely for fever) 4. Avoid prolonged labor --- ## **🔟 Case — Arrest of Descent + Late Decelerations** Second stage, fully dilated, prolonged pushing, late decels appear. ### **Management** 1. Check for instrumental eligibility 2. **Forceps or vacuum** if head low 3. If not eligible → emergency LSCS --- ## **1️⃣1️⃣ Case — Recurrent Severe Variable Decelerations** CTG: variable decels dropping to 70 bpm for 60–90 sec. ### **Management** 1. Lateral positioning 2. Amnioinfusion 3. Reduce contractions if tachysystole 4. If persistent → operative delivery --- ## **1️⃣2️⃣ Case — Fetal Scalp pH Borderline** FBS pH = 7.22. ### **Management** 1. Correct reversible causes 2. Repeat FBS in 30 min 3. If worsens → expedite delivery --- ## **1️⃣3️⃣ Case — Loss of Variability with Bradycardia** Baseline 90 bpm, absent variability. ### **Diagnosis** Advanced fetal hypoxia. ### **Management** 1. Immediate decision for LSCS 2. No role of waiting or FBS --- ## **1️⃣4️⃣ Case — CTG Unable to Trace Due to Obesity** During labor, external CTG poor quality. ### **Management** 1. Switch to **fetal scalp electrode (FSE)** 2. Use IUPC for contraction monitoring 3. Continue labor normally if FHR normal --- ## **1️⃣5️⃣ Case — Category III CTG in Trial of Labor After Cesarean (TOLAC)** Late decels + minimal variability + scar tenderness. ### **Diagnosis** Scar rupture suspected. ### **Management** 1. Immediate emergency LSCS 2. Do NOT attempt instrumental delivery --- ## **1️⃣6️⃣ Case — Hyperstimulation Causing Decelerations** Misoprostol induction; CTG shows tachysystole + decels. ### **Management** 1. Stop prostaglandin 2. Tocolysis 3. Continuous monitoring 4. If fetal distress → emergency delivery --- ## **1️⃣7️⃣ Case — True Sinusoidal Pattern from Fetomaternal Hemorrhage** CTG sinusoidal; Kleihauer test positive. ### **Management** 1. Emergency delivery 2. Neonatal transfusion preparation --- ## **1️⃣8️⃣ Case — Prolonged Decel During Second Stage** Mother pushing vigorously; CTG shows bradycardia. ### **Management** 1. Stop pushing 2. Reassess for instrument delivery 3. If head + station → vacuum/forceps 4. Otherwise → LSCS --- ## **1️⃣9️⃣ Case — Mild Variable Decelerations with Normal Variability** Intermittent variables, contraction-associated. ### **Management** 1. Reassurance 2. Continue monitoring No intervention required. --- ## **2️⃣0️⃣ Case — Shoulder Dystocia + Bradycardia** Delivery nearly complete, FHR falls to 70 bpm. ### **Management** 1. McRoberts + suprapubic pressure 2. Deliver shoulders quickly 3. Neonatal resuscitation readiness --- ## **2️⃣1️⃣ Case — Cord Around Neck Detected on Ultrasound Before Labor** During labor → variable decels appear. ### **Management** 1. Continue monitoring 2. If severe or persistent → expedite delivery 3. Do not intervene solely for nuchal cord --- ## **2️⃣2️⃣ Case — Prolapsed Cord in Breech** CTG severe bradycardia. ### **Management** 1. Knee–chest position 2. Manual elevation of presenting part 3. Emergency LSCS --- ## **2️⃣3️⃣ Case — Minimal Variability from Opioid Analgesia** Given pethidine 15 min ago; variability <5. ### **Management** 1. Observe for 30–60 min 2. If variability recovers → continue 3. If not → evaluate for fetal hypoxia --- ## **2️⃣4️⃣ Case — Reassuring CTG in Low-Risk Labor** Baseline 140, variability 10, accelerations present. ### **Management** Continue routine monitoring. --- ## **2️⃣5️⃣ Case — Excessive Maternal Dehydration** CTG shows fetal tachycardia 170 bpm. ### **Management** 1. IV fluid bolus 2. Assess maternal vitals 3. Continue monitoring --- ## **2️⃣6️⃣ Case — Placental Abruption Suspected** Pain + bleeding + fetal tachycardia → later bradycardia. ### **Management** 1. Stabilize mother 2. Immediate LSCS if fetus alive 3. Vaginal delivery only if imminent --- ## **2️⃣7️⃣ Case — IUGR Baby with Recurrent Late Decelerations** CTG: late decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. No role for prolonged labor 3. **Expedite delivery** --- ## **2️⃣8️⃣ Case — Maternal Seizure (Eclampsia)** CTG: prolonged decel. ### **Management** 1. Stabilize mother (MgSO₄, airway) 2. Left lateral position 3. If fetal recovery absent → LSCS --- ## **2️⃣9️⃣ Case — Vaginal Birth After Multiple Variables** CTG mostly reassuring except mild variables. ### **Management** 1. Continue monitoring 2. Check for cord issues 3. No intervention unless severe --- ## **3️⃣0️⃣ Case — Failure of Fetal Response to Scalp Stimulation** Minimal variability, no acceleration after stimulation. ### **Diagnosis** Hypoxia suspected. ### **Management** 1. FBS if available 2. If pH abnormal → immediate delivery 3. If not available → treat as pathological CTG → expedite delivery --- If you want, I can also produce: ✅ **HTML + CSS + JS EXAM MODE MCQs (25/30/50)** ✅ **SEO title/description/keywords** ✅ **A medical diagram image for intrapartum fetal monitoring** Just say **“generate MCQs”**, **“generate image”**, or **“give SEO”**. Below is your **complete, concise-but-exhaustive master reference** on **Intrapartum Fetal Monitoring** — fully aligned with NEET PG / INI-CET high-yield requirements. --- # ⭐ **INTRAPARTUM FETAL MONITORING — COMPLETE DETAILED NOTES (2025)** --- ## **1️⃣ Factors Affecting Fetal Oxygenation During Labor** Fetal oxygenation depends on uninterrupted flow across **four levels**: ### **A. Maternal Factors** * **Maternal oxygenation:** Hypoxia, severe anemia, pulmonary disease. * **Uterine perfusion:** Hypotension (epidural, hemorrhage), dehydration, aortocaval compression. * **Uterine hyperactivity:** Tachysystole (>5 contractions/10 min), hypertonus ↓ intervillous blood flow. * **Drugs:** β-agonists ↑ fetal tachycardia; opioids ↓ variability. ### **B. Uteroplacental Factors** * Placental insufficiency (hypertension, preeclampsia, post-maturity). * Placental abruption, infarction, previa, accreta spectrum. * Umbilical cord compression (oligohydramnios, cord prolapse, tight nuchal cord). ### **C. Fetal Factors** * Fetal