Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
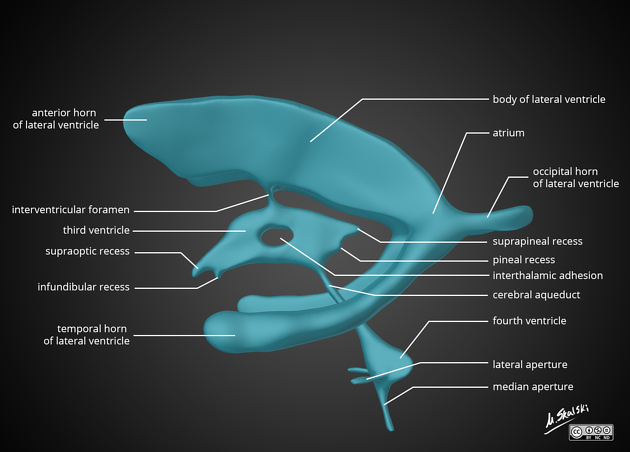
Cerebrospinal Fluid and Ventricular System Anatomy
## Cerebrospinal Fluid and Ventricular System Anatomy – Complete SEO-Friendly Guide ### SEO Title **Cerebrospinal Fluid and Ventricular System Anatomy** ### Meta Description Detailed anatomy of cerebrospinal fluid and the ventricular system covering formation, circulation, absorption, functions, ventricular components, and important clinical correlations. ### Keywords cerebrospinal fluid anatomy, ventricular system brain, lateral ventricles anatomy, third ventricle anatomy, fourth ventricle anatomy, CSF circulation, choroid plexus, arachnoid villi, hydrocephalus anatomy --- ## 1. Cerebrospinal Fluid (CSF) ### Definition Cerebrospinal fluid is a **clear, colorless fluid** that circulates within the **ventricular system of the brain and subarachnoid space** surrounding the brain and spinal cord, providing protection, nutrition, and waste removal. ### Normal Volume and Pressure * Total volume (adult): **≈150 mL** * Daily production: **≈500 mL** * Normal opening pressure (lumbar puncture): **70–180 mm H₂O** --- ## 2. Formation of CSF ### Choroid Plexus CSF is primarily produced by the **choroid plexus**, a vascular structure lined by **ependymal cells**. **Locations of choroid plexus** * Lateral ventricles (body and temporal horn) * Third ventricle * Fourth ventricle **Mechanism** * Active secretion via **Na⁺/K⁺ ATPase** * Water follows osmotically * Independent of intracranial pressure --- ## 3. Ventricular System of the Brain The ventricular system consists of **four interconnected cavities** lined by ependyma and filled with CSF. --- ### 3.1 Lateral Ventricles (First and Second Ventricles) **Location** * One in each cerebral hemisphere **Parts** 1. **Anterior (frontal) horn** * In frontal lobe * Roof: Corpus callosum * Floor: Head of caudate nucleus 2. **Body** * Extends through parietal lobe 3. **Posterior (occipital) horn** * In occipital lobe 4. **Inferior (temporal) horn** * In temporal lobe * Floor: Hippocampus * Roof: Tail of caudate nucleus **Communication** * Each lateral ventricle communicates with the third ventricle via the **interventricular foramen (foramen of Monro)** --- ### 3.2 Third Ventricle **Location** * Midline cavity between the two thalami **Boundaries** * Lateral walls: Thalamus and hypothalamus * Floor: Hypothalamus * Roof: Tela choroidea * Anterior wall: Lamina terminalis * Posterior wall: Pineal region **Connections** * Receives CSF from lateral ventricles * Drains into the fourth ventricle via the **cerebral aqueduct (aqueduct of Sylvius)** --- ### 3.3 Fourth Ventricle **Location** * Between pons and medulla anteriorly * Cerebellum posteriorly **Boundaries** * Floor: Rhomboid fossa * Roof: Superior and inferior medullary vela **Openings** * **One median aperture (foramen of Magendie)** * **Two lateral apertures (foramina of Luschka)** These openings allow CSF to enter the **subarachnoid space**. --- ## 4. Circulation of CSF **Flow pathway** 1. Lateral ventricles 2. Foramen of Monro 3. Third ventricle 4. Cerebral aqueduct 5. Fourth ventricle 6. Foramen of Magendie and Luschka 7. Subarachnoid space 8. Arachnoid villi and granulations 9. Superior sagittal sinus --- ## 5. Absorption of CSF ### Arachnoid Villi and Granulations * Protrusions of arachnoid mater into venous sinuses * Act as **one-way valves** * Absorption occurs when CSF pressure exceeds venous pressure Minor absorption also occurs via: * Spinal nerve sheaths * Choroid plexus --- ## 6. Composition of CSF * Clear and acellular * Low protein * Low potassium and calcium * Higher chloride compared to plasma * Glucose ≈ 60% of plasma glucose --- ## 7. Functions of CSF * **Mechanical protection** (shock absorber) * **Buoyancy** (reduces effective brain weight) * **Nutrient delivery** * **Removal of metabolic waste** * **Maintenance of intracranial pressure** --- ## 8. Blood–CSF Barrier Formed by: * Tight junctions between **choroid plexus epithelial cells** Functions: * Regulates composition of CSF * Protects CNS from toxins --- ## 9. Clinical Correlations ### Hydrocephalus * Abnormal accumulation of CSF **Types** * **Non-communicating (obstructive):** Block within ventricular system (e.g., aqueductal stenosis) * **Communicating:** Impaired absorption at arachnoid villi * **Normal pressure hydrocephalus:** Triad of gait disturbance, dementia, urinary incontinence --- ### Raised Intracranial Pressure * Headache * Vomiting * Papilledema * Altered consciousness --- ### Lumbar Puncture * Performed at **L3–L4 or L4–L5** * Measures CSF pressure and composition --- ## 10. High-Yield Exam Points * CSF production: **Choroid plexus** * Narrowest part of ventricular system: **Cerebral aqueduct** * Largest ventricles: **Lateral ventricles** * Main absorption site: **Arachnoid granulations** * CSF volume remains constant despite high daily production --- If you want, I can also provide **MCQs (exam-oriented)**, **clinical case-based questions**, or **schema-style revision tables** for CSF and ventricles.
