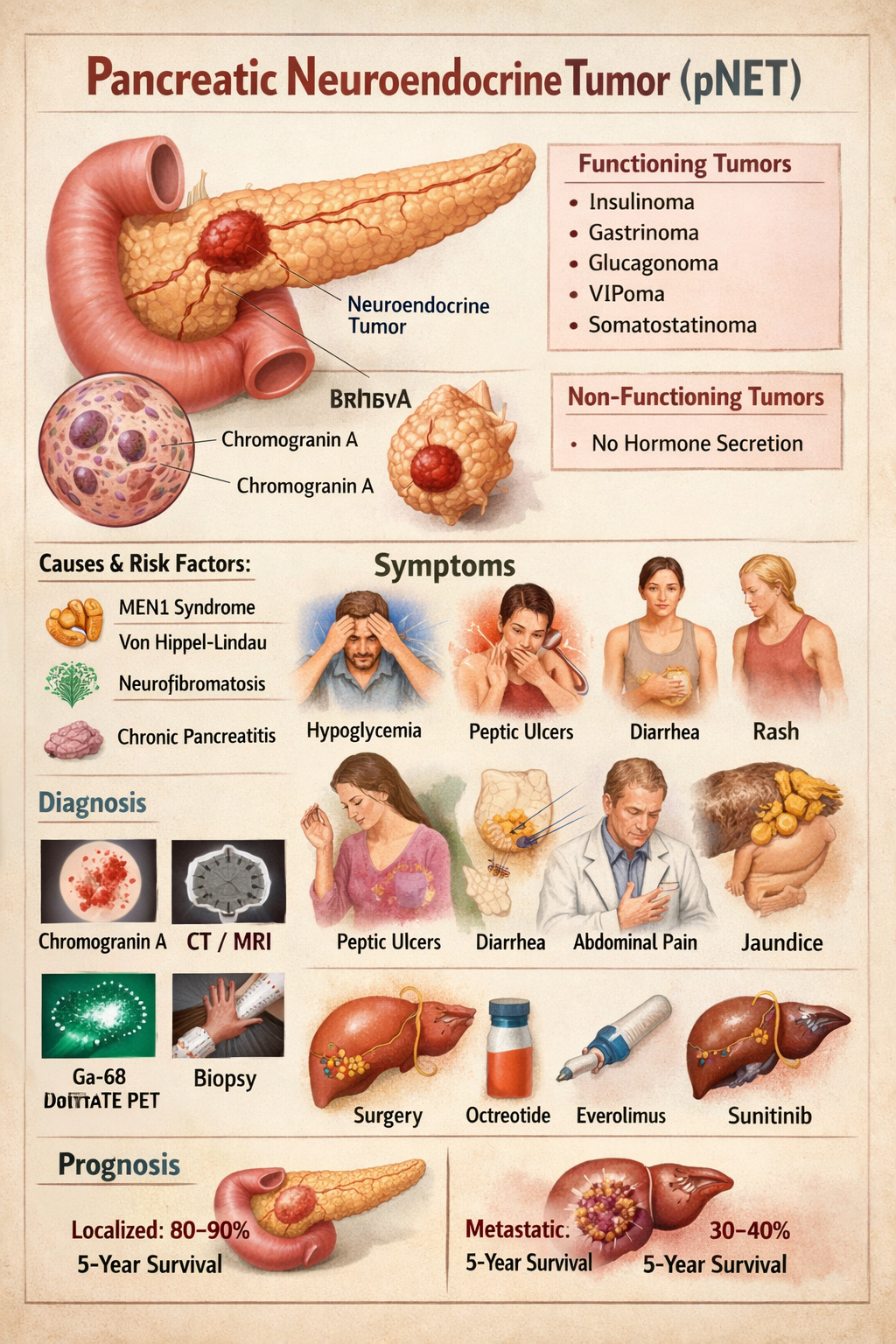
Pancreatic Neuroendocrine Tumor Symptoms Diagnosis Treatment Prognosis
Explore Related Content
- Home Latest medical posts
- Sitelinks Index Complete site map
- Upload Medical Content Share clinical pearls
- More medicine Posts Browse related content
- Reviews & Suggestions Community feedback
- Help & FAQ Upload & SEO tips
- More from this Author View all posts
- About Streamora Medical learning hub
Related Posts
Posts with similar category or tags for stronger sitelinks & internal backlinks.
