nike – Profile
Streamora author since Jan 2026. This profile aggregates all their public posts and exam-oriented notes.
Public posts by this author
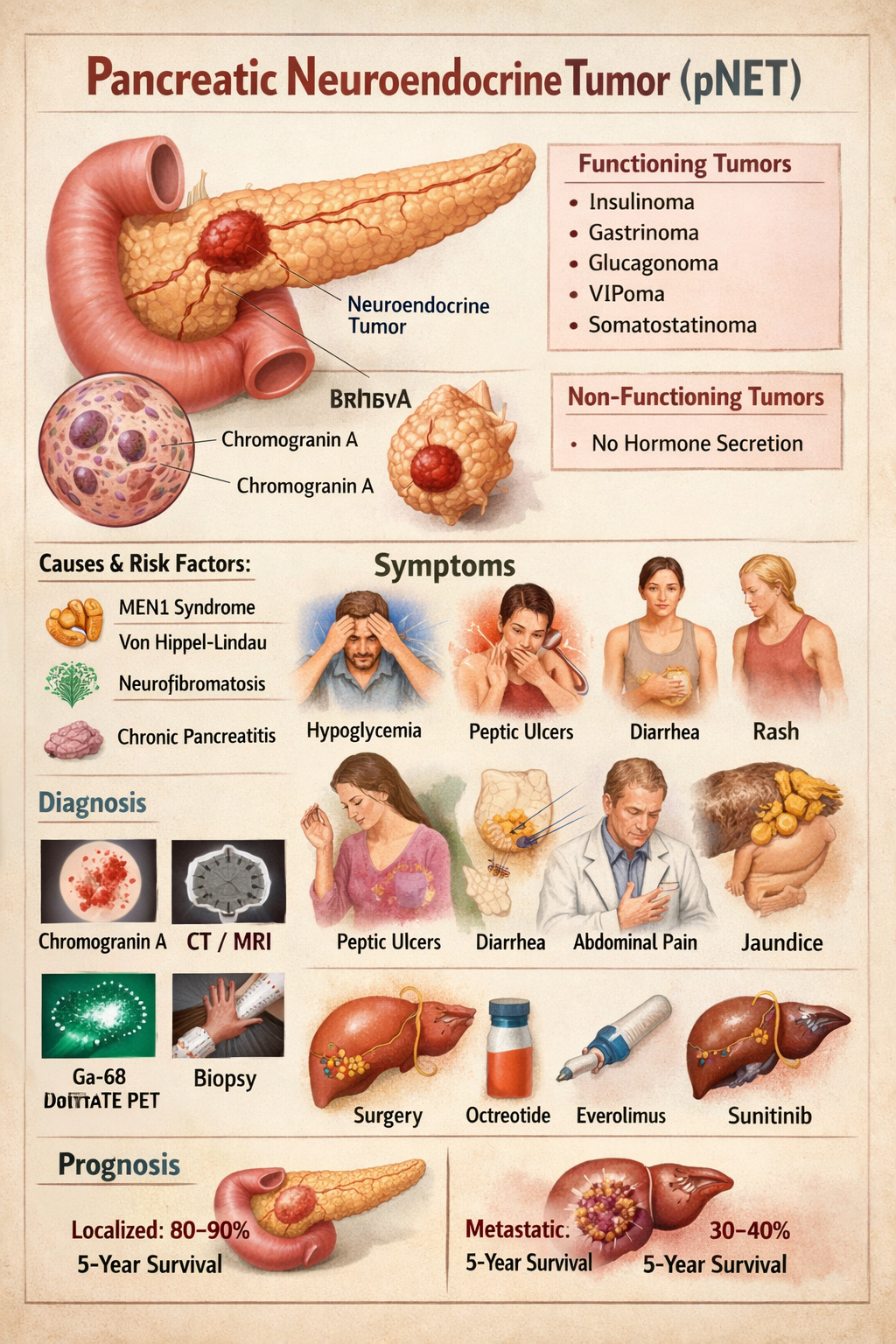
Pancreatic Neuroendocrine Tumor Symptoms Diagnosis Treatment Prognosis
--- # **PANCREATIC NEUROENDOCRINE TUMOR (pNET)** --- ## **1. Definition** Pancreatic neuroendocrine tumors (pNETs) are **neoplasms arising from endocrine (islet) cells of the pancreas** that secrete peptide hormones or amines. They are biologically distinct from pancreatic adenocarcinoma and may be **functioning (hormone-secreting)** or **non-functioning**. --- ## **2. Pathophysiology** pNETs originate from **enterochromaffin cells** of pancreatic islets. They show: * **Neuroendocrine differentiation** * **Dense-core secretory granules** * **Expression of chromogranin A and synaptophysin** Tumor behavior depends on: * **Hormone secretion** * **Tumor size** * **Ki-67 index (mitotic rate)** * **Invasion and metastasis** Tumors may be: * **Well differentiated (NET G1–G3)** * **Poorly differentiated (Neuroendocrine carcinoma)** MEN1 mutation commonly involved → parathyroid, pituitary, pancreas tumors. --- ## **3. Classification** ### **A. By hormone secretion** | Type | Hormone | | --------------- | ------------ | | Insulinoma | Insulin | | Gastrinoma | Gastrin | | Glucagonoma | Glucagon | | VIPoma | VIP | | Somatostatinoma | Somatostatin | | Non-functioning | None | ### **B. By WHO grading** | Grade | Ki-67 | | ----- | ----- | | G1 | <3% | | G2 | 3–20% | | G3 | >20% | --- ## **4. Causes and Risk Factors** * MEN-1 syndrome * Von Hippel–Lindau * Neurofibromatosis-1 * Tuberous sclerosis * Smoking * Chronic pancreatitis --- ## **5. Clinical Features** ### **A. Insulinoma** * Hypoglycemia * Sweating * Palpitations * Confusion * Weight gain ### **B. Gastrinoma (Zollinger-Ellison)** * Severe recurrent peptic ulcers * Diarrhea * GERD ### **C. Glucagonoma** * Diabetes * Necrolytic migratory erythema * Weight loss * Anemia ### **D. VIPoma** * Profuse watery diarrhea * Hypokalemia * Achlorhydria ### **E. Somatostatinoma** * Diabetes * Gallstones * Steatorrhea ### **F. Non-functioning** * Abdominal pain * Weight loss * Jaundice * Abdominal mass * Metastasis symptoms --- ## **6. Investigations** ### **Blood Tests** | Test | Use | | ------------------ | --------------- | | Chromogranin-A | Tumor marker | | Insulin, C-peptide | Insulinoma | | Gastrin | Gastrinoma | | Glucagon | Glucagonoma | | VIP | VIPoma | | Somatostatin | Somatostatinoma | | Fasting glucose | Hypoglycemia | ### **Imaging** * Contrast CT * MRI pancreas * Endoscopic ultrasound (best for small tumors) * Ga-68 DOTATATE PET-CT (gold standard) * Octreoscan ### **Biopsy** * EUS-guided biopsy * Ki-67 index --- ## **7. Differential Diagnosis** * Pancreatic adenocarcinoma * Islet cell hyperplasia * Metastatic carcinoid * Chronic pancreatitis * Insulin autoimmune syndrome --- ## **8. Management** ### **A. Curative – Surgery** * Enucleation (small insulinomas) * Distal pancreatectomy * Whipple procedure * Liver metastasis resection ### **B. Medical Therapy** Used when metastatic, unresectable or hormone excess. --- ## **9. Drugs Used** ### **1. Octreotide** **Indication:** Hormone control and tumor stabilization **Mechanism:** Somatostatin analog → inhibits hormone secretion **Dose:** Adult: 100–500 mcg SC 2–3 times/day or 20–30 mg IM monthly Paediatric: 1–10 mcg/kg/day **Adverse effects:** Gallstones, diarrhea, hyperglycemia **Contraindication:** Severe gallbladder disease **Monitoring:** LFT, glucose **Counsel:** May cause GI upset --- ### **2. Lanreotide** Same as octreotide Dose: 120 mg SC every 4 weeks --- ### **3. Everolimus** **Indication:** Advanced pNET **Mechanism:** mTOR inhibitor **Dose:** 10 mg daily **Adverse:** Mouth ulcers, hyperglycemia, infections **Contra:** Active infection **Monitor:** CBC, glucose **Counsel:** Avoid live vaccines --- ### **4. Sunitinib** **Indication:** Metastatic pNET **Mechanism:** VEGF receptor inhibitor **Dose:** 37.5 mg daily **Adverse:** Hypertension, fatigue **Contra:** Cardiac failure **Monitor:** BP, ECG --- ### **5. Diazoxide (for