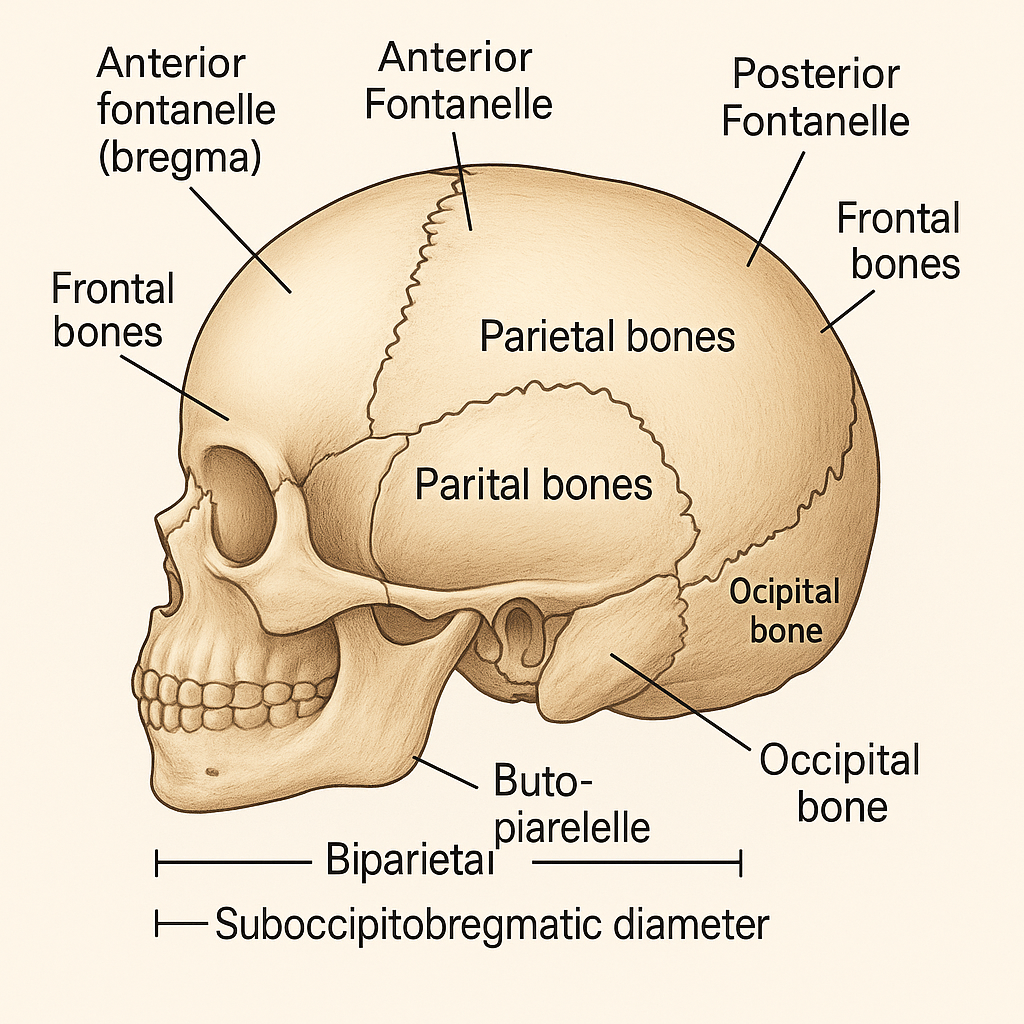
Fetal Skull Anatomy in Obstetrics: Sutures, Fontanelles, Diameters and Clinical Importance
## **SEO Title** **Fetal Skull Anatomy in Obstetrics: Sutures, Fontanelles, Diameters and Clinical Importance** ## **Meta Description** Comprehensive obstetrics-focused guide on fetal skull anatomy covering bones, sutures, fontanelles, diameters, molding, and their clinical significance during labor and delivery. ## **SEO Keywords** fetal skull obstetrics, fetal skull anatomy, sutures of fetal skull, fontanelles fetal skull, fetal skull diameters, molding of fetal skull, obstetric diameters, fetal head engagement, labor mechanism fetal skull --- # **Fetal Skull – Complete Obstetric Guide** ## **Introduction** The **fetal skull** is the most important part of the fetus in obstetrics because its **size, shape, flexibility, and diameters** determine the **mechanism of labor**, engagement, descent, and mode of delivery. --- ## **1. Structure of the Fetal Skull** The fetal skull is divided into **three main parts**: ### **A. Vault (Cranium) – Obstetrically Most Important** * Formed by **membranous bones** * Flexible and compressible * Allows **molding during labor** **Bones of the vault:** * 2 Frontal bones * 2 Parietal bones * Upper part of occipital bone --- ### **B. Base of the Skull** * Formed by **cartilaginous bones** * Rigid and non-compressible * Not affected by molding **Bones include:** * Sphenoid * Temporal * Lower occipital bone --- ### **C. Face** * Small obstetric significance * Important in **face presentation** --- ## **2. Sutures of the Fetal Skull** **Sutures** are fibrous joints between skull bones that allow overlapping during labor. | Suture | Location | Obstetric Importance | | ---------------------------- | ---------------------------------- | ---------------------------- | | **Sagittal suture** | Between parietal bones | Determines head position | | **Coronal suture** | Between frontal & parietal bones | Identifies degree of flexion | | **Lambdoid suture** | Between parietal & occipital bones | Helps locate occiput | | **Frontal (metopic) suture** | Between frontal bones | Indicates head attitude | --- ## **3. Fontanelles** Fontanelles are **membranous gaps** at the junction of sutures. ### **A. Anterior Fontanelle (Bregma)** * Diamond-shaped * Junction of **sagittal, coronal, and frontal sutures** * Closes by **18 months** * Palpation indicates **deflexed head** ### **B. Posterior Fontanelle (Lambda)** * Triangular * Junction of **sagittal and lambdoid sutures** * Closes by **6–8 weeks** * Palpation indicates **well-flexed vertex** **👉 Posterior fontanelle is the key landmark in normal labor** --- ## **4. Diameters of the Fetal Skull** Diameters are classified into **transverse and anteroposterior**. ### **A. Transverse Diameters** | Diameter | Measurement | Importance | | ----------------------------- | ----------- | ----------------- | | **Biparietal diameter (BPD)** | **9.5 cm** | Engaging diameter | | Bitemporal | 8 cm | Internal fit | | Bimastoid | 7.5 cm | Base diameter | --- ### **B. Anteroposterior Diameters** | Diameter | Measurement | Presentation | | ------------------------ | ----------- | -------------------------- | | **Suboccipitobregmatic** | **9.5 cm** | Well-flexed vertex (ideal) | | Suboccipitofrontal | 10 cm | Incomplete flexion | | Occipitofrontal | 11.5 cm | Deflexed vertex | | Mentovertical | 13.5 cm | Brow presentation | | Submentobregmatic | 9.5 cm | Face presentation | --- ## **5. Circumferences of the Fetal Head** | Circumference | Measurement | | -------------------- | ----------- | | Suboccipitobregmatic | ~32 cm | | Occipitofrontal | ~34 cm | | Mentovertical | ~38 cm | --- ## **6. Molding of the Fetal Skull** **Molding** refers to **overlapping of skull bones during labor**. ### **Grades of Molding** * **+ (Mild):** Sutures touching * **++ (Moderate):** Sutures overlapping but reducible * **+++ (Severe):** Overlapping not reducible (suggests CPD) **Clinical Importance** * Facilitates vaginal delivery * Excessive molding → fetal distress or obstructed labor --- ## **7. Caput Succedaneum** * Edematous swelling of scalp * Crosses suture lines * Appears at birth * Resolves spontaneously --- ## **8. Cephalhematoma** * Subperiosteal hemorrhage * Does **not cross suture lines** * Appears hours after birth * Resolves slowly --- ## **9. Obstetric Importance of the Fetal Skull** * Determines **engagement** * Helps assess **presentation and position** * Influences **mechanism of labor** * Guides **decision for vaginal delivery vs cesarean** * Critical in diagnosing **CPD and malpresentations** --- ## **Key Clinical Points** * **Best diameter for vaginal delivery:** Suboccipitobregmatic (9.5 cm) * **Most dangerous presentation:** Brow (mentovertical 13.5 cm) * **Posterior fontanelle palpable → normal vertex** * **Excessive molding → obstructed labor** --- If you want, I can also provide: * **SEO FAQs** * **Exam-oriented tables** * **25 hard case-based MCQs in HTML/CSS/JS (single file, modern UI)** * **Illustration prompts for image generation** Just tell me 👍

Contracted Pelvis and Cephalopelvic Disproportion Types Diagnosis Management