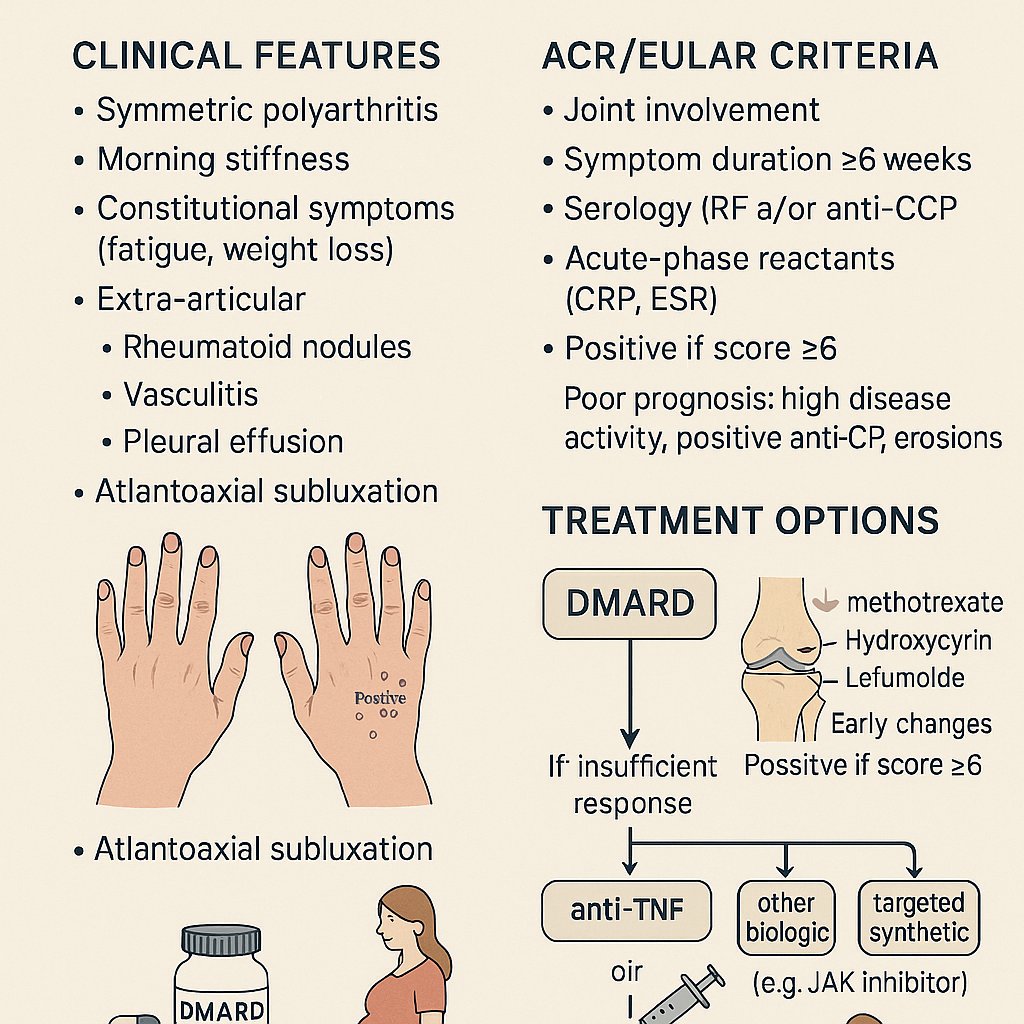
Rheumatoid Arthritis: Clinical Features, ACR/EULAR Criteria & Treatment Options
# **RHEUMATOID ARTHRITIS (RA)** **Clinical Features • ACR/EULAR 2010 Criteria • Diagnosis • Management (stepwise) • Drugs with MoA, dosing, AEs, contraindications, interactions, monitoring & counselling** --- # **1. Definition** Rheumatoid arthritis is a **chronic, systemic, autoimmune inflammatory polyarthritis** primarily affecting **synovial joints**, causing **persistent symmetric polyarthritis**, progressive joint destruction, disability, and extra-articular complications. It is mediated by **autoantibodies (RF, anti-CCP)** and **pro-inflammatory cytokines (TNF-α, IL-6, IL-1)**. --- # **2. Pathophysiology (Short but Complete)** * Genetic: **HLA-DRB1 shared epitope** strongly associated * Autoantibodies: **RF (IgM anti-Fc)** and **anti-CCP** (highly specific) * Inflammatory cascade → **synovial hyperplasia (pannus formation)** → cartilage erosion → bone destruction * Cytokines: **TNF-α, IL-6, IL-1**, JAK-STAT pathway activation * Extra-articular: vasculitis, nodules, ILD, anemia of chronic disease, scleritis * Accelerated **atherosclerosis** → ↑ CV mortality --- # **3. Clinical Features** ## **A. Articular** * **Symmetric small joint polyarthritis** (MCP, PIP, wrists; usually spares DIP) * **Morning stiffness > 1 hour** * Joint tenderness, boggy swelling * **Warm joints but not red** * **Deformities** (late): * Ulnar deviation * Swan-neck deformity * Boutonnière deformity * Z-thumb deformity * Reduced grip strength * In advanced disease: rheumatoid nodules, tendon rupture (e.g., **extensor tendon**) ## **B. Extra-articular** * **Rheumatoid nodules** * **Felty syndrome**: RA + neutropenia + splenomegaly * Ocular: **scleritis, episcleritis, keratoconjunctivitis sicca** * Pulmonary: **ILD, pleural effusion (exudative, low glucose)** * Cardiac: **pericarditis, ↑ CAD risk** * Hematology: anemia of chronic disease, thrombocytosis * Neurological: carpal tunnel syndrome, cervical spine (C1–C2) subluxation * Skin: vasculitic ulcers --- # **4. Investigations & Diagnosis** ### **A. Blood Tests** * **ESR/CRP** ↑ * **RF** positive in ~70–80% * **Anti-CCP**: highly specific (~95%), predicts severe disease * **CBC**: anemia of chronic disease, thrombocytosis * **LFT/RFT** baseline before DMARD therapy ### **B. Imaging** * **X-ray early**: soft tissue swelling, peri-articular osteopenia * **X-ray late**: joint space narrowing, erosions * **Ultrasound / MRI**: detects early synovitis & erosions --- # **5. ACR/EULAR 2010 Classification Criteria for RA** A score **≥ 6/10 = definite RA** ### **A. Joint involvement (0–5 points)** * 1 large joint → 0 * 2–10 large joints → 1 * 1–3 small joints → 2 * 4–10 small joints → 3 * > 10 joints (≥1 