anemia, infections, acidosis. * Congenital anomalies (especially CNS, cardiac). * Prematurity → reduced variability. ### **D. Intrinsic Physiological Factors** * Autonomic nervous system balance (sympathetic/parasympathetic). * Fetal behavioral states (quiet sleep cycles ↓ variability). --- ## **2️⃣ Methods of Intrapartum Fetal Surveillance** ### **A. Intermittent Auscultation (IA)** * Using **Pinard stethoscope** or **Doppler**. * Low-risk pregnancies. * Frequency: * **1st stage:** every 30 min * **2nd stage:** every 5 min * Look for: baseline, accelerations, decelerations. ### **B. Continuous Electronic Fetal Monitoring (EFM / CTG)** * External US transducer + tocodynamometer. * Internal scaling: scalp electrode + IUPC (intrauterine pressure catheter) when needed. ### **C. Fetal Scalp Stimulation** * Acceleration after stimulation → reassuring (pH > 7.2). ### **D. Fetal Scalp Blood Sampling (FBS)** → Direct measure of fetal acid-base status. * **Normal pH ≥ 7.25** * **Borderline 7.21–7.24** * **Abnormal < 7.20** → urgent delivery. ### **E. ST-Analysis of Fetal ECG (STAN)** * Detects myocardial hypoxia (ST changes). * Used with CTG. ### **F. Fetal Pulse Oximetry (rare)** * Reassurance if SpO₂ > 30%. ### **G. Vibroacoustic Stimulation** * Sound stimulus → acceleration = good oxygenation. --- ## **3️⃣ Cardiotocography (CTG) – Complete Interpretation** CTG has **5 components**: **Baseline, Variability, Accelerations, Decelerations, Contractions.** --- ## **3.1 Baseline Fetal Heart Rate** Normal: **110–160 bpm** ### **Tachycardia (>160 bpm) causes:** * Maternal fever (chorioamnionitis) * Fetal hypoxia early * Fetal anemia * Drugs: β-agonists, atropine ### **Bradycardia (<110 bpm) causes:** * Vagal stimulation (head compression) * Cord compression * Prolonged deceleration → late sign of hypoxia --- ## **3.2 Baseline Variability (BV)** Reflects fetal autonomic integrity. | **Type** | **Range** | **Significance** | | --------------------- | ------------ | ------------------------------------------ | | Absent | 0 bpm | Severe hypoxia, acidosis, drugs | | Minimal | <5 bpm | Sleep cycle, opioids, prematurity, hypoxia | | **Moderate (Normal)** | **6–25 bpm** | Good oxygenation | | Marked | >25 bpm | Early hypoxia, cord compression | --- ## **3.3 Accelerations** * Abrupt ↑ in FHR by ≥15 bpm for ≥15 sec. * **Reassuring sign** → fetal well-being. --- ## **3.4 Decelerations — Types & Complete Interpretation** ### **A. Early Decelerations** * Mirror contractions. * Due to **head compression**. * **Benign, no treatment.** ### **B. Late Decelerations** * Begin after the contraction peak → return after contraction ends. * Due to **uteroplacental insufficiency**. * **Always concerning**, esp. with absent variability. ### **C. Variable Decelerations** * Abrupt fall in FHR, variable shape. * Due to **cord compression**. * May have "shoulders" (pre- & post-acceleration). * Severe if >60 bpm drop lasting >60 sec. ### **D. Prolonged Deceleration** * FHR drop ≥15 bpm lasting **2–10 min**. * > 10 min = change in baseline. ### **E. Sinusoidal Pattern (MOST IMPORTANT)** **True Sinusoidal Pattern** * Smooth, regular, sine-wave oscillation (3–5 cycles/min) * Amplitude 5–15 bpm * No variability, no accelerations * **Causes:** * Severe fetal anemia (Rh isoimmunization, fetomaternal hemorrhage) * Twin-to-twin transfusion * Hypoxia late stage * **Immediate delivery required** **Pseudo-sinusoidal:** * Seen with opioids — benign. --- ## **4️⃣ NICE 2024 Categories of CTG Interpretation** | Category | Findings | Action | | ------------------------------- | -------------------------------------------------------- | ------------------------------------------------ | | **Normal (Category I)** | Baseline 110–160, Variability 6–25, No repetitive decels | Continue | | **Suspicious (Category II)** | One non-reassuring feature | Correct reversible causes, close monitoring | | **Pathological (Category III)** | ≥1 abnormal feature OR ≥2 non-reassuring | Immediate evaluation, FBS, or expedited delivery | ### **Features** **Reassuring:** * Baseline 110–160 * Variability 6–25 * No decelerations / early decels * Accelerations present **Non-reassuring:** * Baseline 100–109 or 161–180 * Variability <5 for 40–90 min * Variable decels with features * Single prolonged decel <3 min **Abnormal:** * Baseline <100 or >180 * Variability <5 for >90 min * Late decels / prolonged decels >3 min * Sinusoidal pattern --- ## **5️⃣ Management of Abnormal CTG** ### **A. Correct Reversible Causes** * Left lateral position * IV fluids → treat maternal hypotension * Stop oxytocin (if tachysystole) * Tocolysis if uterine hyperstimulation (Terbutaline 0.25 mg SC) * Oxygen (only if maternal hypoxia) ### **B. Fetal Assessment** * Fetal scalp stimulation * FBS (pH or lactate) ### **C. Delivery** * If pH <7.20 OR pathological CTG persists * Emergency LSCS or instrumental delivery depending on stage --- ## **6️⃣ Other Methods of Intrapartum Monitoring** ### **A. Intrauterine Pressure Catheter (IUPC)** * Measures **Montevideo units** * Adequate labor: **>200 MVU** ### **B. Fetal Scalp Electrode (FSE)** * Accurate beat-to-beat FHR * Used when external CTG is poor. ### **C. Meconium-stained liquor evaluation** * Thick meconium + abnormal CTG → intrapartum hypoxia risk. ### **D. Lactate Monitoring** * Fetal scalp lactate <4.8 mmol/L reassuring. --- ## **7️⃣ Quick High-Yield Revision Table** | Topic | Key Points | | ------------------------------- | ------------------------------- | | Best indicator of fetal hypoxia | **Reduced variability** | | Worst CTG sign | **Sinusoidal pattern** | | Earliest sign of hypoxia | **Tachycardia** | | Most common deceleration | **Variable (cord compression)** | --- If you want, I can also generate: ✅ SEO title, description & keywords ✅ 25 hard case-based MCQs (HTML + CSS + JS EXAM MODE) ✅ 25 case scenarios with management ✅ Medical diagram image (via image generator) Just tell me **“continue”** with what you need.