Below is a **concise yet complete, exam-oriented and SEO-friendly medical reference** covering **Contracted Pelvis, Cephalopelvic Disproportion (CPD), and Types of Pelvis**. Structured with **H1–H4 headings**, keyword-rich language, and clear clinical flow. **No images included**, as requested. --- # Contracted Pelvis and Cephalopelvic Disproportion: Types, Diagnosis and Management ## Introduction **Contracted pelvis** and **cephalopelvic disproportion (CPD)** are major causes of **obstructed labor**, **prolonged labor**, and **operative delivery**. Understanding **pelvic anatomy**, **pelvic types**, and **fetal–pelvic relationships** is essential for safe obstetric practice. --- ## Contracted Pelvis ### Definition A **contracted pelvis** is a pelvis in which **one or more pelvic diameters are reduced** below normal, interfering with the **descent and delivery of the fetus**. --- ### Causes of Contracted Pelvis #### Developmental Causes * Congenital pelvic abnormalities * Malnutrition during childhood * Rickets and osteomalacia #### Acquired Causes * Pelvic fractures with malunion * Tuberculosis of bones * Spinal deformities (kyphosis, scoliosis) * Previous pelvic surgery --- ### Classification of Contracted Pelvis #### 1. Anatomical Contracted Pelvis * **True contraction** of one or more diameters * Diagnosed by **pelvimetry** #### 2. Functional Contracted Pelvis * Pelvic diameters normal * Obstruction due to: * Large fetus * Malposition or malpresentation * Deflexed fetal head --- ### Degrees of Contracted Pelvis (Based on Obstetric Conjugate) | Degree | Obstetric Conjugate | Clinical Significance | | -------- | ------------------- | ------------------------- | | Mild | 9–10 cm | Vaginal delivery possible | | Moderate | 7.5–9 cm | Trial of labor | | Severe | <7.5 cm | Cesarean section | --- ## Cephalopelvic Disproportion (CPD) ### Definition **Cephalopelvic disproportion** occurs when the **fetal head is too large** or the **maternal pelvis too small** to allow vaginal delivery. --- ### Types of CPD #### 1. Absolute CPD * Gross pelvic contraction * Vaginal delivery **impossible** #### 2. Relative CPD * Borderline pelvis * Delivery depends on: * Fetal head molding * Position and attitude * Strength of uterine contractions --- ### Causes of CPD #### Maternal Factors * Contracted pelvis * Pelvic tumors * Short stature #### Fetal Factors * Macrosomia * Hydrocephalus * Occipitoposterior position * Deflexed head --- ### Clinical Features of CPD * Failure of head engagement * Prolonged labor * Cervical dystocia * Increasing caput and molding * Maternal exhaustion * Fetal distress --- ### Diagnosis of CPD #### Antenatal Assessment * History of difficult labor * Clinical pelvimetry * Ultrasound for fetal weight #### Intrapartum Diagnosis * Lack of descent despite good contractions * Non-progress of labor * Rising Bandl’s ring --- ### Management of CPD #### Antenatal * Identify high-risk cases * Plan mode of delivery #### Intrapartum * **Trial of labor** in selected cases * Continuous maternal and fetal monitoring #### Definitive Management * **Cesarean section** for: * Absolute CPD * Failed trial of labor * Fetal distress --- ## Types of Pelvis (Caldwell–Moloy Classification) ### 1. Gynecoid Pelvis * Most favorable for vaginal delivery * Rounded inlet * Wide subpubic angle * Straight side walls --- ### 2. Android Pelvis * Male-type pelvis * Heart-shaped inlet * Narrow mid-pelvis * Common cause of **arrest of descent** --- ### 3. Anthropoid Pelvis * Oval inlet (anteroposterior diameter increased) * Occipitoposterior position common * Vaginal delivery usually possible --- ### 4. Platypelloid Pelvis * Flattened pelvis * Wide transverse diameter * Narrow anteroposterior diameter * Engagement delayed --- ## Comparison of Pelvic Types | Pelvic Type | Inlet Shape | Labor Outcome | | ------------ | ------------ | ------------------ | | Gynecoid | Round | Best | | Android | Heart-shaped | Difficult | | Anthropoid | Oval (AP) | OP common | | Platypelloid | Flat | Engagement delayed | --- ## Clinical Importance * Major determinant of **mode of delivery** * Prevention of **obstructed labor** * Reduces maternal and perinatal morbidity * Essential for **exam preparation** and **clinical decision-making** --- ## Conclusion **Contracted pelvis and CPD** remain critical challenges in obstetrics. Accurate **pelvic assessment**, understanding **pelvic types**, and timely intervention ensure safe outcomes for both mother and fetus. --- ### SEO Keywords (Comma-Separated) contracted pelvis, cephalopelvic disproportion, CPD in obstetrics, types of pelvis, gynecoid pelvis, android pelvis, anthropoid pelvis, platypelloid pelvis, obstructed labor causes, pelvic contraction degrees, CPD diagnosis management If you want, I can also provide **case-based MCQs**, **exam notes**, or a **single-file HTML CSS JS quiz** on this topic.