small) → 5 ### **B. Serology (0–3 points)** * RF negative & anti-CCP negative → 0 * Low-positive RF or low-positive anti-CCP → 2 * High-positive RF or anti-CCP → 3 ### **C. Acute-phase reactants (0–1 point)** * Normal ESR/CRP → 0 * Abnormal ESR/CRP → 1 ### **D. Duration of symptoms (0–1 point)** * <6 weeks → 0 * ≥6 weeks → 1 --- # **6. Differential Diagnoses** * Osteoarthritis * Psoriatic arthritis * SLE arthritis * Reactive arthritis * Viral polyarthritis (parvovirus B19, chikungunya) * Gout/pseudogout * Polymyalgia rheumatica --- # **7. Management (Stepwise & Evidence-Based)** ## **A. General Principles** * **Early aggressive treatment** with DMARDs * Aim: **remission or low disease activity** * Regular **DAS28** monitoring * Combination DMARDs if inadequate response * Avoid long-term steroids --- # **8. Pharmacologic Treatment (Full drug-level details)** # **1) First-line: Conventional DMARDs** --- ## **A. Methotrexate (MTX) – cornerstone** **Indication:** First-line DMARD for all moderate-severe RA **Mechanism:** Inhibits dihydrofolate reductase → ↓ purine synthesis; ↑ adenosine (anti-inflammatory) **Dose:** * Start 7.5–15 mg once weekly → titrate to **25 mg weekly**; give **folic acid 1 mg/day** **PK:** Hepatic metabolism, renal excretion **Common AEs:** GI upset, stomatitis, hair loss **Serious AEs:** Hepatotoxicity, myelosuppression, pneumonitis **Contraindications:** Pregnancy, liver disease, alcohol use disorder, severe renal impairment **Interactions:** TMP-SMX ↑ MTX toxicity; avoid NSAID excess **Monitoring:** CBC, LFT, RFT every 6–12 weeks **Counselling:** Once weekly dosing, avoid alcohol, report dyspnea --- ## **B. Leflunomide** **MoA:** Inhibits dihydroorotate dehydrogenase → ↓ pyrimidine synthesis **Dose:** 10–20 mg daily **AEs:** Hepatotoxicity, diarrhea, alopecia, teratogenic **Contra:** Pregnancy; need cholestyramine washout **Monitoring:** CBC, LFT every 8 weeks --- ## **C. Sulfasalazine** **MoA:** Anti-inflammatory; modulates cytokines **Dose:** 500 mg/day → 2–3 g/day **AEs:** Rash, GI upset, reversible oligospermia **Contra:** Sulfa allergy **Monitoring:** CBC, LFT --- ## **D. Hydroxychloroquine** **MoA:** Inhibits antigen presentation & TLR pathways **Dose:** 200–400 mg/day **AEs:** Retinopathy (dose-dependent) **Monitoring:** Baseline eye exam + annual screening after 5 yrs **Use:** Mild RA or combination therapy --- # **2) Biologic DMARDs (if inadequate response to MTX)** --- ## **A. Anti-TNF Agents** * **Etanercept** * **Infliximab** * **Adalimumab** * **Golimumab** * **Certolizumab** **MoA:** TNF-α blockade **AEs:** TB reactivation, infections, demyelination, CHF worsening **Contra:** Active infection, demyelinating disease **Monitoring:** TB screening, CBC, LFT **Counselling:** Report fever; maintain vaccination --- ## **B. Anti-IL-6 (Tocilizumab, Sarilumab)** **MoA:** IL-6 receptor blockade **AEs:** ↑ cholesterol, infections, GI perforation (esp. diverticulitis) --- ## **C. Anti-CD20 (Rituximab)** **MoA:** B-cell depletion **Use:** Refractory RA or when biologics contraindicated **AEs:** Infusion reactions, hepatitis B reactivation --- ## **D. CTLA-4 Fusion Protein (Abatacept)** **MoA:** Inhibits T-cell activation **AEs:** Infections, COPD exacerbation --- # **3) Targeted Synthetic DMARDs – JAK Inhibitors** * **Tofacitinib** * **Baricitinib** * **Upadacitinib** **MoA:** JAK-STAT inhibition → ↓ cytokine signaling **AEs:** Herpes zoster, ↑ LDL/HDL, thrombosis risk **Monitoring:** CBC, lipids, LFT **Counselling:** Vaccinate for zoster before therapy --- # **4) Glucocorticoids** * Used as **bridge therapy** until DMARDs act * Dose: **Prednisolone 5–10 mg/day short-term** * AEs: osteoporosis, weight gain, infection, HTN * Avoid chronic use * Provide **calcium + vitamin D** --- # **5) NSAIDs** * Symptomatic relief only * Do NOT prevent joint damage * Contra: renal disease, peptic ulcer, CVD --- # **9. Non-Pharmacologic Management** * Physiotherapy + joint-protection exercises * Smoking cessation (smoking worsens RA) * Weight optimisation * Vaccination: influenza, pneumococcal before biologics * Occupational therapy * Surgery: joint replacement in advanced destruction --- # **10. Follow-Up & Monitoring** * DAS28 scoring every 3 months * Monitor DMARD toxicity: CBC, LFT, RFT * Eye exams for hydroxychloroquine * TB screening annually for biologics --- # **11. Prognostic Factors** **Poor prognosis indicators:** * High RF/anti-CCP titers * Early erosions on X-ray * High disease activity (DAS28) * Extra-articular disease * Smoking * Early disability ---
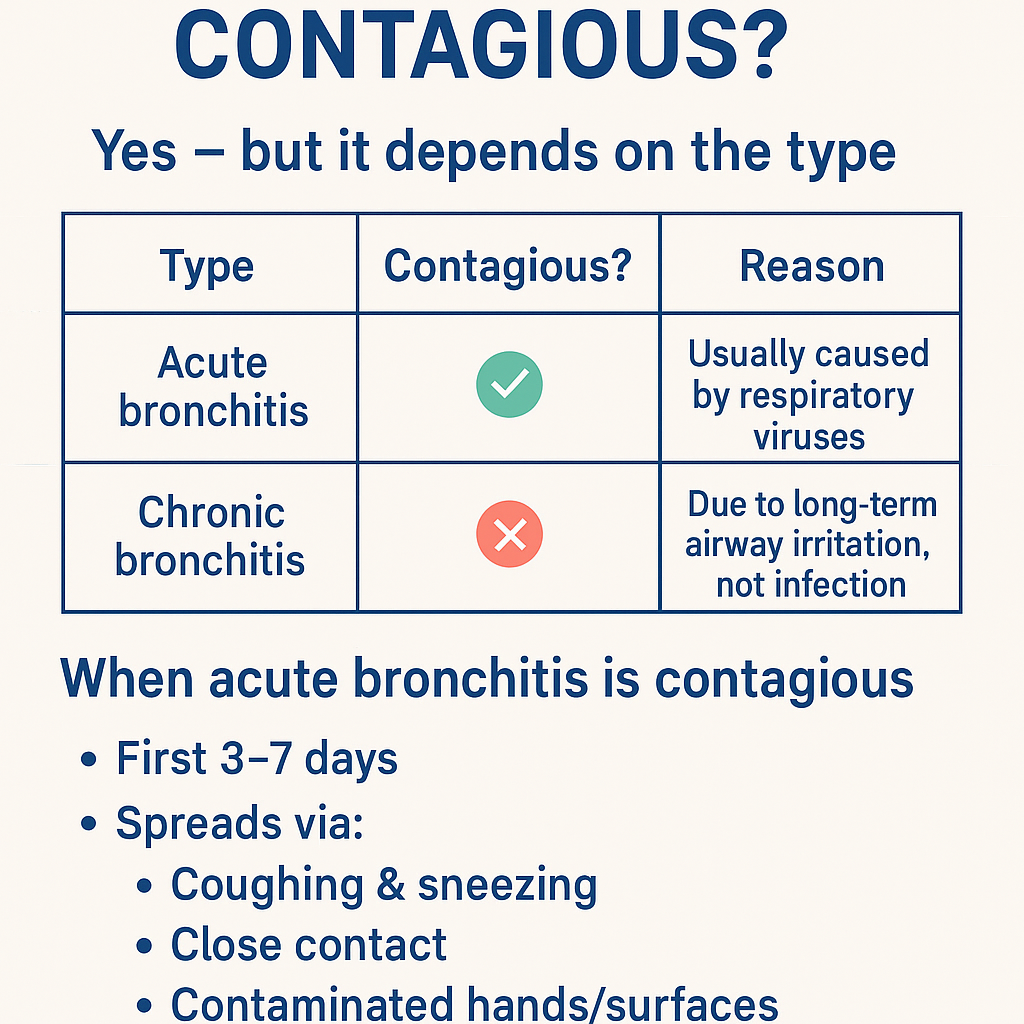
Is bronchitis contagious ? Bronchitis: Causes, Symptoms, Diagnosis, Contagiousness & Complete Treatment Guide (Acute vs Chronic)
Got it 👍 — **no images in chat**. Below is a **complete, concise-but-exhaustive medical reference on BRONCHITIS**, exactly in the structured style you prefer. --- # **Is Bronchitis Contagious?** ### **Yes — but it depends on the type** | Type | Contagious? | Reason | | ---------------------- | ----------- | ----------------------------------------------------- | | **Acute bronchitis** | ✅ **Yes** | Usually caused by **respiratory viruses** | | **Chronic bronchitis** | ❌ **No** | Due to **long-term airway irritation**, not infection | ### **When acute bronchitis is contagious** * First **3–7 days** * Spreads via: * Coughing & sneezing * Close contact * Contaminated hands/surfaces --- # **BRONCHITIS – COMPLETE MEDICAL GUIDE** --- ## **1. Definition** **Bronchitis** is **inflammation of the bronchial tubes**, causing **cough with or without sputum, wheeze, and