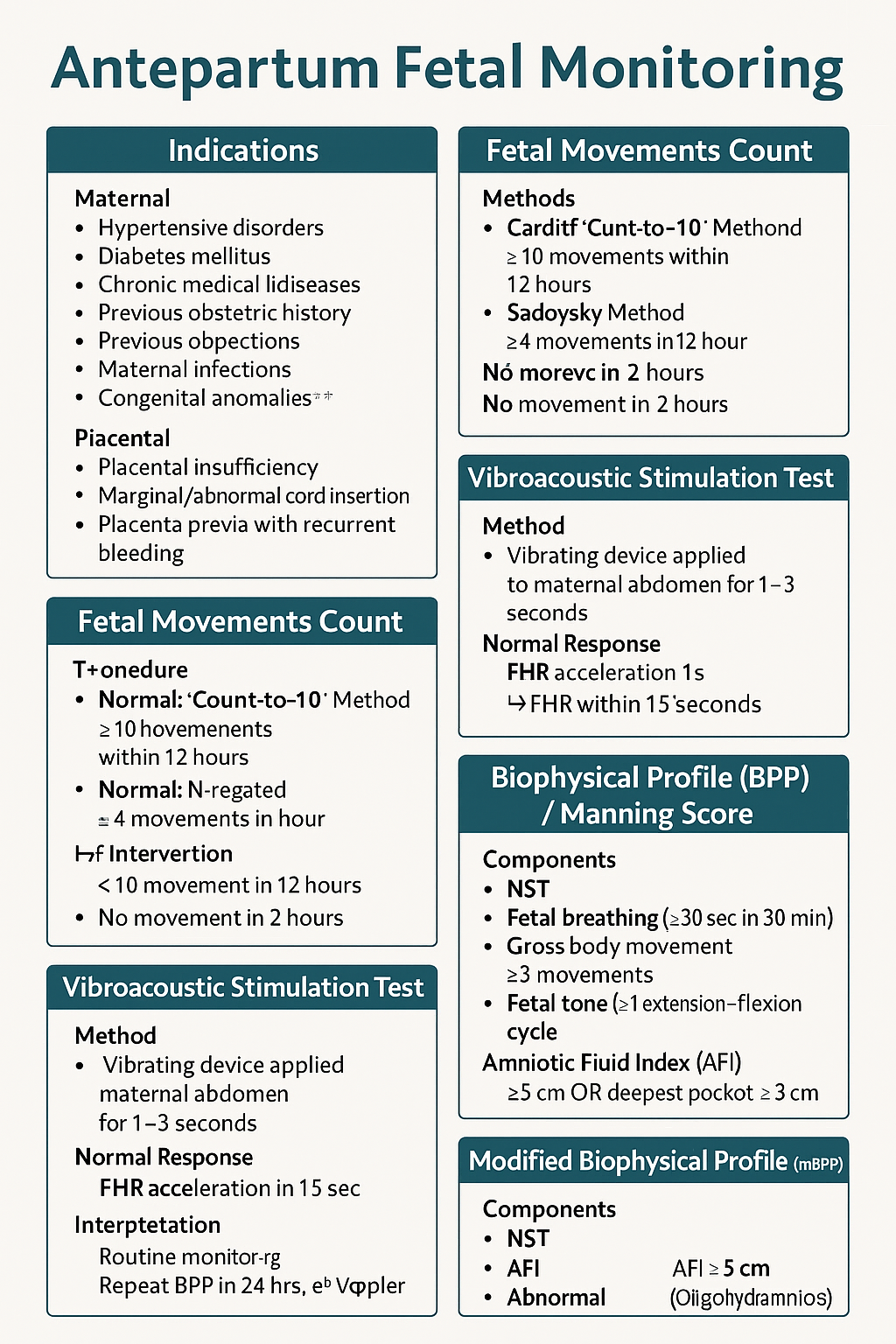
Antepartum Fetal Monitoring: Indications, NST, Biophysical Profile, Modified BPP & Vibroacoustic Test | Complete Obstetrics Guide 2025
--- # ⭐ **ANTEPARTUM FETAL MONITORING — COMPLETE HIGH-YIELD REFERENCE (NEET PG / INI-CET)** Antepartum fetal surveillance aims to detect **early fetal hypoxia** to prevent stillbirth, reduce perinatal morbidity, and guide timing of delivery. It assesses **placental function**, **oxygenation**, **neurological integrity**, and **fetal compensatory mechanisms**. --- # **1️⃣ Indications for Antepartum Fetal Monitoring** ### **A. Maternal Indications** * **Hypertensive disorders:** Gestational HTN, preeclampsia, eclampsia * **Diabetes mellitus:** GDM requiring insulin/OADs, pre-gestational DM * **Chronic medical diseases:** * Chronic hypertension * Renal disease * Autoimmune disease (SLE, APLA syndrome) * Cardiac disease * Thyroid disease with complications * **Previous obstetric history:** * Previous stillbirth * Previous IUGR baby * Previous neonatal death * Isoimmunization/Rh alloimmunization * **Maternal infections:** TORCH with fetal involvement * **Advanced maternal age (>35)** * **Post-dated pregnancy (>40 weeks)** ### **B. Fetal Indications** * **Decreased fetal movements** * **IUGR (Symmetric/Asymmetric)** * **Oligohydramnios / Polyhydramnios** * **Multiple pregnancy with complications** * **Fetal anemia / hydrops** * **Congenital anomalies** ### **C. Placental Indications** * Placental insufficiency * Marginal/Abnormal cord insertion * Placenta previa with recurrent bleeding --- # **2️⃣ Fetal Movement Count (FMC / Kick Count)** Fetal movements reflect fetal well-being (neurological + metabolic status). ### **Methods** ### **A. Cardiff Count-to-10 Method** * Mother records movements daily. * **Normal:** 10 movements within 12 hours. ### **B. Sadovsky Method** * Count movements for 1 hour after meals. * **Normal:** ≥4 movements/hour. ### **When to worry?** * **<10 movements in 12 hours** * **<4 movements in 1 hour** * **No movement in 2 hours** → urgent evaluation (NST/BPP) ### **Management of Decreased Fetal Movements** 1. Immediate **NST** 2. If NST non-reactive → **BPP** 3. If BPP equivocal → **Doppler studies** 4. If evidence of fetal compromise → **Delivery based on GA** --- # **3️⃣ Non-Stress Test (NST)** NST measures **fetal heart rate accelerations** in response to fetal movements via cardiotocography. ### **Procedure** * Done after **28–32 weeks** (mature autonomic nervous system). * Duration: **20 minutes** (extend to 40 minutes if needed). --- ## **Interpretation (Reactive vs Non-Reactive)** ### ✔ **Reactive NST (Normal)** * **≥2 accelerations** in 20 minutes * Acceleration criteria: * **≥15 bpm for ≥15 sec** (≥32 weeks) * **≥10 bpm for ≥10 sec** (<32 weeks) ### ✔ **Non-Reactive NST** * <2 accelerations in 40 minutes * Suggests fetal sleep cycle, hypoxia, CNS depression. ### **Causes of Non-Reactive NST** * Fetal sleep * Maternal drug intake (MgSO₄, opioids, sedatives) * Hypoxia * Prematurity * Congenital anomalies ### **Next Steps in Non-Reactive NST** * Vibroacoustic stimulation test * BPP * Contraction stress test (rarely used today) * Doppler studies --- # **4️⃣ Vibroacoustic Stimulation Test (VAST)** Used to differentiate fetal sleep from hypoxia in non-reactive NST. ### **Method** * A vibrating device (artificial larynx) applied to maternal abdomen for **1–3 seconds**. ### **Normal Response** * FHR acceleration within **15 seconds** * Converts non-reactive NST → **reactive** ### **Significance** * High negative predictive value * Reduces need for BPP --- # **5️⃣ Biophysical Profile (BPP) / Manning Score** Combines **NST + ultrasound parameters** assessing fetal CNS integrity + oxygenation. ### **Components (Total 10 points)** Each gets **2 = normal**, **0 = abnormal** | Component | Normal Criteria (2 points) | | ------------------------------ | --------------------------------- | | **NST** | Reactive | | **Fetal breathing** | ≥30 sec in 30 min | | **Gross body movement** | ≥3 movements | | **Fetal tone** | ≥1 extension–flexion cycle | | **Amniotic Fluid Index (AFI)** | AFI ≥5 cm OR deepest pocket ≥2 cm | --- ## **Scoring & Interpretation** | Score | Interpretation | Management | | -------- | -------------- | ------------------------------------------- | | **8–10** | Normal | Routine monitoring | | **6** | Equivocal | Repeat BPP in 24 hrs; evaluate Doppler | | **4** | Abnormal | Risk of fetal hypoxia → Delivery if ≥34 wks | | **0–2** | Severe hypoxia | Immediate delivery | --- # **6️⃣ Modified Biophysical Profile (mBPP)** Simplified & widely used. ### **Components** 1. **NST** 2. **AFI (Amniotic Fluid Index)** ### **Interpretation** * **Normal:** Reactive NST + AFI ≥5 cm * **Abnormal:** * Non-reactive NST * AFI <5 cm (Oligohydramnios) → placental insufficiency ### **Management** * If abnormal mBPP → full BPP or Doppler; consider delivery based on GA. --- # **7️⃣ Contraction Stress Test (OBSOLETE mostly)** Assesses fetal response to **uterine contractions** → risk of late decelerations. Rarely done due to risk + availability of Doppler and BPP. --- # **8️⃣ Putting It All Together — Management Algorithm** ### **Decreased fetal movements →** 1. **NST** 2. If reactive → reassure 3. If non-reactive → repeat + VAST 4. If still non-reactive → BPP 5. * **BPP ≤4** → Delivery * **BPP 6** → Repeat in 24 hrs * **BPP 8–10** → Continue routine follow-ups 6. Assess **AFI, Doppler, maternal condition** --- # **9️⃣ Important Clinical Correlations** ### **NST becomes abnormal earliest in fetal hypoxia** CNS activity reduces → loss of accelerations. ### **BPP components lost in sequence during hypoxia (Late → Early loss)** 1. **NST** 2. **Fetal breathing** 3. **Gross movement** 4. **Fetal tone** (last to disappear) 5. **AFI reduced** from chronic utero-placental insufficiency ### **AFI is chronic marker**; NST is acute marker. --- # ⭐ **HIGH-YIELD VALUES (MUST REVISE)** * Reactive NST: **≥2 accelerations** (15 × 15) * Tone: 1 flexion–extension * Breathing: ≥1 episode ≥30 sec * Movement: ≥3 body movements * AFI: Normal ≥5 cm * Modified BPP = NST + AFI * Sleep cycle: **20–40 min** → extend NST to 40 min --- --- # ⭐ **25 CASE SCENARIOS WITH DETAILED MANAGEMENT** *(Antepartum Fetal Surveillance: FMC, NST, BPP, VAST, mBPP)* --- # **1️⃣ Case Scenario – Decreased Fetal Movements at 34 Weeks** A 28-year-old G2P1 at 34 weeks reports **no fetal movements for 8 hours**. ### **Management** 1. Immediate **NST** 2. If **reactive** → reassure, daily kick count 3. If **non-reactive** → extend to 40 min 4. If still non-reactive → **VAST** 5. If remains non-reactive → **BPP** 6. * **BPP ≥8** → Follow-up * **BPP ≤4** → Deliver based on GA --- # **2️⃣ Case Scenario – Non-Reactive NST in a Diabetic Mother** GDM on insulin at 36 weeks undergoes NST → **non-reactive** after 40 minutes. ### **Management** 1. Perform **VAST** 2. If reactive → repeat NST in 1 week 3. If still non-reactive → **Full BPP** 4. If BPP score **≤4** → Plan delivery 5. Assess **AFI & Doppler** for placental insufficiency --- # **3️⃣ Case Scenario – Oligohydramnios with IUGR** 30-year-old at 32 weeks with **AFI = 4 cm**, EFW <10th percentile. ### **Management** 1. Start **modified BPP (NST + AFI)** 2. Daily NST 3. Doppler: **Umbilical artery S/D ratio** 4. If AEDF/REDF → **Immediate delivery** 5. If NST non-reactive → full BPP 6. Steroids if <34 weeks --- # **4️⃣ Case – Post-Dated Pregnancy (41 Weeks)** Patient at 41+2 weeks shows decreased fetal movement. ### **Management** 1. **NST + AFI** 2. If NST reactive & AFI normal → induce labour within 24–48 hrs 3. If NST non-reactive → BPP 4. BPP ≤6 → Deliver 5. Continuous intrapartum monitoring --- # **5️⃣ Case – Preeclampsia with Severe Features** 32 weeks, BP 160/110, proteinuria +++, fetus active. ### **Management** 1. Daily **NST** 2. Twice-weekly **BPP** 3. Doppler (UA + MCA) weekly 4. Magnesium sulfate for seizure prophylaxis 5. Deliver at 34 weeks or earlier if fetal compromise --- # **6️⃣ Case – Chronic Hypertension with Reduced Movements** 35-year-old with chronic HTN reports <4 kicks in 1 hr. ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. If AFI <5 → suspect placental insufficiency 4. Admit, daily surveillance 5. Deliver if BPP ≤4 or Doppler abnormal --- # **7️⃣ Case – IUGR with Normal NST** 29 weeks, IUGR but **reactive NST**. ### **Management** 1. Continue **twice-weekly NST** 2. Weekly Doppler (UA/ MCA/ CPR ratio) 3. Growth scan every 2 weeks 4. Deliver if Doppler deteriorates or NST becomes abnormal --- # **8️⃣ Case – Polyhydramnios with GDM** 30-year-old with polyhydramnios, NST reactive. ### **Management** 1. Twice-weekly NST 2. AFI monitoring 3. Doppler weekly 4. Induce at 38–39 weeks 5. Prepare for shoulder dystocia risk --- # **9️⃣ Case – Decreased Fetal Movement in Obese Mother** NST shows **baseline variability minimal**. ### **Management** 1. Rule out maternal meds, sleep cycle 2. Extend NST + VAST 3. If still abnormal → BPP 4. Deliver if BPP ≤4 --- # **🔟 Case – Rh-Isoimmunization** 28 weeks, MCA PSV >1.5 MOM (fetal anemia suspected). ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. Plan **intrauterine transfusion** 4. After IUT: Daily NST --- # **1️⃣1️⃣ Case – Twin Pregnancy with Growth Discordance** NST non-reactive for smaller twin. ### **Management** 1. VAST 2. If still non-reactive → BPP for each twin 3. Doppler UA/MCA/ Ductus venosus 4. Deliver if evidence of compromise --- # **1️⃣2️⃣ Case – Maternal Hypoglycemia Before NST** NST shows no accelerations. ### **Management** 1. Give oral glucose 2. Repeat NST 3. If becomes reactive → normal 4. If persistently non-reactive → VAST → BPP --- # **1️⃣3️⃣ Case – Placental Abruption Suspicion** Pain + bleeding + reduced movements. ### **Management** 1. **Immediate NST** 2. If late decelerations / bradycardia → **Immediate delivery** 3. Stabilize mother --- # **1️⃣4️⃣ Case – COVID Positive Mother with Decreased Movements** NST non-reactive. ### **Management** 1. Rule out maternal fever, hypoxia 2. Oxygen + hydration 3. VAST 4. If still non-reactive → BPP 5. Deliver if fetal compromise --- # **1️⃣5️⃣ Case – Smoking Mother with IUGR** NST shows decreased variability. ### **Management** 1. VAST 2. BPP 3. Doppler UA 4. Nicotine cessation + fetal surveillance every 2–3 days --- # **1️⃣6️⃣ Case – Absent Fetal Breathing on BPP** BPP = 6/10 (breathing absent). ### **Management** 1. Repeat BPP in 24 hrs 2. If repeat BPP ≤6 → Deliver 3. Continuous NST monitoring --- # **1️⃣7️⃣ Case – Low AFI but Reactive NST** AFI = 4 cm at 37 weeks. ### **Management** 1. Diagnose **oligohydramnios** 2. Admit, hydration 3. Modified BPP daily 4. Deliver at 37–38 weeks --- # **1️⃣8️⃣ Case – Maternal Seizure on MgSO₄** NST shows minimal variability (drug effect). ### **Management** 1. Continue monitoring 2. Do not interpret variability during MgSO₄ therapy 3. Use **BPP** instead of NST --- # **1️⃣9️⃣ Case – Poorly Controlled Diabetes** 36 weeks, polyhydramnios + macrosomia. ### **Management** 1. NST every 2–3 days 2. Weekly BPP 3. Deliver at 38 weeks 4. Prepare for shoulder dystocia --- # **2️⃣0️⃣ Case – Maternal Dehydration** NST non-reactive. ### **Management** 1. Give IV fluids 2. Repeat NST 3. If reactive → dehydration cause 4. If persists → BPP --- # **2️⃣1️⃣ Case – Postpartum Hemorrhage Risk Mother** Placenta previa major. ### **Management** 1. Weekly NST 2. BPP if NST abnormal 3. Plan elective C-section at 36–37 weeks --- # **2️⃣2️⃣ Case – Fetal Tachycardia** FHR 170 bpm in NST. ### **Management** 1. Exclude maternal fever, dehydration, drugs 2. Treat maternal cause 3. If persists → BPP + Doppler 4. Consider delivery if fetal compromise --- # **2️⃣3️⃣ Case – Mother on Sedatives** NST non-reactive. ### **Management** 1. Document medication effect 2. Perform BPP instead of repeating NST 3. Reassure if BPP normal --- # **2️⃣4️⃣ Case – Sudden IUD Suspicion** No FHR detected in NST. ### **Management** 1. Confirm with ultrasound 2. Evaluate cause (abruption, cord accident) 3. Manage according to GA and maternal stability --- # **2️⃣5️⃣ Case – Preterm (<32 Weeks) Non-Reactive NST** At 30 weeks, NST non-reactive. ### **Management** 1. Extend NST to 40 min 2. Apply VAST 3. If still non-reactive → BPP 4. If BPP ≤4 → Deliver after steroid cover 5. If BPP normal → prematurity likely cause ---
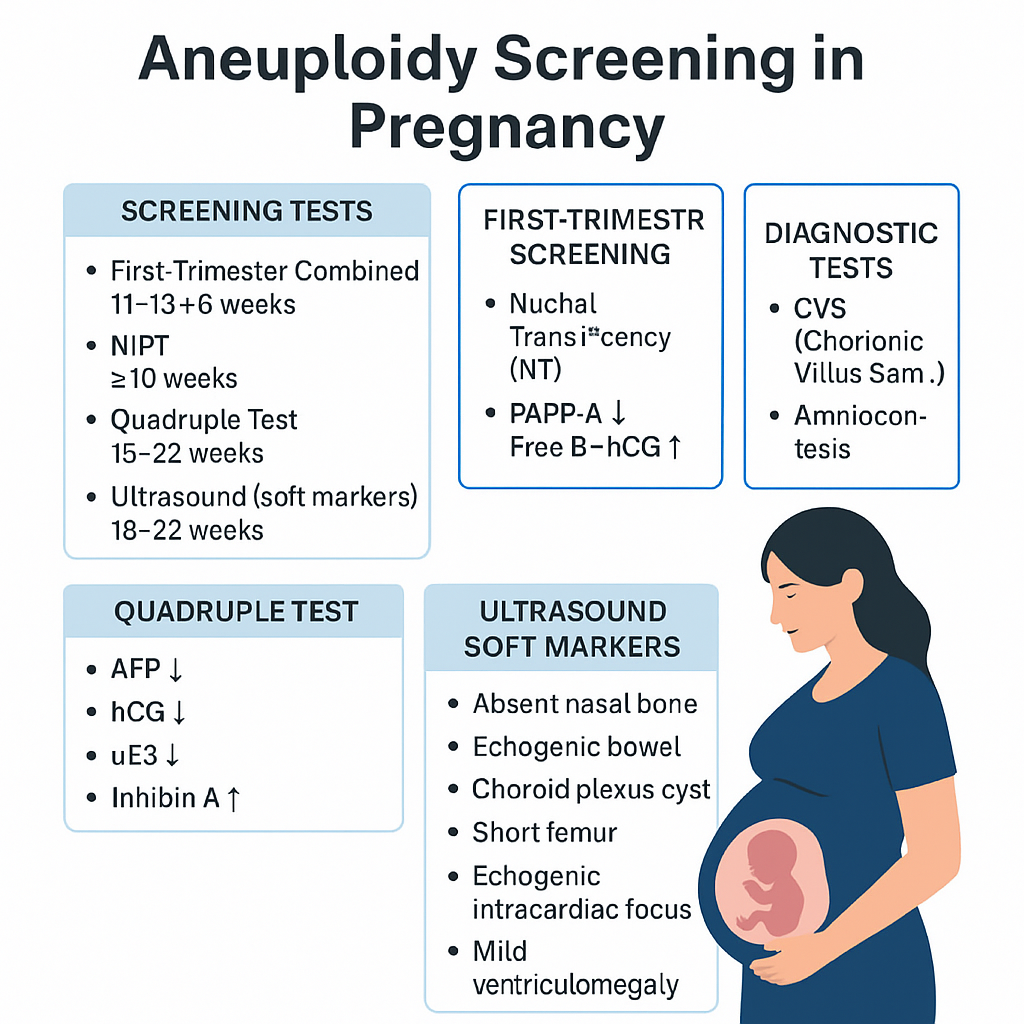
Aneuploidy Screening in Pregnancy: First Trimester, Quadruple Test, NIPT & Soft Markers | Complete Guide 2025
--- # ⭐ **Aneuploidy Screening in Pregnancy — Complete Obstetric Guide** Aneuploidy = **abnormal number of chromosomes** (most clinically relevant: **Trisomy 21, 18, 13**, Turner syndrome). Goal of screening = **identify pregnancies at increased risk** early enough to offer **diagnostic testing**. --- # **1. Why Aneuploidy Occurs (Basic Pathophysiology)** * **Meiotic nondisjunction** → failure of homologous chromosomes/sister chromatids to separate. * **Common in maternal meiosis I** (age-related). * **Trisomy 21 risk increases exponentially with maternal age**. * Mosaicism occurs if nondisjunction happens post-zygotically. --- # **2. High-Risk Factors** * Advanced maternal age (≥35 yrs). * Previous pregnancy with aneuploidy. * Parental balanced translocation (esp. Robertsonian). * Abnormal ultrasound markers (NT ↑, absent nasal bone, echogenic bowel, cardiac defects). * Abnormal biochemical screening results. --- # **3. Overview of Screening Timeline** | Gestation | Test | | ------------------- | ------------------------------------------------------------- | | **11–13+6 weeks** | First-trimester combined screening (NT + PAPP-A + free β-hCG) | | **10 weeks onward** | NIPT / cfDNA (highest accuracy) | | **15–22 weeks** | Second-trimester quadruple test | | **18–22 weeks** | Targeted anomaly scan (soft markers) | **Screening ≠ diagnosis.** Diagnostic tests = **CVS (10–13 wks)**, **Amniocentesis (≥15 wks)**, **FISH/karyotype/microarray**. --- # **4. First-Trimester Screening (11–13+6 Weeks)** ## **Components** 1. **Nuchal translucency (NT):** * Measured at CRL 45–84 mm * **NT >3.5 mm = major risk marker** * Increased NT → Trisomy 21/18/13, cardiac defects, Noonan syndrome, skeletal dysplasias 2. **Biochemical markers:** * **PAPP-A ↓**: Trisomy 21/18, placental insufficiency * **Free β-hCG ↑**: Trisomy 21 * **Free β-hCG ↓**: Trisomy 18/13 ## **Detection rate:** ~85–90% for T21 when combined. --- # **5. NIPT / cfDNA (Non-Invasive Prenatal Testing)** * Can be done **from 10 weeks onward**. * Analyzes **cell-free fetal DNA** in maternal blood. * **Most accurate screening test**. ## **Detects** * **Trisomy 21, 18, 13** * **Sex chromosome aneuploidies** (Turner, Klinefelter) * Microdeletions (low PPV, not recommended routinely) ## **Not diagnostic**, but: * **Sensitivity**: * T21 ≈ 99% * T18 ≈ 97–98% * T13 ≈ 92% ## **Causes of false results** * Confined placental mosaicism * Vanishing twin * Maternal malignancy * Low fetal fraction (<4%) --- # **6. Second-Trimester Quadruple Test (15–22 Weeks)** Markers: * **AFP** * **hCG** * **uE3 (unconjugated estriol)** * **Inhibin-A** ## **Patterns** ### **Trisomy 21** * **AFP ↓** * **uE3 ↓** * **hCG ↑** * **Inhibin-A ↑** ### **Trisomy 18** * **AFP ↓** * **uE3 ↓** * **hCG ↓** * **Inhibin-A normal** ### **Open neural tube defects** * **AFP ↑↑** Detection rate: * **~75% for T21** --- # **7. Ultrasound Soft Markers (18–22 Weeks)** ### **Major structural markers** * Cardiac defects (AV canal) → T21 * Holoprosencephaly → T13 * Omphalocele → T18 * Diaphragmatic hernia * Renal anomalies ### **Soft markers (non-structural)** | Marker | Association | | -------------------------------------- | --------------- | | **Absent nasal bone** | T21 | | **Echogenic intracardiac focus (EIF)** | Mild ↑ T21 risk | | **Echogenic bowel** | T21, CMV, CF | | **Short femur/humerus** | T21 | | **Choroid plexus cyst** | T18 | | **Single umbilical artery** | T18, T13 | | **Mild ventriculomegaly** | Aneuploidy risk | Soft markers **modify risk**, not diagnostic. --- # **8. Integrated & Sequential Screening** ### **Integrated test** * Combines first-trimester + second-trimester results * Highest combined detection before NIPT * Detection: **~94–95%**, but results available only in 2nd trimester ### **Sequential screening** * If first-trimester is high-risk → offer NIPT/CVS * If low-risk → continue with second trimester screening * More practical than integrated approach --- # **9. Diagnostic Tests (When Screening Is Positive)** ## **Chorionic Villus Sampling (CVS)** * **10–13+6 weeks** * Transcervical or transabdominal * Results: karyotype, microarray * Miscarriage risk: **~0.2–0.3%** ## **Amniocentesis** * **≥15 weeks** * Lower miscarriage risk: **0.1–0.2%** ## **Rapid tests** * **FISH** (24–48 hrs): detects T21, T18, T13 * **Microarray**: detects microdeletions/duplications --- # **10. Combined Detection Performance** | Test | Detection rate for T21 | | ------------------------ | ---------------------- | | First trimester combined | 85–90% | | Quadruple test | 75% | | Integrated screening | 94–95% | | **NIPT** | **>99%** | NIPT is **preferred**, especially for high-risk pregnancies. --- # **11. When to Offer NIPT (Indications)** * Maternal age ≥35 yrs * Previous trisomy pregnancy * Abnormal ultrasound markers * Positive biochemical screen * IVF pregnancies (optional but recommended) * Parental chromosomal rearrangement (screening may be inadequate → offer diagnostic test) --- # **12. Management Algorithm (Simplified)** ### **STEP 1: First antenatal visit** * Counsel regarding available