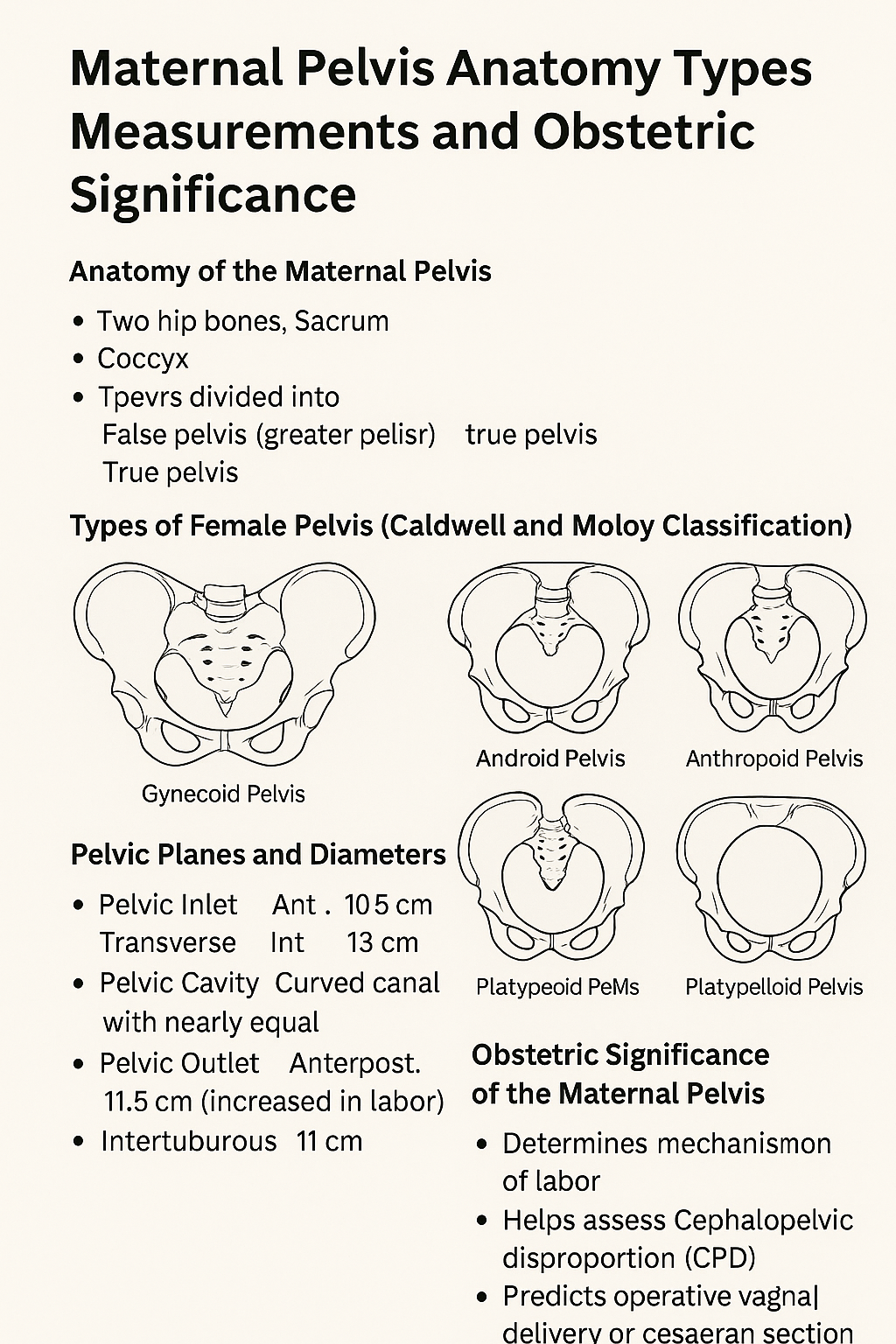
Maternal Pelvis Anatomy Types Measurements and Obstetric Significance
# **Maternal Pelvis Anatomy Types Measurements and Obstetric Significance** ## **Introduction** The **maternal pelvis** is a rigid bony structure that forms the birth canal. Its **shape, size, and dimensions** are critical determinants of **labor progression, fetal descent, and delivery outcome**. In obstetrics, detailed assessment of the maternal pelvis helps predict **normal vaginal delivery, obstructed labor, and cephalopelvic disproportion**. --- ## **Anatomy of the Maternal Pelvis** ### **1. Bones Forming the Pelvis** * **Two hip bones** (each formed by ilium, ischium, and pubis) * **Sacrum** * **Coccyx** These bones unite to form a **bony ring** that supports pelvic organs and provides a passage for childbirth. --- ## **Divisions of the Maternal Pelvis** ### **1. False Pelvis (Greater Pelvis)** * Located above the pelvic brim * Supports the gravid uterus * Has **no direct role in labor** ### **2. True Pelvis (Lesser Pelvis)** * Located below the pelvic brim * Forms the **birth canal** * Obstetrically important part --- ## **Pelvic Brim (Inlet)** The pelvic brim separates the false and true pelvis. ### **Boundaries** * Sacral promontory (posterior) * Ala of sacrum * Linea terminalis * Upper border of pubic symphysis (anterior) --- ## **Planes and Diameters of the Maternal Pelvis** ### **1. Pelvic Inlet** **Important diameters** * **Anteroposterior (Obstetric conjugate)**: ~10.5 cm * **Transverse diameter**: ~13 cm * **Oblique diameter**: ~12 cm **Clinical importance** * Determines engagement of fetal head --- ### **2. Pelvic Cavity** * Curved canal with nearly equal AP and transverse diameters * Smooth lateral walls favor rotation of the fetal head --- ### **3. Pelvic Outlet** **Boundaries** * Ischial tuberosities * Coccyx * Lower border of pubic arch **Important diameters** * **Anteroposterior**: ~11.5 cm (increases during labor due to coccygeal movement) * **Intertuberous diameter**: ~11 cm **Clinical importance** * Determines completion of vaginal delivery --- ## **Types of Female Pelvis (Caldwell and Moloy Classification)** ### **1. Gynecoid Pelvis** * Rounded inlet * Wide subpubic angle * Straight side walls **Most favorable for vaginal delivery** ### **2. Android Pelvis** * Heart-shaped inlet * Narrow forepelvis * Prominent ischial spines **Associated with deep transverse arrest** ### **3. Anthropoid Pelvis** * Oval inlet with long AP diameter * Favors occipitoposterior positions **Vaginal delivery usually possible** ### **4. Platypelloid Pelvis** * Flattened inlet * Wide transverse diameter * Short AP diameter **Engagement may be difficult** --- ## **Obstetric Significance of the Maternal Pelvis** * Determines **mechanism of labor** * Helps assess **cephalopelvic disproportion** * Predicts **operative vaginal delivery or cesarean section** * Influences fetal head **engagement, rotation, and descent** --- ## **Clinical Assessment of the Maternal Pelvis** ### **1. Clinical Pelvimetry** * Performed per vaginum * Assesses pelvic inlet, cavity, and