insulinoma)** **Mechanism:** Inhibits insulin release **Dose:** 100–600 mg/day **Adverse:** Fluid retention, hyperglycemia **Monitor:** Glucose, edema --- ### **6. Streptozocin + 5-FU (Chemotherapy)** **Indication:** High-grade metastatic disease **Adverse:** Nephrotoxicity, nausea --- ## **10. Non-Pharmacologic** * Surgical resection * Radiofrequency ablation of liver mets * Peptide receptor radionuclide therapy (PRRT) * Dietary glucose support in insulinoma --- ## **11. Prognosis** * Localized pNET: 80–90% 5-year survival * Metastatic: 30–40% Better than pancreatic adenocarcinoma --- ## **12. Key Exam Points** * Insulinoma = most common pNET * Gastrinoma = most malignant * MEN1 = 3 P’s: Parathyroid, Pituitary, Pancreas * Chromogranin A is universal tumor marker * Ga-68 DOTATATE PET = best imaging ---
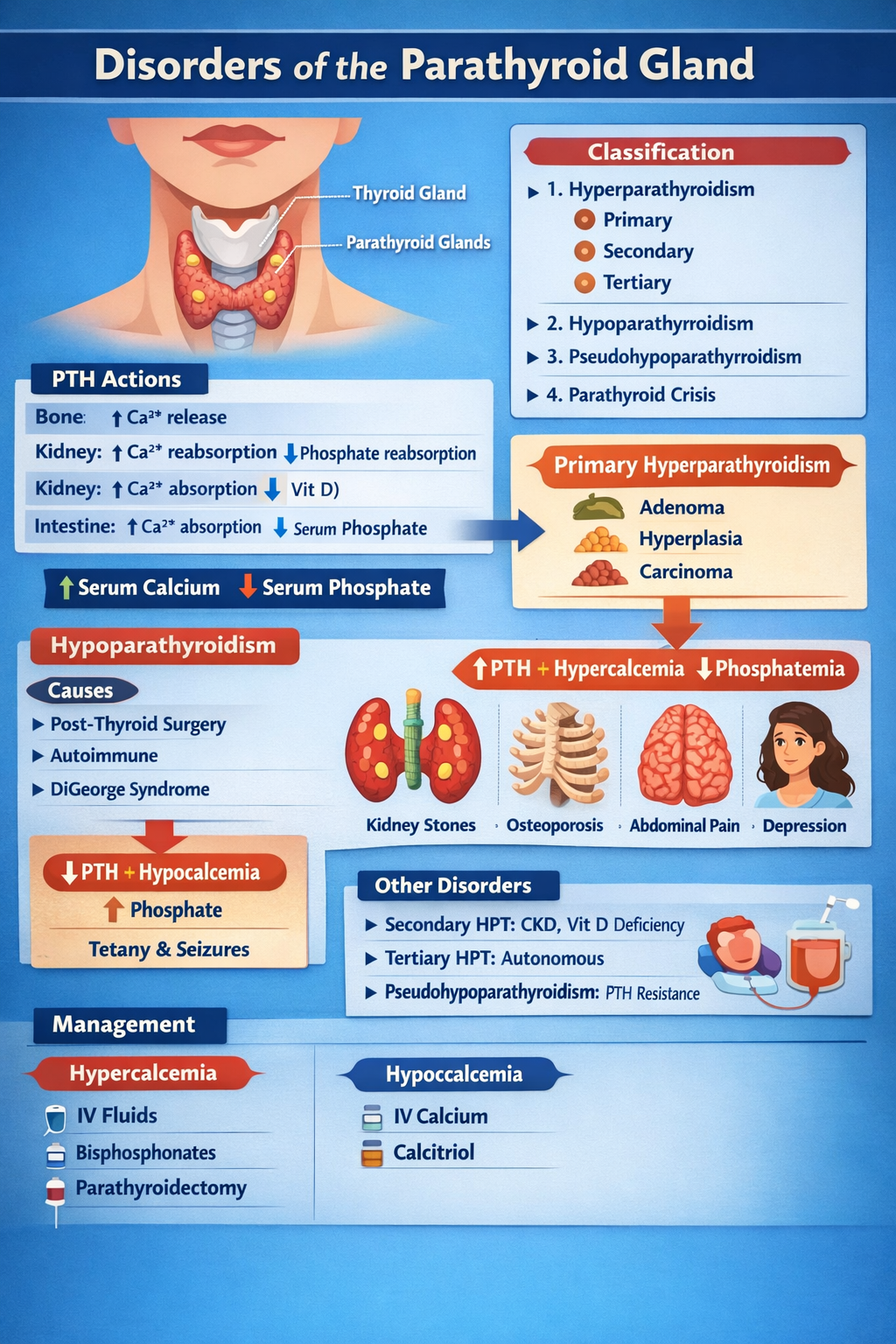
Disorders of Parathyroid Gland Complete Clinical Guide for Medical Students
--- # **DISORDERS OF THE PARATHYROID GLAND** --- ## **1. Physiology of Parathyroid Hormone (PTH)** **Parathyroid glands (4)** → secrete **PTH** → maintain **serum calcium and phosphate balance** ### **Normal actions of PTH** | Target organ | Action | | ------------- | ----------------------------------------------- | | **Bone** | ↑ Osteoclastic bone resorption → ↑ Ca²⁺ release | | **Kidney** | ↑ Ca²⁺ reabsorption, ↓ phosphate reabsorption | | **Kidney** | ↑ 1-α hydroxylase → ↑ calcitriol | | **Intestine** | Indirectly ↑ Ca²⁺ absorption via vitamin D | **Net effect:** **↑ Serum calcium, ↓ serum phosphate** --- # **CLASSIFICATION** 1. **Hyperparathyroidism** * Primary * Secondary * Tertiary 2. **Hypoparathyroidism** 3. **Pseudohypoparathyroidism** 4. **Parathyroid crisis** --- # **PRIMARY HYPERPARATHYROIDISM (PHPT)** ## **Definition** Autonomous excessive PTH secretion → **hypercalcemia** ## **Causes** | Cause | % | | ----------------------- | ------ | | Parathyroid adenoma | 85% | | Parathyroid hyperplasia | 10–15% | | Parathyroid carcinoma | <1% | | MEN-1, MEN-2A | Rare | --- ## **Pathophysiology** Excess PTH → * ↑ Bone resorption → osteoporosis * ↑ Renal Ca reabsorption * ↑ Vitamin D → ↑ gut Ca absorption → **Hypercalcemia + hypophosphatemia** --- ## **Clinical Features** **“Stones, Bones, Groans, Thrones, Psychiatric Overtones”** | System | Features | | ------ | ---------------------------------------------- | | Kidney | Nephrolithiasis, polyuria | | Bone | Bone pain, fractures, osteitis fibrosa cystica | | GIT | Constipation, pancreatitis, peptic ulcer | | CNS | Depression, confusion | | Heart | Short QT | --- ## **Investigations** | Test | Result | | -------------------- | ---------------- | | Serum Ca | ↑ | | Serum phosphate | ↓ | | PTH | ↑ | | ALP | ↑ | | 24-hr urine Ca | ↑ | | DEXA | Osteoporosis | | Neck USG / Sestamibi | Localize adenoma | --- ## **Differential Diagnosis** | Condition | PTH | Ca | | ------------------------ | --- | -------- | | PHPT | ↑ | ↑ | | Malignancy hypercalcemia | ↓ | ↑ | | FHH | ↑ | Normal/↑ | --- ## **Management** ### **A. Acute hypercalcemia** | Step | Treatment | | ---- | ----------------- | | 1 | IV normal saline | | 2 | Loop diuretic | | 3 | IV bisphosphonate | | 4 | Calcitonin | ### **B. Definitive** **Parathyroidectomy** **Indications** * Ca >1 mg/dL above normal * Kidney stones * Osteoporosis * Age <50 --- # **SECONDARY HYPERPARATHYROIDISM** ## **Definition** Compensatory ↑ PTH due to **hypocalcemia** ## **Causes** * Chronic kidney disease (most common) * Vitamin D deficiency * Malabsorption --- ## **Biochemistry** | Parameter | Result | | --------- | ---------- | | Calcium | ↓ | | Phosphate | ↑ (in CKD) | | PTH | ↑ | | Vitamin D | ↓ | --- ## **Management** * Oral calcium * Vitamin D (calcitriol) * Phosphate binders * Dialysis if CKD --- # **TERTIARY HYPERPARATHYROIDISM** Long-standing secondary → autonomous glands | Ca | PTH | | -- | --- | | ↑ | ↑ | **Treatment:** Parathyroidectomy --- # **HYPOPARATHYROIDISM** ## **Definition** Deficient PTH → hypocalcemia ## **Causes** * Post-thyroid surgery (most common) * Autoimmune * DiGeorge syndrome * Hypomagnesemia --- ## **Pathophysiology** Low PTH → ↓ calcium, ↑ phosphate → neuromuscular excitability --- ## **Clinical Features** | Feature | Mechanism | | --------------- | ------------------------------ | | Tetany | Hypocalcemia | | Chvostek sign | Facial nerve hyperexcitability | | Trousseau sign | Carpopedal spasm | | Seizures | Low Ca | | QT prolongation | Hypocalcemia | --- ## **Investigations** | Test | Result | | --------- | -------- | | Ca | ↓ | | Phosphate | ↑ | | PTH | ↓ | | Mg | May be ↓ | --- ## **Management** ### **Acute** IV **calcium gluconate** ### **Chronic** * Oral calcium * Calcitriol --- # **CALCIUM GLUCONATE** | Parameter | Value | | ------------ | -------------------- | | Indication | Acute tetany | | Mechanism | Raises serum Ca | | Dose | 10 ml of 10% IV slow | | Side effects | Arrhythmia | | Monitoring | ECG | --- # **CALCITRIOL (Vitamin D)** | Feature | Detail | | ------------ | -------------------------- | | Action | ↑ Intestinal Ca absorption | | Dose | 0.25–1 mcg/day | | Side effects | Hypercalcemia | | Monitoring | Serum Ca | --- # **PSEUDOHYPOPARATHYROIDISM** ## **Definition** Target organ resistance to PTH | Ca | PTH | Phosphate | | -- | --- | --------- | | ↓ | ↑ | ↑ | ## **Clinical** * Short stature * Round face * Brachydactyly * Mental retardation **Treatment:** Calcium + Vitamin D --- # **PARATHYROID CRISIS** Severe hypercalcemia (>14 mg/dL) ### **Features** * Dehydration * Arrhythmia * Coma ### **Management** 1. IV saline 2. Loop diuretic 3. Calcitonin 4. Bisphosphonates 5. Dialysis if refractory --- # **EXAM PEARLS** | Scenario | Diagnosis | | --------------------------------- | --------------------------- | | High Ca + high PTH | Primary hyperparathyroidism | | Low Ca + high PTH | Secondary HPT | | Low Ca + low PTH | Hypoparathyroidism | | Low Ca + high PTH + short fingers | Pseudohypoparathyroidism | ---
Explore More
- Home Latest medical posts
- Sitelinks Index Complete site map
- Upload Medical Content Share clinical pearls
- Reviews & Suggestions Community feedback
- Help & FAQ Upload & SEO tips
- About Streamora Medical learning hub
- Contact Admin Support & queries
- All Medical Authors Browse all contributors