screening methods * Offer **NIPT** to all (optimal) ### **STEP 2: If NT scan & biochemistry done** * **High-risk → NIPT or CVS** * **Intermediate risk → NIPT** * **Low risk → routine care** ### **STEP 3: Anomaly scan** * If any major structural abnormality → **Diagnostic test (CVS/Amniocentesis)** irrespective of NIPT result ### **STEP 4: If NIPT positive** * **Never terminate pregnancy based on NIPT alone** * Perform **confirmatory CVS/Amniocentesis** --- # **13. Counseling Points** * Screening ≠ diagnosis * Explain detection rates and false positives * Invasive diagnostic tests carry small miscarriage risks * A normal screen reduces but **does not eliminate** risk * Final decision is patient-centered --- # **14. Key Exam High-Yield Points** * **Most sensitive screening test:** NIPT * **Earliest diagnostic test:** CVS * **Best time for NT scan:** 11–13+6 weeks * **AFP ↑:** NTD, abdominal wall defects, incorrect dating * **AFP ↓ + hCG ↑ + uE3 ↓:** Trisomy 21 * **Choroid plexus cyst:** Trisomy 18 marker * **Absent nasal bone:** Down syndrome strongest soft marker * **Echogenic bowel:** Trisomy 21, CMV, CF ---
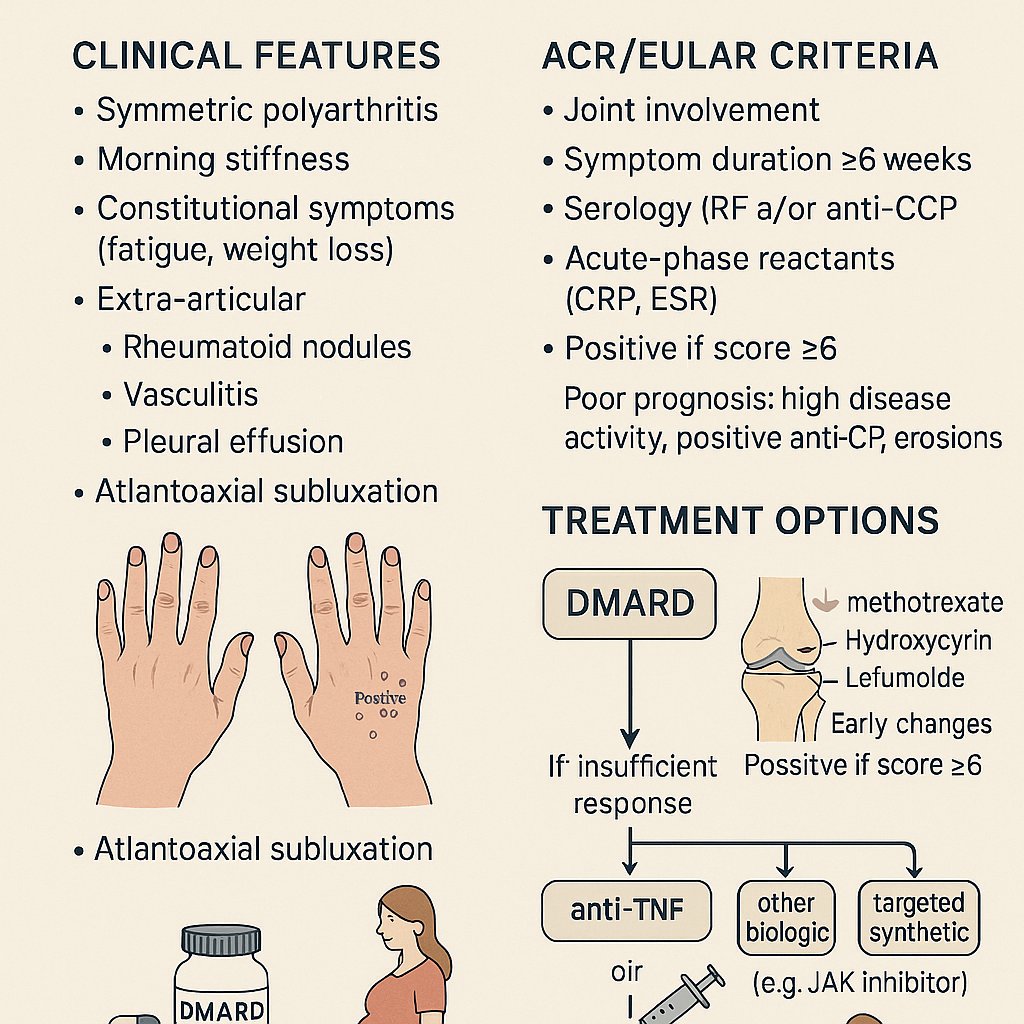
Rheumatoid Arthritis: Clinical Features, ACR/EULAR Criteria & Treatment Options
# **RHEUMATOID ARTHRITIS (RA)** **Clinical Features • ACR/EULAR 2010 Criteria • Diagnosis • Management (stepwise) • Drugs with MoA, dosing, AEs, contraindications, interactions, monitoring & counselling** --- # **1. Definition** Rheumatoid arthritis is a **chronic, systemic, autoimmune inflammatory polyarthritis** primarily affecting **synovial joints**, causing **persistent symmetric polyarthritis**, progressive joint destruction, disability, and extra-articular complications. It is mediated by **autoantibodies (RF, anti-CCP)** and **pro-inflammatory cytokines (TNF-α, IL-6, IL-1)**. --- # **2. Pathophysiology (Short but Complete)** * Genetic: **HLA-DRB1 shared epitope** strongly associated * Autoantibodies: **RF (IgM anti-Fc)** and **anti-CCP** (highly specific) * Inflammatory cascade → **synovial hyperplasia (pannus formation)** → cartilage erosion → bone destruction * Cytokines: **TNF-α, IL-6, IL-1**, JAK-STAT pathway activation * Extra-articular: vasculitis, nodules, ILD, anemia of chronic disease, scleritis * Accelerated **atherosclerosis** → ↑ CV mortality --- # **3. Clinical Features** ## **A. Articular** * **Symmetric small joint polyarthritis** (MCP, PIP, wrists; usually spares DIP) * **Morning stiffness > 1 hour** * Joint tenderness, boggy swelling * **Warm joints but not red** * **Deformities** (late): * Ulnar deviation * Swan-neck deformity * Boutonnière deformity * Z-thumb deformity * Reduced grip strength * In advanced disease: rheumatoid nodules, tendon rupture (e.g., **extensor tendon**) ## **B. Extra-articular** * **Rheumatoid nodules** * **Felty syndrome**: RA + neutropenia + splenomegaly * Ocular: **scleritis, episcleritis, keratoconjunctivitis sicca** * Pulmonary: **ILD, pleural effusion (exudative, low glucose)** * Cardiac: **pericarditis, ↑ CAD risk** * Hematology: anemia of chronic disease, thrombocytosis * Neurological: carpal tunnel syndrome, cervical spine (C1–C2) subluxation * Skin: vasculitic ulcers --- # **4. Investigations & Diagnosis** ### **A. Blood Tests** * **ESR/CRP** ↑ * **RF** positive in ~70–80% * **Anti-CCP**: highly specific (~95%), predicts severe disease * **CBC**: anemia of chronic disease, thrombocytosis * **LFT/RFT** baseline before DMARD therapy ### **B. Imaging** * **X-ray early**: soft tissue swelling, peri-articular osteopenia * **X-ray late**: joint space narrowing, erosions * **Ultrasound / MRI**: detects early synovitis & erosions --- # **5. ACR/EULAR 2010 Classification Criteria for RA** A score **≥ 6/10 = definite RA** ### **A. Joint involvement (0–5 points)** * 1 large joint → 0 * 2–10 large joints → 1 * 1–3 small joints → 2 * 4–10 small joints → 3 * > 10 joints (≥1 small) → 5 ### **B. Serology (0–3 points)** * RF negative & anti-CCP negative → 0 * Low-positive RF or low-positive anti-CCP → 2 * High-positive RF or anti-CCP → 3 ### **C. Acute-phase reactants (0–1 point)** * Normal ESR/CRP → 0 * Abnormal ESR/CRP → 1 ### **D. Duration of symptoms (0–1 point)** * <6 weeks → 0 * ≥6 weeks → 1 --- # **6. Differential Diagnoses** * Osteoarthritis * Psoriatic arthritis * SLE arthritis * Reactive arthritis * Viral polyarthritis (parvovirus