outlet ### **2. Imaging Pelvimetry** * X-ray, CT, or MRI pelvimetry * Reserved for selected cases --- ## **Common Obstetric Problems Related to Pelvis** * Contracted pelvis * Obstructed labor * Prolonged labor * Fetal malposition and malrotation --- ## **Conclusion** The **maternal pelvis** plays a decisive role in childbirth. Knowledge of **pelvic anatomy, dimensions, and pelvic types** is essential for safe obstetric practice, early identification of labor complications, and appropriate delivery planning. --- ### **SEO Keywords** maternal pelvis anatomy, types of female pelvis, obstetric pelvis, pelvic inlet outlet diameters, gynecoid pelvis, android pelvis, anthropoid pelvis, platypelloid pelvis, pelvic planes obstetrics, clinical pelvimetry If you want, I can **generate 25 hard case-based MCQs in a single HTML CSS JS file**, or **convert this into exam notes or infographic-ready content**.
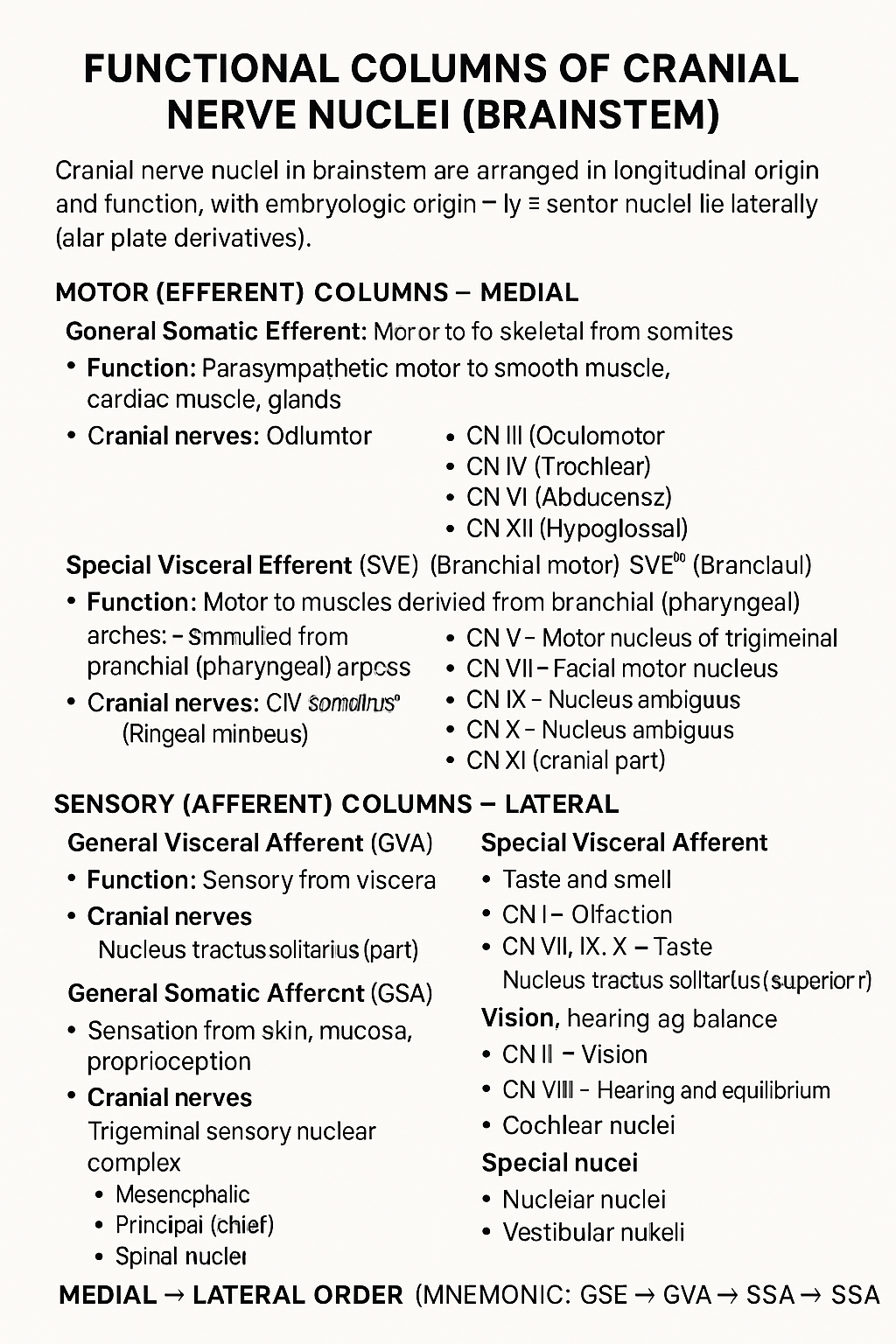
Functional Columns of Cranial Nerve Nuclei in Brainstem
## Functional Columns of Cranial Nerve Nuclei (Brainstem) Cranial nerve nuclei in the brainstem are arranged in **longitudinal functional columns** based on **embryologic origin** and **function**. **Motor nuclei lie medially** (basal plate derivatives) and **sensory nuclei lie laterally** (alar plate derivatives). --- ## MOTOR (EFFERENT) COLUMNS – Medial ### 1. **General Somatic Efferent (GSE)** * **Function:** Motor to skeletal muscles derived from **somites** * **Muscles supplied:** Extraocular muscles, tongue muscles * **Cranial nerves:** * CN III (Oculomotor) * CN IV (Trochlear) * CN VI (Abducens) * CN XII (Hypoglossal) --- ### 2. **General Visceral Efferent (GVE)** * **Function:** **Parasympathetic** motor to smooth muscle, cardiac muscle, glands * **Cranial nerves & nuclei:** * CN III – Edinger–Westphal nucleus * CN VII – Superior salivatory nucleus * CN IX – Inferior salivatory nucleus * CN X – Dorsal motor nucleus of vagus --- ### 3. **Special Visceral Efferent (SVE)** *(Branchial motor)* * **Function:** Motor to muscles derived from **branchial (pharyngeal) arches** * **Muscles supplied:** Muscles of mastication, facial expression, pharynx, larynx * **Cranial nerves:** * CN V – Motor nucleus of trigeminal * CN VII – Facial motor nucleus * CN IX – Nucleus ambiguus * CN X – Nucleus ambiguus * CN XI (cranial part) --- ## SENSORY (AFFERENT) COLUMNS – Lateral ### 4. **General Visceral Afferent (GVA)** * **Function:** Sensory from viscera * **Cranial nerves:** * CN IX * CN X * **Nucleus:** Nucleus tractus solitarius (inferior part) --- ### 5. **Special Visceral Afferent (SVA)** * **Function:** Taste and smell * **Cranial nerves:** * CN I – Olfaction * CN VII, IX, X – Taste * **Nucleus:** Nucleus tractus solitarius (superior part) --- ### 6. **General Somatic Afferent (GSA)** * **Function:** Sensation from skin, mucosa, proprioception * **Cranial nerves:** * CN V (main) * CN VII, IX, X (small contributions) * **Nuclei:** * Trigeminal sensory nuclear complex * Mesencephalic * Principal (chief) * Spinal nucleus --- ### 7. **Special Somatic Afferent (SSA)** * **Function:** Vision, hearing, balance * **Cranial nerves:** * CN II – Vision * CN VIII – Hearing and equilibrium * **Nuclei:** * Cochlear nuclei * Vestibular nuclei --- ## MEDIAL → LATERAL ORDER (Mnemonic) **GSE → GVE → SVE → GVA → SVA → GSA → SSA** --- If you want, I can also provide: * **One-table summary (exam revision)** * **Clinical correlations** * **Simple mnemonics for each column** * **Neat labelled text diagram (ASCII-style)**
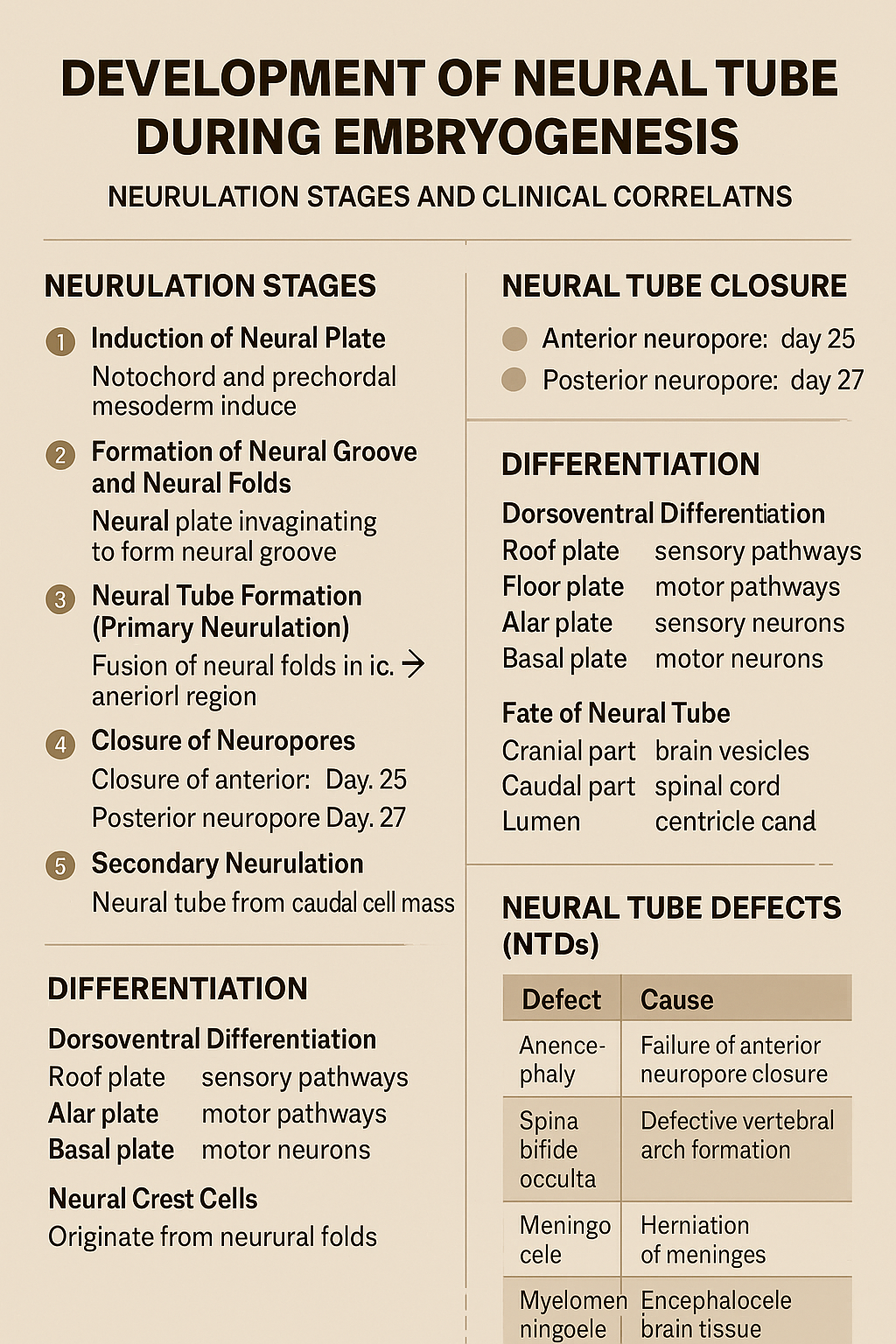
Development of Neural Tube During Embryogenesis Neurulation Stages and Clinical Correlation
## Development of the Neural Tube (Neurulation) ### **Definition** The **neural tube** is the embryonic precursor of the **central nervous system (CNS)**, forming the **brain and spinal cord**. Its development occurs by **neurulation** during the **3rd and 4th weeks of intrauterine life**. --- ## **Timeline** * **Day 18**: Neural plate appears * **Day 20–21**: Neural folds form * **Day 22**: Fusion begins in cervical region * **Day 25**: Closure of anterior (cranial) neuropore * **Day 27**: Closure of posterior (caudal) neuropore --- ## **Phases of Neural Tube Development** ### **1. Induction of Neural Plate** * The **notochord** and **prechordal mesoderm** induce overlying **ectoderm**. * Ectoderm thickens to form the **neural plate**. **Key signaling molecules**: * Sonic hedgehog (Shh) * Noggin * Chordin * Follistatin --- ### **2. Formation of Neural Groove and Neural Folds** * Central neural plate invaginates → **neural groove**. * Lateral edges elevate → **neural folds**. * Neural folds approach each other dorsally. --- ### **3. Neural Tube Formation (Primary Neurulation)** * Neural folds fuse in the **midline**, starting in the **cervical region**. * Fusion proceeds cranially and caudally. * Temporary openings remain: * **Anterior (cranial) neuropore** * **Posterior (caudal) neuropore** --- ### **4. Closure of Neuropores** * **Anterior neuropore closes (Day 25)** → brain development * **Posterior neuropore closes (Day 27)** → spinal cord development Failure of closure leads to **neural tube defects**. --- ### **5. Secondary Neurulation** * Occurs in the **caudal region (below S2)**. * Neural tube forms from **caudal cell mass**. * Important for formation of: * Conus medullaris * Filum terminale --- ## **Differentiation of the Neural Tube** ### **Neural Tube Wall Layers** 1. **Ventricular (ependymal) layer** – neuroepithelial cells 2. **Mantle layer** – gray matter 3. **Marginal layer** – white matter --- ### **Dorsoventral Differentiation** * **Roof plate** → sensory pathways * **Floor plate** → motor pathways * **Alar plate** → sensory neurons * **Basal plate** → motor neurons * **Sulcus limitans** separates alar and basal plates --- ## **Fate of Neural Tube** * **Cranial part** → brain vesicles * Prosencephalon * Mesencephalon * Rhombencephalon * **Caudal part** → spinal cord * **Lumen** → ventricles and central canal --- ## **Neural Crest Cells (Related Event)** * Originate from neural folds * Migrate extensively * Form: * Peripheral nervous system * Melanocytes * Adrenal medulla * Craniofacial