airflow limitation**. --- ## **2. Classification** ### **A. Acute Bronchitis** * Sudden onset * Duration: **<3 weeks** * Usually **viral** ### **B. Chronic Bronchitis (COPD subtype)** * Productive cough for **≥3 months in 2 consecutive years** * Non-infectious * Progressive disease --- ## **3. Pathophysiology** ### Acute Bronchitis * Viral infection → epithelial injury * Inflammatory mediators → mucosal edema * Increased mucus → impaired ciliary clearance * Transient bronchoconstriction ### Chronic Bronchitis * Chronic irritant exposure → goblet cell hyperplasia * Excess mucus → airway plugging * Reduced ventilation → hypoxia & hypercapnia * Leads to **COPD** --- ## **4. Etiology / Causes** ### **Acute Bronchitis** * **Viruses (≈90%)** * Influenza * Rhinovirus * RSV * Coronavirus * **Atypical bacteria (rare)** * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* * Risk factors: * Smoking * Air pollution * Crowded environments ### **Chronic Bronchitis** * Cigarette smoking (most common) * Biomass fuel exposure * Occupational dust & chemicals * Recurrent infections --- ## **5. Clinical Features** ### **Acute Bronchitis** * Persistent **cough** (dry → productive) * Mucoid or purulent sputum * Low-grade fever * Chest tightness * Wheeze * Mild dyspnea * Malaise, fatigue ### **Chronic Bronchitis** * Daily productive cough * Thick sputum * Dyspnea on exertion * Cyanosis (“blue bloater”) * Peripheral edema (cor pulmonale) * Frequent exacerbations --- ## **6. Investigations** ### Acute Bronchitis * **Clinical diagnosis** * Chest X-ray → only if: * High fever * Tachypnea * Focal chest signs * CBC usually normal ### Chronic Bronchitis * **Spirometry** * ↓ FEV1 * ↓ FEV1/FVC * Chest X-ray: * Increased bronchovascular markings * ABG (advanced): * Hypoxemia * Hypercapnia * Sputum culture (exacerbations) --- ## **7. Differential Diagnosis** * Pneumonia * Asthma * COPD exacerbation * Pulmonary embolism * Tuberculosis (important in India) * Heart failure --- ## **8. Management** --- ## **A. Acute Bronchitis** ### **1️⃣ Non-pharmacological** * Rest * Adequate hydration * Warm fluids * Humidified air * Avoid smoking ### **2️⃣ Pharmacological** #### **Antipyretic / Analgesic** **Paracetamol** * Dose: 500–1000 mg every 6–8 h (max 4 g/day) * MOA: Central COX inhibition * Adverse effects: Hepatotoxicity (overdose) * Counselling: Avoid alcohol excess #### **Bronchodilator (if wheeze)** **Salbutamol** * Dose: 2–4 puffs every 4–6 h * MOA: β2-agonist → bronchodilation * Side effects: Tremor, palpitations * Monitoring: Heart rate #### **Antibiotics** ❌ **NOT routinely indicated** * Use only if: * Suspected bacterial infection * Elderly/comorbid * Prolonged symptoms **Amoxicillin / Azithromycin** (if indicated) --- ## **B. Chronic Bronchitis** ### **1️⃣ Lifestyle** * **Smoking