B19, chikungunya) * Gout/pseudogout * Polymyalgia rheumatica --- # **7. Management (Stepwise & Evidence-Based)** ## **A. General Principles** * **Early aggressive treatment** with DMARDs * Aim: **remission or low disease activity** * Regular **DAS28** monitoring * Combination DMARDs if inadequate response * Avoid long-term steroids --- # **8. Pharmacologic Treatment (Full drug-level details)** # **1) First-line: Conventional DMARDs** --- ## **A. Methotrexate (MTX) – cornerstone** **Indication:** First-line DMARD for all moderate-severe RA **Mechanism:** Inhibits dihydrofolate reductase → ↓ purine synthesis; ↑ adenosine (anti-inflammatory) **Dose:** * Start 7.5–15 mg once weekly → titrate to **25 mg weekly**; give **folic acid 1 mg/day** **PK:** Hepatic metabolism, renal excretion **Common AEs:** GI upset, stomatitis, hair loss **Serious AEs:** Hepatotoxicity, myelosuppression, pneumonitis **Contraindications:** Pregnancy, liver disease, alcohol use disorder, severe renal impairment **Interactions:** TMP-SMX ↑ MTX toxicity; avoid NSAID excess **Monitoring:** CBC, LFT, RFT every 6–12 weeks **Counselling:** Once weekly dosing, avoid alcohol, report dyspnea --- ## **B. Leflunomide** **MoA:** Inhibits dihydroorotate dehydrogenase → ↓ pyrimidine synthesis **Dose:** 10–20 mg daily **AEs:** Hepatotoxicity, diarrhea, alopecia, teratogenic **Contra:** Pregnancy; need cholestyramine washout **Monitoring:** CBC, LFT every 8 weeks --- ## **C. Sulfasalazine** **MoA:** Anti-inflammatory; modulates cytokines **Dose:** 500 mg/day → 2–3 g/day **AEs:** Rash, GI upset, reversible oligospermia **Contra:** Sulfa allergy **Monitoring:** CBC, LFT --- ## **D. Hydroxychloroquine** **MoA:** Inhibits antigen presentation & TLR pathways **Dose:** 200–400 mg/day **AEs:** Retinopathy (dose-dependent) **Monitoring:** Baseline eye exam + annual screening after 5 yrs **Use:** Mild RA or combination therapy --- # **2) Biologic DMARDs (if inadequate response to MTX)** --- ## **A. Anti-TNF Agents** * **Etanercept** * **Infliximab** * **Adalimumab** * **Golimumab** * **Certolizumab** **MoA:** TNF-α blockade **AEs:** TB reactivation, infections, demyelination, CHF worsening **Contra:** Active infection, demyelinating disease **Monitoring:** TB screening, CBC, LFT **Counselling:** Report fever; maintain vaccination --- ## **B. Anti-IL-6 (Tocilizumab, Sarilumab)** **MoA:** IL-6 receptor blockade **AEs:** ↑ cholesterol, infections, GI perforation (esp. diverticulitis) --- ## **C. Anti-CD20 (Rituximab)** **MoA:** B-cell depletion **Use:** Refractory RA or when biologics contraindicated **AEs:** Infusion reactions, hepatitis B reactivation --- ## **D. CTLA-4 Fusion Protein (Abatacept)** **MoA:** Inhibits T-cell activation **AEs:** Infections, COPD exacerbation --- # **3) Targeted Synthetic DMARDs – JAK Inhibitors** * **Tofacitinib** * **Baricitinib** * **Upadacitinib** **MoA:** JAK-STAT inhibition → ↓ cytokine signaling **AEs:** Herpes zoster, ↑ LDL/HDL, thrombosis risk **Monitoring:** CBC, lipids, LFT **Counselling:** Vaccinate for zoster before therapy --- # **4) Glucocorticoids** * Used as **bridge therapy** until DMARDs act * Dose: **Prednisolone 5–10 mg/day short-term** * AEs: osteoporosis, weight gain, infection, HTN * Avoid chronic use * Provide **calcium + vitamin D** --- # **5) NSAIDs** * Symptomatic relief only * Do NOT prevent joint damage * Contra: renal disease, peptic ulcer, CVD --- # **9. Non-Pharmacologic Management** * Physiotherapy + joint-protection exercises * Smoking cessation (smoking worsens RA) * Weight optimisation * Vaccination: influenza, pneumococcal before biologics * Occupational therapy * Surgery: joint replacement in advanced destruction --- # **10. Follow-Up & Monitoring** * DAS28 scoring every 3 months * Monitor DMARD toxicity: CBC, LFT, RFT * Eye exams for hydroxychloroquine * TB screening annually for biologics --- # **11. Prognostic Factors** **Poor prognosis indicators:** * High RF/anti-CCP titers * Early erosions on X-ray * High disease activity (DAS28) * Extra-articular disease * Smoking * Early disability ---
Explore More
- Home Latest medical posts
- Sitelinks Index Complete site map
- Upload Medical Content Share clinical pearls
- Reviews & Suggestions Community feedback
- Help & FAQ Upload & SEO tips
- About Streamora Medical learning hub
- Contact Admin Support & queries
- All Medical Authors Browse all contributors