cartilage --- ## **Clinical Correlation: Neural Tube Defects (NTDs)** | Defect | Cause | | -------------------- | ------------------------------------- | | Anencephaly | Failure of anterior neuropore closure | | Spina bifida occulta | Defective vertebral arch formation | | Meningocele | Herniation of meninges | | Myelomeningocele | Herniation of spinal cord + meninges | | Encephalocele | Herniation of brain tissue | **Risk factors**: * Folic acid deficiency * Maternal diabetes * Valproate exposure **Prevention**: * Folic acid 400–800 µg/day (preconception) --- ### **One-Line Exam Summary** > The neural tube forms from ectoderm by neurulation during weeks 3–4 and develops into the brain and spinal cord. If you want, I can also provide **exam-oriented MCQs, flowcharts, or comparison tables** for neurulation.
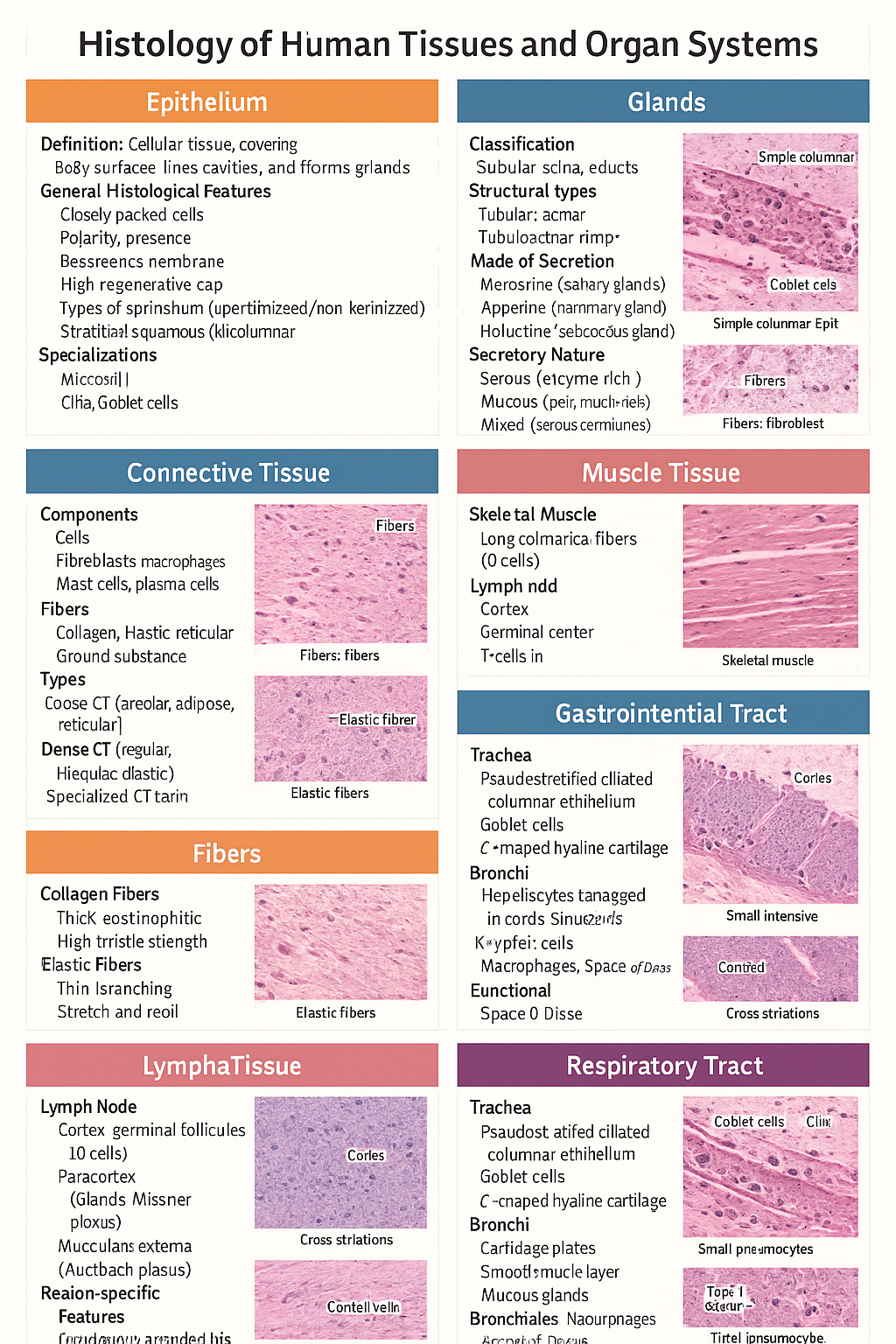
Histology of Epithelium, Connective Tissue, Muscle, Cartilage, Glands, GIT, Liver and Respiratory Tract
Below is a **single-place, SEO-optimized, exam-ready histology guide** covering **epithelium, glands, connective tissue, fibers, cartilage, muscle, lymphatic system, GIT, liver, and respiratory tract**. Structured with **clear H1–H3 headings**, **high-yield features**, and **clinical correlations** for medical students and competitive exams. --- # Histology of Human Tissues and Organ Systems – Complete Guide ## Histology of Epithelium ### Definition Epithelium is a **cellular tissue** that covers body surfaces, lines cavities, and forms glands. ### General Histological Features * Closely packed cells with **minimal extracellular matrix** * **Polarity**: apical, lateral, basal surfaces * **Basement membrane** present * **Avascular**, richly innervated * High **regenerative capacity** ### Types of Epithelium * **Simple squamous**: alveoli, capillaries * **Simple cuboidal**: kidney tubules, glands * **Simple columnar**: stomach, intestine * **Stratified squamous (keratinized/non-keratinized)**: skin / oral cavity * **Pseudostratified ciliated columnar**: trachea * **Transitional epithelium**: urinary bladder ### Specializations * **Microvilli** – absorption * **Cilia** – movement * **Goblet cells** – mucus secretion --- ## Histology of Glands ### Classification * **Exocrine glands** – ducts present * **Endocrine glands** – ductless, secrete into blood ### Structural Types * **Tubular**, **acinar**, **tubuloacinar** * **Simple** or **compound** ### Mode of Secretion * **Merocrine** (salivary glands) * **Apocrine** (mammary gland) * **Holocrine** (sebaceous gland) ### Secretory Nature * **Serous** – enzyme-rich, dark staining * **Mucous** – pale, mucin-rich * **Mixed** – serous demilunes --- ## Histology of Connective Tissue ### Components * **Cells**: fibroblasts, macrophages, mast cells, plasma cells * **Fibers**: collagen, elastic, reticular * **Ground substance**: proteoglycans, GAGs ### Types * **Loose CT**: areolar, adipose, reticular * **Dense CT**: regular, irregular, elastic * **Specialized CT**: cartilage, bone, blood --- ## Histology of Fibers ### Collagen Fibers * Thick, eosinophilic * High tensile strength * Seen in tendons, ligaments ### Elastic Fibers * Thin, branching * Stretch and recoil * Found in lungs, elastic arteries ### Reticular Fibers * Type III collagen * Supportive network * Seen in lymphoid organs --- ## Histology of Cartilage ### General Features * Avascular * Chondrocytes in **lacunae** * Perichondrium present (except articular cartilage) ### Types * **Hyaline cartilage**: trachea, articular surfaces * **Elastic cartilage**: pinna, epiglottis * **Fibrocartilage**: intervertebral discs, pubic symphysis --- ## Histology of Muscle Tissue ### Skeletal Muscle * Long cylindrical fibers * **Multinucleated**, peripheral nuclei * Cross striations present * Voluntary ### Cardiac Muscle * Branching fibers * Single central nucleus * **Intercalated discs** * Involuntary ### Smooth Muscle * Spindle-shaped cells * No striations * Involuntary * Found in viscera, vessels --- ## Histology of Lymphatic System ### Lymph Node * Capsule with trabeculae * **Cortex**: lymphoid follicles (B cells) * **Paracortex**: T cells * **Medulla**: medullary cords and sinuses ### Spleen * **White pulp**: lymphocytes around central artery * **Red pulp**: sinusoids and splenic cords ### Thymus * Cortex and medulla * **Hassall’s corpuscles** * T-cell maturation --- ## Histology of Gastrointestinal Tract (GIT) ### Common Layers 1. **Mucosa** – epithelium, lamina propria, muscularis mucosa 2. **Submucosa** – glands, Meissner plexus 3. **Muscularis externa** – Auerbach plexus 4. **Serosa/adventitia** ### Region-Specific Features * **Esophagus**: stratified squamous epithelium * **Stomach**: simple columnar epithelium, gastric glands * **Small intestine**: villi, plicae circulares, Peyer’s patches (ileum) * **Colon**: no villi, abundant goblet cells --- ## Histology of Liver ### Structural Unit * **Classical hepatic lobule** * Central vein * Portal triad: hepatic artery, portal vein, bile duct ### Cellular Features * Hepatocytes arranged in cords * **Sinusoids** lined by fenestrated endothelium * **Kupffer cells** – macrophages * **Space of Disse** ### Functional Significance * Metabolism * Detoxification * Bile production --- ## Histology of Respiratory Tract ### Trachea * Pseudostratified ciliated columnar epithelium * Goblet cells * C-shaped hyaline cartilage ### Bronchi * Cartilage plates * Smooth muscle layer * Mucous glands ### Bronchioles * No cartilage or glands * Simple ciliated columnar → cuboidal epithelium ### Alveoli * **Type I pneumocytes** – gas exchange * **Type II pneumocytes** – surfactant * Alveolar macrophages --- ## High-Yield Exam Pearls * Transitional epithelium is **unique to urinary tract** * Fibrocartilage **lacks perichondrium** * Peyer’s patches are characteristic of **ileum** * Kupffer cells are **liver macrophages** * Type II pneumocytes produce **surfactant** --- If you want, I can next: * ✅ Convert this into **HTML-CSS-JS single-file notes** * ✅ Add **labeled histology images** * ✅ Generate **25 image-based MCQs** * ✅ Create **printable PDF or exam charts** Just tell me 👍
Browse by Medical Category
Explore content organized by medical specialties and systems