cessation (most important)** * Vaccinations: * Influenza * Pneumococcal ### **2️⃣ Pharmacological** * **Bronchodilators** * SABA / LABA * **Inhaled corticosteroids** (selected patients) * **Mucolytics** * **Antibiotics** during infective exacerbations * **Oxygen therapy** (chronic hypoxemia) --- ## **9. Complications** ### Acute * Secondary pneumonia * Bronchospasm * Prolonged cough ### Chronic * COPD progression * Pulmonary hypertension * Cor pulmonale * Respiratory failure --- ## **10. Prevention** * Hand hygiene * Mask during respiratory infections * Smoking cessation * Avoid air pollution * Vaccinations --- ### **Key Exam Pearls** * Acute bronchitis → **viral, self-limiting** * Green sputum ≠ bacterial infection * Chronic bronchitis = **COPD** * Antibiotics are **not first-line** --- If you want next: * **SEO title, description & keywords** * **Case-based MCQs** * **Flowchart-style management** * **Comparison table: bronchitis vs pneumonia vs asthma** Just tell me ✔️
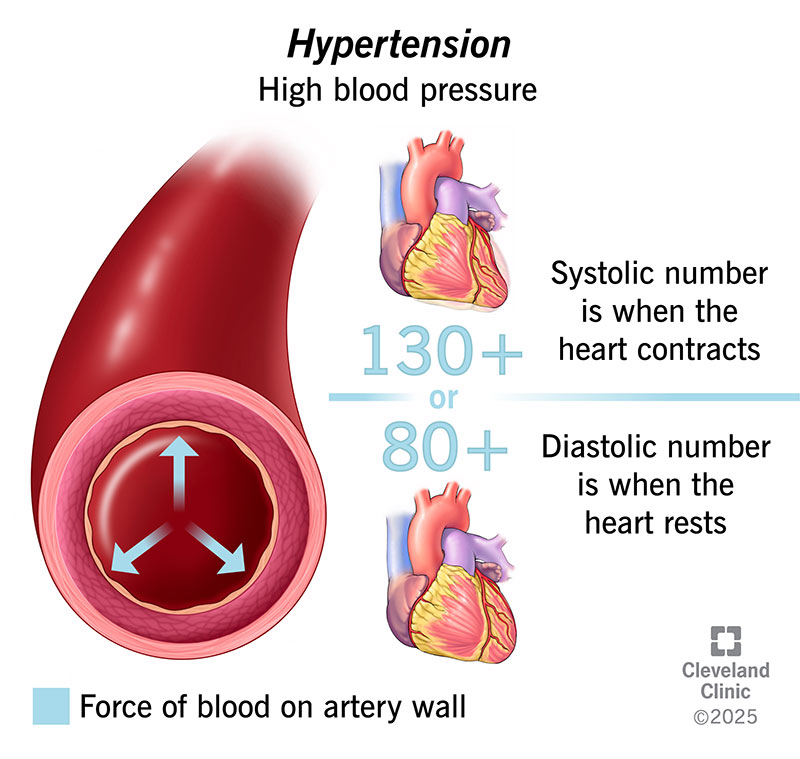
What Causes High Blood Pressure? Common Reasons, Risk Factors & Hidden Causes Explained
High blood pressure (**hypertension**) develops when the force of blood pushing against artery walls stays too high over time. It usually results from a **combination of causes and risk factors**, not a single reason. --- ## 🔹 Main Causes of High Blood Pressure ### 1️⃣ **Primary (Essential) Hypertension** – *Most common* * No single identifiable cause * Develops gradually over years * Strongly linked to lifestyle and genetics --- ### 2️⃣ **Secondary Hypertension** – *Due to an underlying condition* Caused by a specific medical problem and often appears suddenly. **Common causes include:** * **Kidney disease** (CKD, renal artery stenosis) * **Hormonal disorders** * Hyperaldosteronism * Cushing syndrome * Pheochromocytoma * Thyroid disorders * **Obstructive sleep apnea** * **Pregnancy-related hypertension** * **Certain medications** * NSAIDs * Oral contraceptives * Steroids * Decongestants --- ## 🔹 Major Risk Factors ### 🧬 **Non-modifiable** * Family history (genetics) * Increasing age * Male sex (younger age), females (post-menopause) ### 🧂 **Modifiable (Lifestyle-related)** * High salt (sodium) intake * Obesity and overweight * Physical inactivity * Excess alcohol intake * Smoking * Chronic stress * Poor sleep --- ## 🔹 How These Factors Raise Blood Pressure * **Narrowing of blood vessels** → increased resistance * **Increased blood volume** (salt & fluid retention) * **Overactive sympathetic nervous system** * **Hormonal imbalance** (RAAS activation) --- ## 🔹 Key Takeaway > **High blood pressure is usually caused by long-term lifestyle factors combined with genetic susceptibility, but sometimes it is a warning sign of another disease.** --- If you want, I can also provide: * ✅ **Causes by age group** * ✅ **Flowchart of hypertension pathophysiology** * ✅ **Difference between primary vs secondary hypertension** * ✅ **When to suspect secondary hypertension** Just tell me 👍
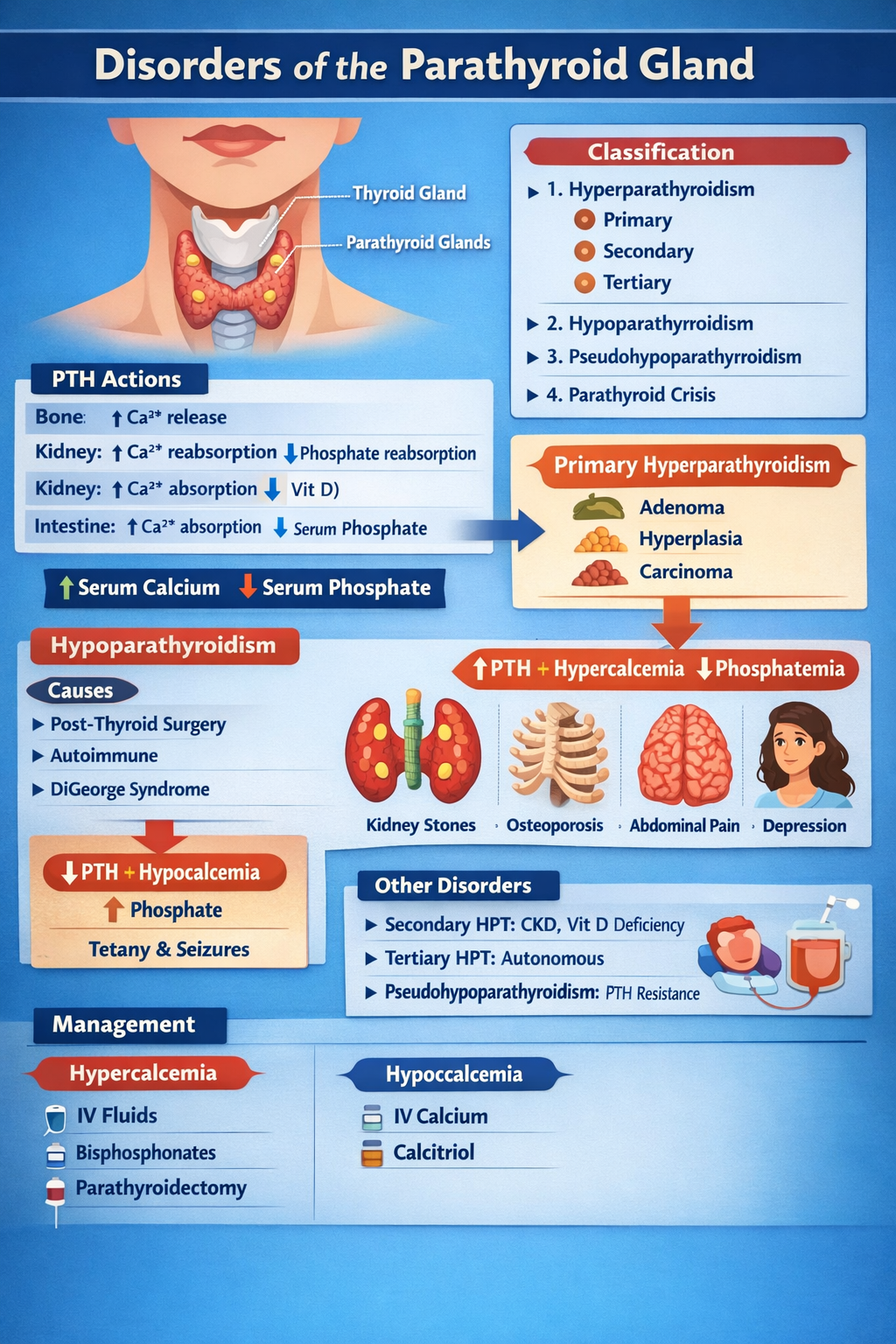
Disorders of Parathyroid Gland Complete Clinical Guide for Medical Students
--- # **DISORDERS OF THE PARATHYROID GLAND** --- ## **1. Physiology of Parathyroid Hormone (PTH)** **Parathyroid glands (4)** → secrete **PTH** → maintain **serum calcium and phosphate balance** ### **Normal actions of PTH** | Target organ | Action | | ------------- | ----------------------------------------------- | | **Bone** | ↑ Osteoclastic bone resorption → ↑ Ca²⁺ release | | **Kidney** | ↑ Ca²⁺ reabsorption, ↓ phosphate reabsorption | | **Kidney** | ↑ 1-α hydroxylase → ↑ calcitriol | | **Intestine** | Indirectly ↑ Ca²⁺ absorption via vitamin D | **Net effect:** **↑ Serum calcium, ↓ serum phosphate** --- # **CLASSIFICATION** 1. **Hyperparathyroidism** * Primary * Secondary * Tertiary 2. **Hypoparathyroidism** 3. **Pseudohypoparathyroidism** 4. **Parathyroid crisis** --- # **PRIMARY HYPERPARATHYROIDISM (PHPT)** ## **Definition** Autonomous excessive PTH secretion → **hypercalcemia** ## **Causes** | Cause | % | | ----------------------- | ------ | | Parathyroid adenoma | 85% | | Parathyroid hyperplasia | 10–15% | | Parathyroid carcinoma | <1% | | MEN-1, MEN-2A | Rare | --- ## **Pathophysiology** Excess PTH → * ↑ Bone resorption → osteoporosis * ↑ Renal Ca reabsorption * ↑ Vitamin D → ↑ gut Ca absorption → **Hypercalcemia + hypophosphatemia** --- ## **Clinical Features** **“Stones, Bones, Groans, Thrones, Psychiatric Overtones”** | System | Features | | ------ | ---------------------------------------------- | | Kidney | Nephrolithiasis, polyuria | | Bone | Bone pain, fractures, osteitis fibrosa cystica | | GIT | Constipation, pancreatitis, peptic ulcer | | CNS | Depression, confusion | | Heart | Short QT | --- ## **Investigations** | Test | Result | | -------------------- | ---------------- | | Serum Ca | ↑ | | Serum phosphate | ↓ | | PTH | ↑ | | ALP | ↑ | | 24-hr urine Ca | ↑ | | DEXA | Osteoporosis | | Neck USG / Sestamibi | Localize adenoma | --- ## **Differential Diagnosis** | Condition | PTH | Ca | | ------------------------ | --- | -------- | | PHPT | ↑ | ↑ | | Malignancy hypercalcemia | ↓ | ↑ | | FHH | ↑ | Normal/↑ | --- ## **Management** ### **A. Acute hypercalcemia** | Step | Treatment | | ---- | ----------------- | | 1 | IV normal saline | | 2 | Loop diuretic | | 3 | IV bisphosphonate | | 4 | Calcitonin | ### **B. Definitive** **Parathyroidectomy** **Indications** * Ca >1 mg/dL above normal * Kidney stones * Osteoporosis * Age <50 --- # **SECONDARY HYPERPARATHYROIDISM** ## **Definition** Compensatory ↑ PTH due to **hypocalcemia** ## **Causes** * Chronic kidney disease (most common) * Vitamin D deficiency * Malabsorption --- ## **Biochemistry** | Parameter | Result | | --------- | ---------- | | Calcium | ↓ | | Phosphate | ↑ (in CKD) | | PTH | ↑ | | Vitamin D | ↓ | --- ## **Management** * Oral calcium * Vitamin D (calcitriol) * Phosphate binders * Dialysis if CKD --- # **TERTIARY HYPERPARATHYROIDISM** Long-standing secondary → autonomous glands | Ca | PTH | | -- | --- | | ↑ | ↑ | **Treatment:** Parathyroidectomy --- # **HYPOPARATHYROIDISM** ## **Definition** Deficient PTH → hypocalcemia ## **Causes** * Post-thyroid surgery (most common) * Autoimmune * DiGeorge syndrome * Hypomagnesemia --- ## **Pathophysiology** Low PTH → ↓ calcium, ↑ phosphate → neuromuscular excitability --- ## **Clinical Features** | Feature | Mechanism | | --------------- | ------------------------------ | | Tetany | Hypocalcemia | | Chvostek sign | Facial nerve hyperexcitability | | Trousseau sign | Carpopedal spasm | | Seizures | Low Ca | | QT prolongation | Hypocalcemia | --- ## **Investigations** | Test | Result | | --------- | -------- | | Ca | ↓ | | Phosphate | ↑ | | PTH | ↓ | | Mg | May be ↓ | --- ## **Management** ### **Acute** IV **calcium gluconate** ### **Chronic** * Oral calcium * Calcitriol --- # **CALCIUM GLUCONATE** | Parameter | Value | | ------------ | -------------------- | | Indication | Acute tetany | | Mechanism | Raises serum Ca | | Dose | 10 ml of 10% IV slow | | Side effects | Arrhythmia | | Monitoring | ECG | --- # **CALCITRIOL (Vitamin D)** | Feature | Detail | | ------------ | -------------------------- | | Action | ↑ Intestinal Ca absorption | | Dose | 0.25–1 mcg/day | | Side effects | Hypercalcemia | | Monitoring | Serum Ca | --- # **PSEUDOHYPOPARATHYROIDISM** ## **Definition** Target organ resistance to PTH | Ca | PTH | Phosphate | | -- | --- | --------- | | ↓ | ↑ | ↑ | ## **Clinical** * Short stature * Round face * Brachydactyly * Mental retardation **Treatment:** Calcium + Vitamin D --- # **PARATHYROID CRISIS** Severe hypercalcemia (>14 mg/dL) ### **Features** * Dehydration * Arrhythmia * Coma ### **Management** 1. IV saline 2. Loop diuretic 3. Calcitonin 4. Bisphosphonates 5. Dialysis if refractory --- # **EXAM PEARLS** | Scenario | Diagnosis | | --------------------------------- | --------------------------- | | High Ca + high PTH | Primary hyperparathyroidism | | Low Ca + high PTH | Secondary HPT | | Low Ca + low PTH | Hypoparathyroidism | | Low Ca + high PTH + short fingers | Pseudohypoparathyroidism | ---
Comments & Discussion
Use this thread like a mini viva: add differentials, staging systems, drug regimens and exam tricks.
Login or register to comment.
No comments yet – start by adding exam-style discussion points.